MOJ
eISSN: 2379-6162


Review Article Volume 9 Issue 2
1General Surgery, Eastern Health, Australia
2Monash University Eastern Health Clinical School, Australia
Correspondence: Janindu Goonawardena, General Surgery, Eastern Health, Box Hill, Victoria 3128, Australia, Tel +613 98953281,
Received: March 15, 2021 | Published: March 26, 2021
Citation: Goonawardena J, Jain A, Cheung KT, et al. Is cavity packing following cutaneous abscess drainage necessary? A systematic review and meta-analysis. MOJ Surg. 2021;9(2):40-47. DOI: 10.15406/mojs.2021.09.00190
Background: This meta-analysis aims to analyze the difference in outcome between a packed group (PG) and a non-packed group (NPG) of patients post drainage of simple cutaneous abscesses.
Methods: A systematic review of patients who underwent incision and drainage of simple cutaneous abscesses with packing or no packing was performed. The meta-analysis was performed using Mantel–Haeszel method.
Results: 217 patients from four studies were included. Overall no significant difference was observed in the primary outcome of recurrence of abscess post drainage in the PG compared to the NPG (RR 2.34, 95% CI 0.90, 6.10) with no heterogeneity between studies (I2=0%, P=0.08). Subgroup analysis involving three studies showed no significant difference in abscess recurrence risk between the PG and the NPG in the pediatric population (RR [95% CI]:2.23[0.77,6.47]). Quality assessment demonstrated all three RCTs were low-quality with an overall high-risk of bias.
Conclusion: Based on the limited number of low-quality small studies, there is data to support elimination of routine cavity packing post drainage in immunocompetent pediatric patients. There is a clear paucity of evidence in the adult population regarding utility of continuous packing.
Keywords: packing, incision, drainage, skin abscess, meta-analysis
PG, packed group; NPG, non-packed group; RCT, randomized controlled trials; RR, relative risk.
A cutaneous abscess is a localized collection of necrotic tissue with pus resulting from the disintegration of tissue in the dermis and deeper skin tissues due to inflammatory cell infiltration, commonly in response to a bacterial infection.1 Abscesses are thought to begin as superficial cellulitis that leads to cell liquefaction and debris collection in the dermis with subsequent loculation, leading to formation of collections of pus.1 Traditional management of cutaneous abscess involves incision and drainage, curettage, and packing of the residual cavity.2–4 The rationale for cavity packing is to prevent incomplete collapse of the cavity with infected material trapped inside it and to assist in development of an epithelial lining in the cavity, allowing healing by secondary intention.4,5 This routine practice of postoperative continuous packing simple cutaneous abscesses has been based on traditional teaching, with limited evidence, justification or benefit.4,6,7 Ongoing packing has considerable ramifications for both the patient and healthcare system alike. It can cause significant discomfort and pain to the patient, requires multiple visits to medical practitioners, increased inconvenience and expense.7,8 Home visiting nurses organized by hospitals augment the financial burden of the healthcare system. Lastly, with continuous packing, cavities may have delayed shrinkage, resulting in healing time.5
A Cochrane review performed by Smith et al.,8 evaluating postoperative continuous cavity packing for perianal abscesses showed no clear difference in abscess recurrences and development of fistulae between packed group (PG) and non-packed group (NPG). In addition, the current guidance from The American Society of Colon and Rectal Surgeons suggests that with an adequately sized incision, postoperative wound packing is usually not necessary.9 Few previous studies4,5,10,11 with variable quality have evaluated outcomes with postoperative packing for simple cutaneous abscesses. There has been no previous systematic review or meta-analysis investigating this cohort of patients. We aim to analyze the difference in outcome between packing and no packing post drainage for patients with simple cutaneous abscesses.
Protocol
This systematic review was conducted according to the guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).
Eligibility criteria
Inclusion criteria for this review were studies evaluating patients of all ages who had a cutaneous abscess treated surgically with incision and drainage and comparing postoperative packing versus no packing. All randomized controlled trials (RCTs) and non-randomized studies were included. All studies published in English language from January 1990 to June 2020 were included in this review. Editorial comments, case reports, reviews, meta-analyses and studies comparing other types of abscesses were excluded.
