MOJ
eISSN: 2379-6162


Research Article Volume 11 Issue 2
Moreno Valle Trauma and Orthopedic Hospital, University Hospital of Puebla, Mexico, Hospital: Mexican Red
Correspondence: Dr. Rogelio Zayas Borquez Address: Av. De los cipreses, col barreal, san andres cholula, puebla, Mexico, Tel 66 21 96 42 59
Received: June 20, 2023 | Published: July 4, 2023
Citation: Bórquez RZ, Lozano DT, Minero JCV, et al. How to recognize a dying patient? Acute traumatic coagulopathy: experience in a level I trauma center. MOJ Surg. 2023;11(2):87-91. DOI: 10.15406/mojs.2023.11.00229
Background: It is possible to detect abnormal clotting parameters in 25-35% of injured patients at their arrival to the hospital, which are proportional to the severity of the injuries and associate with higher morbimortality rates.
Objectives: Therefore, it arises the question whether the results of conventional laboratory tests carried out while monitoring the injured patient may be used as early available predictors. Methods: We conducted a prospective, descriptive and observational multivariable study at the Central Hospital of the Mexican Red Cross to determine the correlation between the alterations in the results of clotting tests obtained at the time of hospital admission of the patient and the likelihood of emergency surgery necessity or death within the first 48 hours of hospital stay.
Results: We included 327 patients, between 1-92 years old, 20.79% patients were admitted with ATC criteria, 40.36% required emergency surgery (54.41% in the context of ATC) and 18.65% died (10.39% of them during or after the surgical management, and 47.05% with ATC criteria).
Conclusions: According with our results conventional clotting tests are quite sensitive tools for identifying patients at high risk of early death and good predictors of poor outcomes in the treatment.
Keywords: coagulopathy, trauma, clotting tests
TTP, partial thromboplastin time, TP, thrombin time, INR, international normalized ratio; ATC, trauma-associated coagulopathy
Trauma is one of the leading causes (10%) of death and disability in patients aged 5 to 44 worldwide, while hemorrhage, responsible for 30-50% of deaths within the first 48 hours after hospital admission is the primary preventable cause of mortality in these patients (16%).1 Blood loss can result in early. This coagulopathy occurs immediately after trauma—before any therapeutic intervention—in up to 56% of cases.2–12 It is now known that these hemostatic abnormalities are directly proportional to the severity of injuries (especially traumatic brain injury) and the degree of tissue hypoperfusion. Patients who develop these abnormalities have significantly higher mortality rates (37%) and a higher incidence of complications (30% vs. 12%).1,2,8–10,12,14–16 such as multiple organ failure, infections, increased transfusion requirements, longer resuscitation periods, and they also increase the risk of exacerbating subsequent medical interventions.1–3,6,7,14–25 Therefore, early detection of acute traumatic coagulopathy (ATC), coupled with adequate and aggressive resuscitation, has been proposed to be associated with a significant reduction in morbidity and mortality.2,7,8,13–15,18,20,26,27
ATC is a state of hypocoagulation observed in injured patients and is defined by the presence of clinical signs of active bleeding (e.g., visible non-surgical bleeding, tachysphygmia, hypotension) and/or laboratory evidence of coagulation disorders (e.g., partial thromboplastin time [PTT] >34 seconds or >1.6x normal, prothrombin time [PT] >14 seconds or <70%, international normalized ratio [INR] ≥1.5, platelet count [PLT] <100,000/mL) at the time of hospital admission.1,3,11,13,19,28,29 However, the pathophysiology of ATC is a complex and multifactorial phenomenon that is only partially understood and continues to generate debate in the medical literature.5,13,17,18,8,9,13, 15,16,20,30–34
Considering the difficulty in characterizing the pathophysiology of ATC and the absence of clinical signs of hemorrhagic shock upon hospital admission in many injured patients due to idiosyncratic variables or prehospital volume expansion, the early assessment of the traumatized individual is complex, and complementary tests are often necessary to detect the presence of coagulopathy early on and make appropriate therapeutic decisions. For these reasons, the question arises as to whether hemostatic abnormalities detected during the monitoring of the injured patient can be used as early available prognostic variables.4,7,15,30,31,35
Determine the correlation between alterations in coagulation test results obtained at the time of patient hospital admission and the probability of requiring urgent surgical treatment or experiencing mortality within the first 48 hours.
