MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 3
1General surgery, Spanish Hospital of Mexico City, Mexico
2General Surgery Resident, Spanish Hospital of Mexico City, Mexico
Correspondence: Gallardo Navarro Elias, Mexican National Army 613, Granada, Miguel Hidalgo, 11520 Mexico City, CDMX, Tel 22276429 45
Received: August 28, 2024 | Published: September 12, 2024
Citation: Emmanuel XXC, Natalie SL, Pedroza EN, et al. Intestinal occlusion secondary to De Garengeot’s hernia resolved by laparoscopy. MOJ Surg. 2024;12(3):93-95. DOI: 10.15406/mojs.2024.12.00270
Introduction: Femoral hernias constitute a minority of abdominal wall hernias and an entrapment of the appendix in the femoral hernia is called Garengeot's hernia.
Case report: A 93-year-old woman was admitted to the emergency department of our hospital presenting abdominal pain accompanied by intestinal occlusion. She underwent laparoscopy for a diagnosis of femoral hernia with inflamed cecal appendix inside, with an adequate postoperative period.
Discussion: The incidence of De Garengeot hernia is approximately 0.1-5% of reported femoral hernias and 0.1% of acute appendicitis.
Conclusion: Despite this uncommon pathology, emergency surgical treatment is generally required, and the laparoscopic approach is the best option as long as the patient's condition and the surgeon's experience allow it.
Keywords: cecal appendix, garengeot's hernia, laparoscopy, abdominal pain, appendicitis, femoral hernia
Incarceration of the appendix within a femoral hernia is a rare condition of abdominal wall hernia about 0.1 to 0.5% in reported femoral hernia.1–3 A cecal appendix within a femoral hernia is a rare pathology, it was described by René Jacques Croissant de Garengeot more than 250 years ago, who reported for the first time this pathology in a 55 year old woman who developed this disease after lifting weights, nowadays it is still surprising to observe this pathology intraoperatively, the contribution on this subject of Rene Jacques Croissant De Garengeot in 1668-1759, parisian surgeon of the XVIII century linked to the Académie Royale de Chirurgie.4–6 In 1735, Claudius Amyand (1660–1735), a surgeon in England, performed the first successful appendectomy on an 11-year-old boy with a perforated, acutely inflamed appendix within the right scrotal sac.3,7 This eponym should be used to describe the incarceration of the vermiform appendix within a femoral sac, the rate of incarceration in femoral hernias, is higher than inguinal hernias, due to the narrow space of the defect and the stiffness of the femoral canal. Therefore, when it is diagnosed, it must be submitted to surgical procedure due to the high risk of incarceration that occurs up to 14 - 56 %, the clinic is an irreducible inguinal protrusion, painful, with inflammatory signs and acute abdomen.4,8–10
Factors contributing to the increased incidence of abdominal complications are delayed diagnosis, poor nutritional status, perforation, among other comorbidities, and other predisposing factors to this condition include a certain degree of intestinal malrotation as well as the presence of an abnormally long and mobile cecum with extension into the pelvis. We present the clinical case of a patient with incarcerated right femoral hernia appendicitis and successful management with laparoscopic appendectomy and laparoscopic inguinal plasty with primary closure.5,10–12
A 93-year-old woman presented to the emergency department with a 1-day history of right lower quadrant abdominal pain that moved into the right groin area. On physical examination, presented with left lower quadrant pain, decreased peristaltic sounds and abdominal distension. Laboratory data demonstrated leukocytosis. Abdominal computed tomography showed an incarcerated right femoral hernia of the appendix with dilatation of the appendix (Figure 1 & 2). She underwent laparoscopic surgery where an incarcerated colon was observed in the internal ring of the right femoral canal (Figure 3 & 4). Appendectomy was performed after reduction (Figure 5). The right femoral hernia of the internal ring was closed with a primary suture (Figure 6 & 7). Pathologic anatomy revealed appendicitis with reactive lymphoid aggregates. From the beginning he was treated with antibiotics, and adequate parenteral fluid management. The postoperative period was adequate, she did not present abdominal symptoms such as pain or nausea. She was discharged 4 days after a successful appendectomy and hernia repair.

Figure 1 Tomography of the abdomen in coronal section , distended bowel loops secondary to right femoral hernia.