Search strategy
Three authors (JG, AJ, KC) performed the systematic search through PubMed, Scopus and Cochrane library on 14 July 2020. For the literature search in PubMed, the following MeSH terms ‘abscess’, ‘skin’, ‘drainage’ and non-MeSH term ‘packing’ were used. The following INDEXTERMS were used in Scopus; ‘abscess’, ‘skin’, ‘drainage’, ‘packing’. The three investigators screened publication titles and abstracts independently. Duplicate studies were excluded. Discrepancies between the three investigators were resolved following discussion with the fourth investigator (RC). Full-text articles were then reviewed.
Data extraction and methodological quality
The following data were extracted from the selected studies: the authors, year of publication, country of origin, type of study, study setting, proceduralist, type of anaesthesia, method of randomization, number of participants, study population, surgical method, intervention, follow up period and power analysis. Three authors (JG, AJ, KC) performed an independent quality assessment of each included RCT based on Cochrane risk of bias tool (RoB2).
Outcome measurement
The primary outcome measured included abscess recurrence, defined as requiring repeat incision and drainage, any additional postoperative intervention such as extension of previous incision, further probing and breaking up loculations and irrigation. Secondary outcomes measured included postoperative pain, time to wound healing and number of presentations.
Statistical analysis
The meta-analysis was performed using the Mantel–Haenszel method for calculating the weighted pooled relative risks using a fixed effects model based on the study heterogeneity. The statistical heterogeneity among studies was evaluated using I2 statistics and P values using STATA 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). The heterogeneity was considered significant at I2>50% or P<0.05. Relative risks with 95% confidence intervals were used. P values were two-sided with a significance of less than 5% i.e. p value<0.05. The publication bias of the studies included was explored by visual inspection of its funnel plot.
The literature search identified a total of 205 articles, out of which twenty-six articles were read completely. Having excluded twenty-two articles, four were included in the systematic review and meta-analysis Figure 1. The four studies evaluated a total of 217 patients, with 112 in the packed group (PG) and 105 in the non-packed group (NPG) Table 1. Three of studies were RCTs4,5,11 and one was a cohort study.10 Three studies were performed on a pediatric population5,10,11 and one study performed in the adult population.4 Two studies were performed in emergency department setting by physicians4,5 and two were performed in theater by surgeons.10, 11
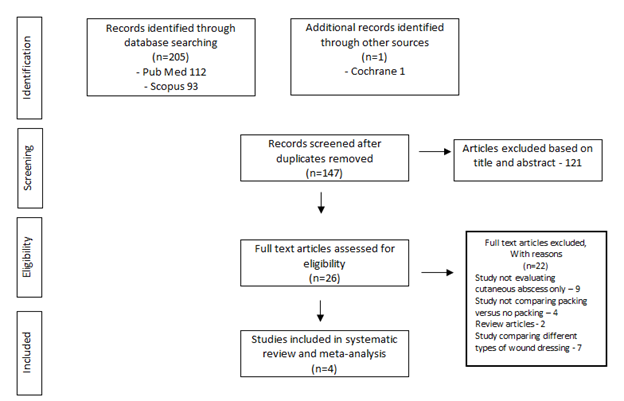
Figure 1 Flow diagram showing identification of studies for inclusion in this systematic review according to PRISMA guidelines.
|
Author, |
Study type |
Study setting |
Type of anaesthesia / analgesia |
Number of patients |
Median age |
Abscess type and size |
Surgical method |
Intervention |
Follow up period |
|
Year, |
Proceduralist |
Years |
|||||||
|
Country |
|||||||||
|
Kessler et al.5 |