This study was a prospective, descriptive, observational, multivariable study conducted at the Central Hospital of the Mexican Red Cross in Mexico City. Its objective was to determine the correlation between the presence of alterations in coagulation test results obtained at the time of patient hospital admission and the probability of requiring urgent surgical treatment or experiencing mortality within the first 48 hours of hospital stay. The study aimed to establish how reliable these tests are in making clinical decisions. All patients admitted to the hospital between January and June 2015, with an age range of 1 to 92 years, who were classified under the category of "trauma" as the reason for admission and received in the shock room, were included in the study based on one or more of the following institutional severity criteria:4,36
Physiological criteria
Respiratory rate <10 or >29 breaths per minute in adults, <20 breaths per minute in children Systolic blood pressure <89 mmHg
Glasgow Coma Scale score <14
Anatomical criteria
Unstable chest
Penetrating trauma to the head, neck, torso, or proximal extremities (above the elbow or knee) Pelvic fracture
Two or more fractures in long bones proximal to the wrist or ankle Exposed fracture with vascular compromise
Proximal amputation above the wrist or ankle Exposed or depressed skull fracture
Limb paralysis
Involvement of two or more organ systems
Kinematic criteria
Motor vehicle collision with speed >64 km/h Motorcycle collision with speed >32 km/h
Passenger without safety measures (seatbelt, helmet, etc.) Ejection from the vehicle
Passenger death in the same vehicle compartment
Vehicle deformation >50 cm
Intrusion into the passenger compartment >30 cm Vehicle extraction time >20 minutes
Pedestrian collision with speed >32 km/h
Fall from a height >6 m (in adults) or three times their height
Comorbidities (as additional data to consider): age <5 or >55 years, pregnancy >20 weeks, history of anticoagulation, end-stage renal failure. Patients who were admitted with a reason for admission other than "trauma" and those in whom complementary tests could not be obtained at the time of hospital admission were excluded from the study. To reduce the dispersion caused by the age range, the decision was made to separately describe three age groups (1-17 years, 18-49 years, and 50 years or older). Other variables such as comorbidities, medication intake, and alcohol and drug consumption were not taken into account. This decision was made because the study objectives were: 1) to determine how many patients received in the shock room met the paraclinical criteria for ATC (TTP >34 seconds, TP >14 seconds or <70%, INR ≥1.5, PLT <100,000/mL), and
2) how many of these patients required urgent surgical management (including "minor" procedures such as the insertion of an endopleural tube) or died within the first 48 hours of hospital stay. The aim was to describe the characteristics of injured patients received in a shock room under real conditions, considering that often the variables we did not take into account are unknown at the time of patient hospital admission due to altered neurological status and/or lack of a reliable informant.
The first age group included 17 patients, 12 males (70.58%) and 5 females (29.41%), aged 1 to 17 years (mean age of 14.52, median of 16, and mode of 16), with an evolution time of 20-90 minutes (mean of 32.94, median of 30, and mode of 30). The mechanisms of trauma included 7 (41.17%) assaults, 7 (41.17%) traffic accidents, and 3 (17.64%) falls. The majority of the main diagnoses, i.e., those that resulted in hospital stay of at least 8 hours, urgent surgical intervention, or death within the first 48 hours, were superficial injuries (47.05%) or related to cranioencephalic trauma (41.17%).
In this population, 6 patients (35.29%, Figure 1) met the criteria for traumatic coagulopathy (83.33% TTP, 66.66% PT, 16.66% INR, 16.66% PLT, and 16.66% met all criteria, Figure 2). Among them, 3 (50%) required urgent surgical management (figure 3), and there was one fatality (16.6%) within the first 48 hours (figure 4). It is worth mentioning that all surgeries and deaths within this group occurred in patients who presented with diagnostic criteria for traumatic coagulopathy.
