MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 3
1General Surgeon, Universidad Pontificia Bolivariana, Colombia
2Oncologic Surgery Service, Instituto de Cancerología - Clínica las Américas Auna, Colombia
3General Surgery Resident, Universidad Militar Nueva Granada, Colombia
4General Surgery Resident, Universidad CES, Colombia
5General doctor, Universidad CES, Medellín, Colombia
Correspondence: Julián Jaramillo Martinez, Oncologic Surgery Service, Instituto de Cancerología - Clínica las Américas Auna, Medellín, Colombia
Received: October 25, 2024 | Published: November 7, 2024
Citation: Gómez EI, Polonia LCA, Martinez JJ, et al. Chyloperitoneum induced by radiotherapy: case report and review of the literature. MOJ Surgery. 2024;12(3):113-115. DOI: 10.15406/mojs.2024.12.00275
Chylous ascites, also known as chyloperitoneum, is an uncommon condition with an incidence ranging from 1 in 20,000 to 1 in 187,000 patients. It is characterized by the presence of chyle in the abdominal cavity. Its etiology is often multifactorial, with abdominal trauma being the most common cause. Atraumatic causes, though less frequent, often arise from malignancies or lymphatic disorders. Radiotherapy-induced chyloperitoneum is even rarer, with an incidence of less than 3%. Diagnostic imaging, such as ultrasound and computed tomography (CT), as well as ascitic fluid analysis, showing triglyceride concentrations greater than 200 mg/dL, are essential for diagnosis. Treatment is generally multifactorial, involving parenteral nutrition, paracentesis, medication, and, in some cases, derivation or surgical procedures.
Keywords: acute abdomen, chyloperitoneum, colostomy, radiotherapy, peritonitis, fistula
Chylous ascites, or chyloperitoneum, is a rare condition characterized by the abnormal accumulation of chyle in the abdominal cavity. It is associated with lymphatic vessel obstruction or disruption, which impedes proper lymphatic drainage into the venous system. Although the etiologies of this condition are varied, traumatic causes are the most common, while atraumatic causes account for a smaller percentage, and radiotherapy is an even rarer cause In this report, we present a clinical case of a patient who developed chyloperitoneum following radiotherapy and brachytherapy, along with a brief discussion of its epidemiology, etiology, pathophysiology, diagnosis, and treatment.
A 38-year-old female patient with a medical history of hypertension, glucose intolerance, ischemic stroke and a moderately differentiated cervical adenocarcinoma in remission. She underwent radiotherapy (total dose of 5040 cGy) and concurrent chemotherapy four years prior, followed by brachytherapy (650 cGy in four applications) approximately two years ago. One month prior to her visit, she had a diverting colostomy due to contained peritonitis associated with radiation-induced proctitis. She presented to the emergency department with acute abdominal pain, abdominal distension, multiple emetic episodes, and absence of bowel movements through the colostomy. Laboratory tests revealed leukocytosis and neutrophilia, with a negative C-reactive protein (CRP). An MRI of the abdomen and pelvis was performed, revealing a contained rectal perforation with an anterior collection in contact with the uterine wall, a second collection in the soft tissues of the anterior wall below the colostomy, radiation-induced proctitis and cystitis, severe adhesions, moderate dilation of small bowel loops without evidence of obstruction, accompanied by adjacent inflammatory changes, as well as free fluid in the lower abdomen and pelvis. Percutaneous drainage of the abdominal wall collection was carried out, and an internal-internal drain was placed for the pelvic collection via proctosigmoidoscopy, yielding a significant amount of milky fluid. Fluid analysis revealed triglyceride levels of 1068 mg/dL and negative cultures, confirming the diagnosis of chyloperitoneum. With a low-output drain, conservative management was initiated, including abdominal drainage and a low-fat diet as recommended by the nutrition team. After five days of observation, the patient showed symptom improvement and a decrease in drainage output. She was discharged with the drain in place and given dietary instructions. At a follow-up appointment one week later, the patient was asymptomatic, the drain was inactive, indicating full resolution, and it was removed without complications.