RCT |
Emergency department by physician |
At the discretion of physician |
49 |
PG: 6.0 |
Cutaneous and no size restriction |
Linear incision using scalpel at least 75% of wound diameter and then fully draining and exploration wound for loculations |
PG: gause packing removed 48 hours post procedure |
1 month |
|
PG:27 |
NPG: 6.0 |
NPG: no intraoperative packing post drainage |
|||||||
|
NPG: 22 |
|||||||||
|
Koehler et al.10 |
Cohort |
Theater by surgeon |
General anaesthesia, sedation, local anaesthesia |
35 |
PG: 5.3 |
Cutaneous and < 5cm |
wide incision over abscess cavity sufficient to drain pus, explore cavity and breakdown loculations |
PG: gause packing continued >two times a day postoperatively until wound healed |
3 months |
|
PG: 19 |
NPG: 8.4 |
NPG: gause packing removed 24 hours post procedure |
|||||||
|
NPG: 16 |
|||||||||
|
Leinwand et al.11 |
RCT |
Theater by surgeon |
Intravenous sedation and local anaesthesia |
85 |
PG: 5.7 |
Cutaneous and no size restriction |
5-8mm incision made in the center of fluctuant area, regardless of the size of the abscess |
PG: gause packing removed 24 hours post procedure |
30 days |
|
PG: 43 |
NPG: 4.6 |
NPG: no intraoperative packing post drainage |
|||||||
|
NPG: 42 |
|||||||||
|
O’Malley et al.4 |
RCT |
Emergency department by physician |
local anaesthesia only |
48 |
PG: 29.7 |
Cutaneous and < 5cm |
Incision with scalpel, cotton tipped applicator to break loculations, irrigation with saline |
PG: gause packing removed 48 hours post procedure |
15 days |
|
PG: 23 |
NPG: 30.5 |
NPG: no intraoperative packing post drainage |
|||||||
|
NPG: 25 |
|||||||||
Table 1 Study, patient characteristics, follow up of all included studies comparing packed group versus non-packed group post drainage of cutaneous abscesses
NPG, non-packed group of patients; PG, packed group of patients; RCT, randomised controlled trial; USA, United States America
This meta-analysis revealed no significant difference in the primary outcome of abscess recurrence post drainage in the PG compared to the NPG for simple cutaneous abscesses, in the fixed effects model (Relative risk (RR) [95% confidence interval (CI)]: 2.34 [0.90, 6.10]) with no heterogeneity between studies (I2=0%, P=0.08) Figure 2. Visual symmetry of the funnel plot suggests no publication bias for the four studies included in the meta-analysis Figure 3.
Subgroup analysis showed no significant difference in the recurrence risk between the PG and the NPG in the pediatric population (RR [95% CI]: 2.23 [0.77, 6.47]), with no heterogeneity between the three studies (I2=0%, p=0.14) Figure 4. The risk of recurrence was not significantly different between the PG and the NPG in the emergency department (RR [95% CI]: 2.54 [0.84, 7.64]) and operating theater setting (RR [95% CI]: 1.82 [0.25, 13.07]). No heterogeneity was detected within either of the two subgroups (I2=0%, p=0.93; I2=0%, p=0.56, respectively) Figure 5.
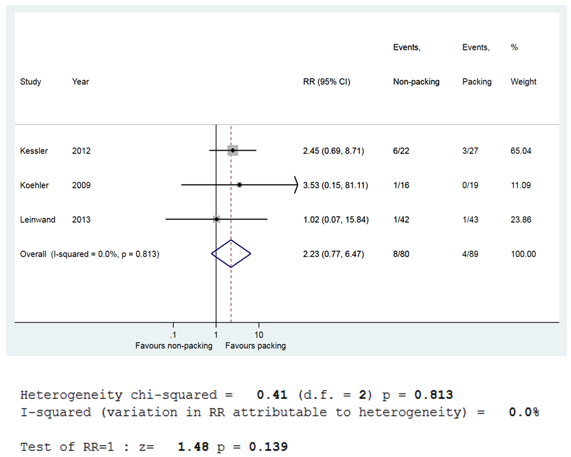
Figure 4 Forest plot showing relative risk of abscess recurrence between PG and NPG; paediatric population.
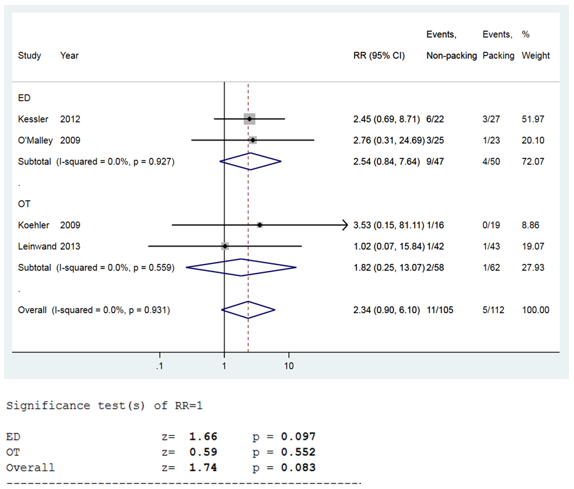
Figure 5 Forest plot showing relative risk of abscess recurrence between PG and NPG; emergency versus operating theatre.