The most frequently observed criteria for traumatic coagulopathy related to the need for urgent surgical intervention in this population were prolonged TTP and PT (100%, i.e., 50% of the total patients with traumatic coagulopathy in both cases), with epidural hematoma (2 males) and compartment syndrome in limbs (1 male) as the main diagnoses. The only patient who died (female) met only the criteria of prolonged TTP and PT, with the main diagnosis being epidural hematoma.
The second group included 260 patients, 219 males (84.23%) and 41 females (15.76%), aged 18 to 49 years (mean age of 30.61, median of 30, and mode of 35), with a time interval of 5 minutes to 14 hours from the moment of trauma to arrival at the hospital (mean of 54.07 minutes, median of 30, and mode of 30). The mechanisms of injury included 139 (53.46%) assaults, 78 (30%) traffic accidents, 42 (16.15%) falls, and one explosion (0.38%). The majority of the main diagnoses were superficial injuries (40.38%) or related to cranioencephalic trauma (20.38%) and thoracic trauma (12.69%).
Within this population, 47 patients (18.07%, Figure 1) met the criteria for traumatic coagulopathy (61.70% prolonged TTP, 73.34% prolonged PT, 10.63% elevated INR, and 6.38% decreased PLT; Figure 2). Among them, 112 patients (43.07%) required urgent surgical management (57.44% of them in the context of traumatic coagulopathy; Figure 3), and there were 39 fatalities (15%) within the first 48 hours (8.84% during or after surgical intervention and 42.55% with criteria for traumatic coagulopathy; Figure 4).
The most frequently observed criteria for traumatic coagulopathy related to the need for urgent surgical intervention in this group were prolonged PT (74.07%, i.e., 42.55% of the total patients with traumatic coagulopathy) and prolonged TTP (48.14%, i.e., 27.65% of patients with traumatic coagulopathy) in the presence of injuries related to thoracic trauma (33.33%), cranioencephalic trauma (22.22%), and abdominal trauma (14.81%) as the most common primary diagnoses, with a male predominance (4:1). Regarding deaths, the most frequently observed criteria for traumatic coagulopathy in this population were prolonged PT (90%, i.e., 38.29% of the total patients with traumatic coagulopathy) and prolonged TTP (60%, i.e., 25.53% of patients with traumatic coagulopathy) in the presence of injuries related to cranioencephalic trauma (65%) as the most common primary diagnosis, with a male predominance (4:1).
Lastly, the third group included 50 patients, 36 males (72%) and 14 females (28%), aged 50 years or older (mean age of 63.34, median of 58, and mode of 52). The time interval between the occurrence of trauma and hospital admission ranged from 10 minutes to 10 days (mean of 344.60 minutes, median of 30, and mode of 30). The mechanisms of injury included 23 (46%) traffic accidents, 18 (36%) falls, and 9 (18%) assaults. The majority of the main diagnoses were related to cranioencephalic trauma (40%) or superficial injuries (34%). Within this population, 14 patients (28%, Figure 1) met the criteria for traumatic coagulopathy (92.85% TTP, 85.71% TP, and 21.42% INR, Figure 2). Among them, 17 (34%) required urgent surgical intervention (42.85% in the context of traumatic coagulopathy, Figure 3), and 21 (42%) died within the first 48 hours (20% during or after surgical intervention and 71.42% with criteria for traumatic coagulopathy, Figure 4).

Figure 1 Trauma patients by age group admitted to the emergency department with and without laboratory criteria for trauma-associated coagulopathy (ATC).
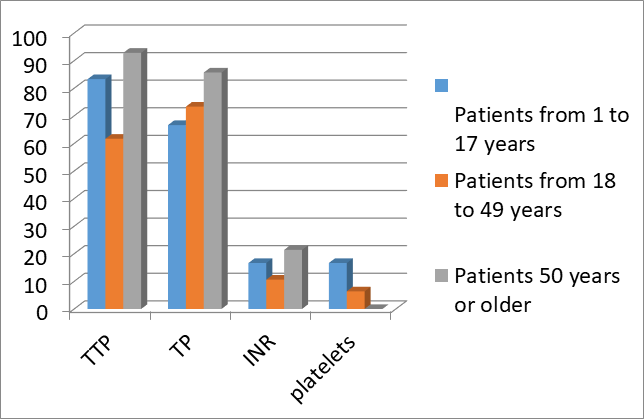
Figure 2 Laboratory criteria for trauma-associated coagulopathy observed in trauma patients admitted to the emergency department.