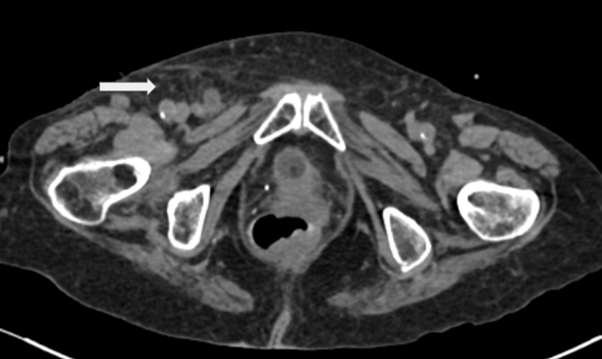
Figure 2 Tomography of the abdomen in axial section, showing right femoral hernia with intestinal content.
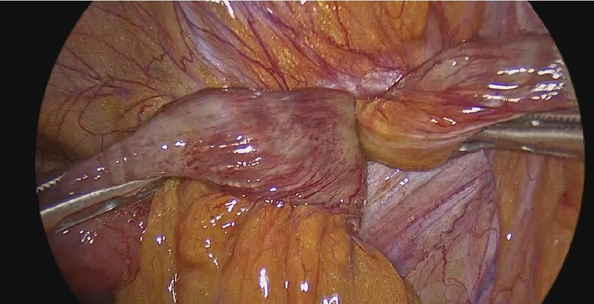
Figure 3 Colon is observed in femoral hernia without macroscopic data of intestinal ischemia or peritonitis.
The medical approach to diagnose this pathology is to recognize and provide timely treatment to reduce complications that may contribute to a poor outcome, abdominal pain, accompanied by signs and symptoms of intestinal occlusion can support the diagnosis along with imaging studies that guide the surgeon to rule out other pathologies.6,13,14 Differential diagnosis should include other types of femoral hernia, such as Cloquet hernia and Serafini hernia, inguinal hernia, infected or necrotic lymphadenopathy, ectasia of the vena saphena megna, lipomas or other soft tissue tumors and hypostatic abscesses in retroperitoneal processes.15,16 Takemuraet first reported De Garengeot's hernia before surgery on CT, which provides a direct view of the appendix in the femoral area, ultrasound was also useful to make this diagnosis, however the diagnosis in most of the times is made intraoperatively.17,18 Despite the low sensitivity of abdominal CT in the preoperative diagnosis of De Garengeot's hernia (61%), it offers a better investigation of the abdominal cavity, a lower rate of complications and a better length of hospital stay, especially winning the case of infection or signs of peritonism.16,19 Guenther described a classification for De Garengeot's hernia and it can be used for surgical treatment that includes a laparoscopic approach or an open approach, the laparoscopic approach is the best option, especially if the diagnosis is made preoperatively, since it offers the advantages of laparoscopy, the open approach is a valid option when the laparoscopic surgical skill is not available or the laparoscopic equipment is not available, the use of mesh is recommended in the literature in case there is no peritonitis or abscess, otherwise the risk of infection or recurrence of the hernia increases.8,10,19
Surgical resolution should not be delayed, since acute appendicitis and intestinal perforation may occur due to the obstructive component.2 According to some authors and in the literature, if the appendix is normal appendectomy is not required, while if it is inflamed it is necessary to do it inside the hernial sac, other authors consider that even if the appendix does not reveal macroscopic signs of inflammation, a regular appendectomy should be performed in all cases, because microscopic signs of inflammation caused by compression and ischemia of the hernial neck cannot be ruled out, a regular appendectomy should be performed in all cases, because microscopic signs of inflammation caused by compression and ischemia of the hernial neck cannot be ruled out, in our case appendectomy was performed with the result of the pathology service confirming appendicitis.3,17s,18 Reports in the literature, such as that of Alessio Rollo and McLaughlin, are similar in the clinical presentation of the patient and the surgical treatment to that performed by us.20,21 The surgeon must be aware of the unusual forms of abdominal wall hernia, as there are variants such as this case, which must be taken into account as a differential diagnosis.19
Despite this uncommon pathology, emergency surgical treatment is generally required, and the laparoscopic approach is the best option as long as the patient's condition and the surgeon's experience allow it. The use of prosthetic mesh is still debated, due to the risk of infection or recurrence of the hernia.
None.
The authors declare that there no conflicts of interest.

©2024 Emmanuel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.