Out of the three secondary outcomes Table 2, post procedure pain was assessed in three4,5,10 out of the four studies, two of which showed greater pain immediately post procedure and within 48 hours in the PG compared to the NPG.4,10 Wound healing was only assessed in one study,5 which showed no difference in the PG compared to the NPG. A statistical power analysis was performed in the three studies, revealing that two studies failed to have enough participants included and the other was not of adequate power. The quality assessment of the three RCTs based on Cochrane risk of bias tool (RoB2) demonstrated all three studies were of low quality with an overall high risk of bias4,5,11 Table 3. Measurement of the outcome was one of the domains that were assessed most poorly, along with missing outcome data and deviation from intended intervention.
|
Author, |
Statistical power analysis |
Primary outcome |
Secondary outcome |
Secondary outcome |
Secondary outcome |
|
Year, |
(Reoccurence of abscess / total) |
Postoperative pain |
Wound healing |
Number of representations |
|
|
Country |
|||||
|
Kessler et al.5 |
Performed, |
PG: 3 / 27* |
NS immediately post procedure and 48 hours post procedure |
NS |
NS |
|
but number of participants didn’t meet requirement |
NPG: 6 / 22 |
||||
|
Koehler et al.10 |
Performed, |
PG: 0/ 19 |
PG greater pain the next day compared to NPG |
NA |
PG higher representations compared to NPG |
|
but low power study |
NPG: 1/16 |
||||
|
Leinwand et al.11 |
Performed, |
PG: 1/ 43 |
NA |
NA |
NA |
|
but number of participants didn’t meet requirement |
NPG: 1/ 42 |
||||
|
O’Malley et al.4 |
NA |
PG: 1 / 23 |
PG higher pain scores immediately post procedure and 48 post procedure |
NA |
NA |
|
NPG: 3 /25 |
|||||
Table 2 Primary and secondary outcomes of included studies comparing packed group versus non-packed group post drainage of cutaneous abscesses
NA, not assessed; NPG, non-packed group of patients; NS, no statistically significant difference between packed versus non-packed group; PG, packed group of patients; USA, United States America
*statistically significant number of patients (8) continued cavity packing post initial assessment
The cornerstone of management of cutaneous abscesses involves adequate incision and drainage of pus, breakdown loculations and copious wound irrigation. Packing the abscess cavity immediately postoperatively with gauze has been commonly practiced for surgical haemostasis. In certain instances, it prevents early closure of the wound, depending on the timing of subsequent patient review. Kessler et al.,5 also argued that some packing material could impede drainage and promote infection through tissue damage. Continuous cavity packing for cutaneous abscesses remains controversial and is largely based on proceduralist preference with no standardised protocol. This review certainly highlights the paucity of evidence on this dilemma, despite it being a very common presentation in clinical practice. This meta-analysis showed no difference in recurrence between the PG and the NPG for cutaneous abscess, with the systematic review indicating an overall low quality of evidence. These results are consistent with the findings of two previous reviews supporting elimination of packing post drainage.6,7
Study setting and population
Two studies were performed in the emergency department by physicians with minimal anaesthesia,4,5 compared to the other two studies performed in theater by surgeons with general anaesthesia or sedation.10,11 The subgroup analysis showed no difference between these two settings. However, in clinical practice the size, location of the abscess and the tolerability of the patient to withstand the procedure needs to be considered as adequate initial abscess drainage is of paramount importance to prevent recurrence. A low threshold for surgeon involvement should be considered. All four studies were performed in the United States of America. The majority of these trials involved a pediatric population, in which the postoperative management would differ in clinical practice compared to the adult population, with limited tendency for postoperative packing of abscesses in children. The subgroup analysis showed no difference in the PG versus the NPG for the pediatric population, justifying hesitancy towards post-procedure packing. It also important to realize that in all four of the studies immunosuppressed patients were excluded. Hence, these findings could be only applied to immunocompetent patients.
Surgical method
An interesting multicenter survey by Schmitzet et al.,12 involving emergency physicians in fifteen centres across the United States depicted the breadth of variability in the surgical management cutaneous abscesses. Intraoperative surgical method does play a role in determining adequate of drainage of pus and hence impacts primary and secondary outcomes in these patients. All four studies made incisions over the abscess with scalpel, only two studies specified the size of incision,5,11 and only one study mentioned the type of incision which was linear.5 Interestingly, early trials performed by Sørensenet et al.,13 showed that linear incisions plus curettage had a significantly shorter healing time compared to deroofing and drainage, even though the results were not statistically significant. Two studies performed irrigation,4,11 whilst the other two studies did not mention irrigation following drainage.5,10 Given no standardised protocol for incision and drainage in the analyzed studies and multiple proceduralists performing these procedures within the same cohort of patients, this could lead to confounding outcomes and limit the quality of the study.