TTP: Partial Thromboplastin Time, TP: Thrombin Time, INR: International Normalized Ratio.

Figure 3 Trauma patients by age group admitted to the emergency department requiring urgent surgical management.
ATC: Trauma-Associated Coagulopathy.
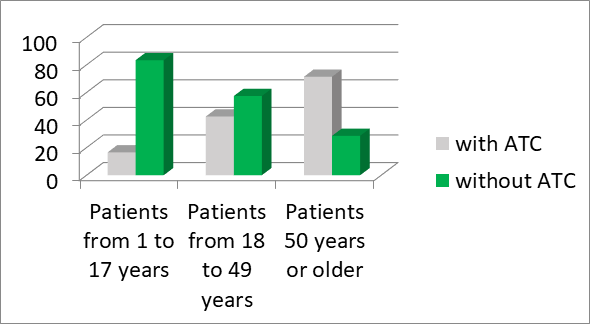
Figure 4 Trauma patients by age group admitted to the emergency department who died within the first 48 hours of hospital stay.
ATC: Trauma-Associated Coagulopathy.
The most frequently observed criteria for traumatic coagulopathy related to the need for urgent surgical intervention in this group were TP (74.07%, 42.55% of the total patients with traumatic coagulopathy) and TTP (48.14%, 27.65% of patients with traumatic coagulopathy) in the presence of injuries related to thoracic trauma (33.33%), cranioencephalic trauma (22.22%), and abdominal trauma (14.81%) as the most frequent primary diagnoses, with a predominance in males (4:1 ratio). Regarding fatalities, the most frequently observed criteria for traumatic coagulopathy in this population were TP (90%, 38.29% of the total patients with traumatic coagulopathy) and TTP (60%, 25.53% of patients with traumatic coagulopathy) in the presence of injuries related to cranioencephalic trauma (65%) as the most frequent primary diagnosis, with a predominance in males (4:1 ratio).
The study included 327 patients with a predominantly male population (4:1 ratio) - 267 males (81.65%) and 60 females (18.34%) - ranging from 1 to 92 years of age, with a mean age of 34.78, median of 32, and mode of 35. These figures align with those found in the literature, which demonstrate that more than half of the population affected by trauma is composed of working-age males.1–7,13,17–19,27–29,36,37
The time interval between the occurrence of trauma and hospital admission ranged from 5 minutes to ten days, with a mean of 91.77 minutes, median of 30, and mode of 30. This allows for two interesting observations: 1) thanks to the institutionalization of the concept of "the golden hour" and the implementation of new "scoop and run" transport protocols, an increasing number of severely injured patients arrive alive at emergency services (38), and 2) as a result, we can study a greater number of patients before any therapeutic intervention.1–5–12,15,19,26
Regarding the mechanisms of trauma, there were 155 cases (47.40%) of assaults (75 puncture wounds, 67 gunshot wounds, and 13 contusions), 108 cases (33.02%) of traffic accidents (56 pedestrian accidents, 40 collisions, and 12 motorcycle skids), 63 cases (19.26%) of falls, and one case (0.30%) of an explosion. The majority of the main diagnoses were superficial injuries (39.75%) or trauma-related to cranioencephalic injuries (24.46%). We did not observe a correlation with the reviewed literature, which states that blunt trauma resulting from motor vehicle accidents predominates in the civilian population. However, these differences are not surprising considering that our hospital has always been known for receiving a large number of patients with injuries resulting from third-party aggression.38
Conventional coagulation tests serve as reference exams for the diagnosis of coagulopathy. However, when processed at 37°C in recalcified plasma obtained from blood samples, they overlook the physiological interactions between coagulation factors, red blood cells, and platelets. Furthermore, the delay in obtaining results (median time of 78 minutes, although in some places they can be available within 10 to 30 minutes) questions their utility in the context of acute bleeding. On the other hand, there is a current trend of making clinical decisions based on thromboelastography and thromboelastometry results. However, these studies also have limitations as they do not take into account responses from the vascular endothelium and their availability is scarce. Additionally, none of them have demonstrated statistically significant benefits for the management of traumatized patients.4,6 ,8,10,21,27,31,35,39–41 Several scoring scales have also been developed to assess the severity of injuries, but they often require complex calculations and inaccessible data at the time of primary evaluation of the injured patient (i.e., definitive radiological findings or surgical findings). Therefore, their utility is limited to population comparisons for epidemiological purposes. That is why we do not routinely use them in our hospital.24