Chylous ascites, or chyloperitoneum, is a rare form of ascites, presenting as a milky fluid with high triglyceride levels. Its incidence ranges from 1 in 20,000 to 1 in 187,000 patients.1 Chylous ascites can be classified into traumatic and atraumatic types, with surgical procedures or abdominal trauma being the most common causes in clinical practice.2,3 Atraumatic presentations are much rarer, with lymphatic abnormalities and malignant neoplasms as the most frequent causes.1 Data on radiation-induced chyloperitoneum are limited. It is believed that abdominal radiation induces fibrosis of lymphatic vessels, leading to obstruction and subsequent leakage. Studies report an incidence of up to 3% in patients receiving radiation for gynecological malignancies.4,5
Patients with atraumatic chyloperitoneum often present with abdominal distension (81%) or nonspecific abdominal pain, including peritonism (14%), progressive distension, malnutrition-related weight loss, hypoproteinemia, and dyspnea due to reduced diaphragmatic excursion. In other cases, sudden abdominal pain accompanied by distension and vomiting has been observed, simulating an abdominal obstruction. In 15% of cases, it may present as an acute surgical abdomen, while in 3% of cases, it is incidentally discovered during unrelated evaluations (Figure 1-3).6
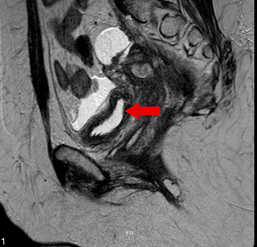
Figure 1 Contrast-enhanced MRI of the abdomen and pelvis in sagittal view shows the presence of a collection and free fluid in the abdominal cavity.
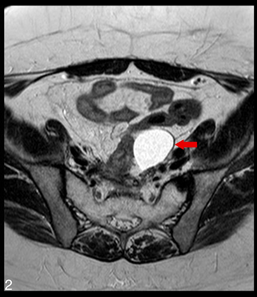
Figure 2 Contrast-enhanced MRI of the abdomen and pelvis in axial view reveals the pelvic collection.
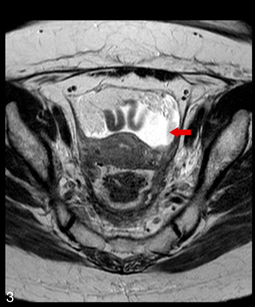
Figure 3 Contrast-enhanced MRI of the abdomen and pelvis in axial view shows the presence of free fluid in the abdominal cavity.
Diagnosis depends on analyses of ascitic fluid, thorough history-taking, and physical examination. For this patient, a significant medical history, including cervical cancer, previous surgeries, and multiple cycles of radiotherapy and brachytherapy, is particularly noteworthy. Diagnostic imaging plays an important role, with basic studies like ultrasound helping to identify fluid in the abdominal cavity.7 Contrast-enhanced abdominal CT scans and magnetic resonance imaging are effective in detecting smaller collections, perforations, or abdominal masses. The appearance of the fluid is also crucial, with chylous ascites diagnosed by triglyceride levels above 200 mg/dL and a milky appearance.1,8
Treatment involves several pillars, including dietary management, drainage of fluid or collections, pharmacological treatment, derivations, or surgical procedures if necessary.9 Oral intake should be suspended initially, with parenteral nutrition being recommended to reduce lymph production. This nutrition should consist of medium-chain triglycerides, with a success rate ranging from 60% to 100% after two to six weeks.7,9 Pharmacological options like diuretics, orlistat, and somatostatin are also available. Drainage or paracentesis decision depends on the patient’s condition and are typically recommended in cases of dyspnea or other complications.7,9 Mortality in chyloperitoneum patients depends on the chronicity of the disease, with rates ranging from 4% in acute events to 40-70% in chronic chylous ascites cases. Increased mortality is mainly due to complications, particularly sepsis and malnutrition.10,11
Chylous ascites or atraumatic chyloperitoneum induced by radiotherapy is rare and should be considered in patients with a history of radiotherapy cycles. Although it presents with nonspecific clinical symptoms, a well-structured diagnostic and therapeutic approach is essential for multimodal management to achieve timely resolution and avoid complications associated with this condition.
None.
The authors declare that there are no conflicts of interest.

©2024 Gómez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.