Post drainage packing versus no packing
Post drainage packing protocols also differed amongst the studies. Three studies in the PG had intraoperative packing with gauze, which was removed within 48 hours and the NPG had no intraoperative packing.4,5,11 This was in comparison to Koehler et al.,10 in which the PG had continuous daily packing and the NPG had gauze packing removed within 24 hours. In current surgical practice, it remains quite common to always pack the cavity with gauze or haemostatic coated dressing for the sole purpose of haemostasis and then remove it within 24 hours. Subsequently, in an adult population, whether a patient has continuous cavity packing or a simple absorbent dressing without cavity packing is based on variety of factors. This includes the size and type of initial incision, adequacy of drainage, cavity size, proceduralist preference, patient factors such as comorbidities, compliance, willingness and ability to tolerate dressings changes, access to dressings, availability of caregivers or visiting nurses to provide postoperative wound care and their social situation. If there is no observable difference in recurrence of abscess between the PG versus the NPG, and possibly more postoperative pain is demonstrated in the PG, an argument could be made for elimination of cavity packing post drainage. Furthermore, patients who were in the PG had their packing removed within 48 hours and subsequently did not have any packing. Despite this, they failed to demonstrate a difference in recurrence, thereby corroborating the limited benefit of continuous cavity packing. It is likely that the most important determinant would be the extent of initial drainage and the size of initial incision compared to the size of the abscess cavity.
Quality assessment
The quality assessment of the three RCTs demonstrated that all three studies were of low quality with an overall high risk of bias.4,5,11 The randomization process and reporting of measured outcomes were the two best reported domains in two of the studies.4,5 One of the contributing factors for the low quality across all three studies was the fact that even though the initial postoperative assessment was carried out by the clinician, the subsequent assessment was determined via phone consultation with the patient, introducing measurement bias. All three studies failed to avoid attrition bias due to missing outcome data.4,5,11 In Kessler et al.,5 there was a significant difference between groups post intervention, in which eight patients in the PG compared to one patient in the NPG underwent subsequent packing following the initial postoperative review. Hence, these deviations from intended treatment varied between the two groups and are likely to have affected the outcome. Koehler et al.,10 was not included in the RoB2 tool as it was a cohort study. This study was also structured poorly as the comparison PG was based on historical controls from twelve-month period in the previous year.
Strengths and limitations
Strength of this review is that it is the first systematic review and meta-analysis evaluating difference in outcome between packing and no packing for patients post drainage of simple cutaneous abscesses. It analyzes the study setting, population, surgical method, difference in intervention and how this affects clinical practice. It demonstrates the paucity of evidence in an adult population evaluating the utility of continuous packing. It also highlights the lack of focus on secondary outcome measurements in included studies. Limitations of the review include the small number of total patients included in the meta-analysis, which might prevent detecting a small difference between the groups. There is limited generalizability and applicability of the findings to the adult population given that there was only one study in this population included in the review. There is also no uniformity in the assessment of secondary outcomes such as postoperative pain, due to the inconsistencies in the included studies of examining these variables.
Recommendations
Based on this review, we recommend performing a multicenter RCT in an adult population with postoperative continuous abscess cavity packing in a PG versus no continuous cavity packing in a NPG in the postoperative period. This trial is currently in progress at our institution. It is paramount that independent clinicians examine wounds in follow up visits. More focus should be based on important secondary outcomes such as time taken to return to work and normal function, costs and resource utilization (e.g. number of visits by nurses and dressings changes). If validated, elimination of the common practice of continuous cavity packing post drainage could be economically favorable to the already burdened health system.
Management of cutaneous abscess requires adequate incision, drainage and irrigation of the wound. Based on the limited number of small studies with low quality, there is data to support elimination of routine cavity packing post drainage in immunocompetent pediatric patients. There is a clear paucity of evidence in the adult population regarding the utility of continuous packing. Multicenter RCTs in the adult population focusing not only on abscess but also on patient-centered outcomes such as return to work and institutional cost differences would be beneficial in facilitating evidence-based treatments.
None.
None.
Then authors declare that they have no conflicts of interest.

©2021 Goonawardena, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.