When comparing the three studied groups, it is notable that there is a similar male-to-female ratio (2-5:1) and time elapsed between the occurrence of trauma and hospital admission (mode and median of 30 minutes). However, regarding the diagnostic criteria for ATC, there was less homogeneity. Nevertheless, it is clear that:
1) the laboratory tests that showed more frequent abnormalities in all three groups were TTP (61.70-92.85%) and PT (66.66-85.71%); 2) the abnormal laboratory findings related to the need for urgent surgical intervention that were more frequently observed in all three groups were TTP (48.14-100%) and PT (74.07-83.33%); and 3) the most common diagnoses associated with ATC were trauma-related to cranioencephalic injuries, chest trauma, and abdominal trauma.38
In this study, 68 patients (20.79%) met the criteria for ATC (69.11% TTP, 75% PT, 11.76% INR, 5.88% PLT, and 1.47% all parameters). Out of these, 132 patients (40.36%) required urgent surgical intervention, with 54.41% of them in the context of ATC. Additionally, there were 61 deaths (18.65%) within the first 48 hours, with 34 deaths (10.39%) occurring during or after surgical management and 32 deaths (47.05%) meeting the criteria for ATC. These figures are similar to those reported in the literature, which states that abnormal coagulation parameters can be detected in 25-35% of traumatized patients upon hospital admission, and those who develop them have significantly higher mortality (37%) and a higher incidence of complications (30% vs. 12%).2–4,6–13,16
TP (74.07-100%), and 3) the laboratory tests with frequently altered results detected in cases of death within the first 48 hours of hospital stay in all three groups were TTP (60-100%) and PT (80-100%). These observations are also similar to those described in the reviewed studies, which state that: 1) TTP and PT are the conventional laboratory tests that most frequently show abnormalities related to ATC, 2) while PT is prolonged in a larger number of patients, TTP appears to be more specific in predicting treatment outcomes as a better predictor of mortality, and 3) appropriate resuscitation of traumatic hemorrhagic shock allows for early correction of PT and TTP levels through the administration of procoagulant factors, which could prevent or treat endothelial damage caused by direct inflammatory effects and, consequently, be associated with better treatment outcomes.6,7,10,11,18,24,29,35 Furthermore, a predominance of ATC criteria was also observed in patients with trauma-related cranioencephalic injuries, which is consistent with the findings in the consulted literature.1,12–14
Conventional coagulation tests are often underestimated as predictors of the need for urgent surgical management and mortality within the first 48 hours of hospital stay in trauma patients, as none of them provide a definitive indication of imminent coagulation disorders. However, it appears that: 1) they are quite sensitive tools for identifying patients at high risk of early death and also good predictors of poor treatment outcomes (especially true for PT and TTP, although they lack specificity), 2) the frequency with which they are requested and evaluated can be combined with clinical judgment to identify coagulation disorders in severely injured patients, and 3) they are inexpensive and their results are rapidly available in most emergency departments.
Nevertheless, there is an area where we agree with the majority of researchers: whether we are discussing conventional coagulation tests or thromboelastography/-metry, further validation of these tools is necessary to ensure their targeted, efficient, and cost-effective use. It is clear that there is still a need to compare the results obtained with thromboelastography/-metry (the current gold standards for detecting coagulation disorders) in order to assign a numerical value to their reliability as screening tests. However, the limited availability of these studies restricts their role in the evaluation of our findings.
None.
The authors had no conflicts of interest during the conduct of this study.
The study did not require any funding.

©2023 Bórquez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.