MOJ
eISSN: 2379-6383


Research Article Volume 9 Issue 5
1Professor in Mathematical Demography & Statistics, International Institute for Population Sciences, India
2Doctoral Student, IIPS, India
Correspondence: SK Singh, Professor in Mathematical Demography & Statistics, International Institute for Population Sciences (IIPS), Mumbai-400088, India, Tel 912242372415, Fax 912225563257
Received: June 30, 2020 | Published: October 12, 2020
Citation: Singh SK, Mishra N, Aditi. Return migration of labourers in the surge of covid-19 in India: multidimensional vulnerability and public health challenges. MOJ Public Health. 2020;9(5):166-173. DOI: 10.15406/mojph.2020.09.00341
Background: The nationwide lockdown imposed in four phases incited by the spread of the COVID in India led simultaneous ramifications, the most rampant of them being the mass exodus of labor migrants to their native places enhancing their multidimensional vulnerability. This paper analyses five dimensions of the vulnerability of the migrant workers returning from high contagion zones in million-plus cities to low-risk rural areas, its contribution to the surge of COVID infections in their native places, and challenges to the public health system.
Data and methods: The SARS-CoV-2 attributable cases and deaths have been taken from the COVID19 India Org website (https://www.covid19india.org/. The total number of COVID cases per lakh population is computed using a district-level projected population as on March 31, 2020. The data on reverse migration has been collated from the Ministry of Railways. It deals with six states having the maximum share of reverse migration in the country. Indicators measuring vulnerability towards preventive practices of COVID at the household level are obtained from the fourth round of Indian DHS.1
Results: There was a sixteen fold increase in clusters of COVID cases once workers employed in the unorganized sectors distressed across the country started reverse migration in May 2020. The increasing number of COVID cases in the rural dominated districts of the migrant-receiving states overburdened their hitherto stressed public health system. States receiving the maximum share of return migrants during the lockdown was Uttar Pradesh, followed by Bihar, Madhya Pradesh, Rajasthan, Odisha, and Jharkhand. The two most unsettling vulnerabilities were their inability to follow social distancing norms and lack of water, soap, or detergent for ensuring hand hygiene. Massive unemployment and disadvantage for the urban economy in terms of shortage of workers were other components of the multidimensional vulnerability of labor migrants engaged in unorganized sectors.
Conclusions: The spread of awareness among the returnees about precautions, ensuring norms of micro-level social distancing in their households and villages is the need of the hour. Public health’s response to COVID-19 should establish a COVID care center in each of around 700 district hospitals with all necessary infrastructures, including trained human resources, medicines, oxygen ventilators, etc. The governments at the origins and the destinations should ensure mechanisms to protect the migrants against multidimensional vulnerabilities that pose a threat to their entities during socio-economic and health emergencies.
The SARS-CoV-2 disease originated in China was declared a worldwide pandemic within two months of its first reported case. Governments across the world initiated lockdowns to curb the spread of the epidemic, which were stretched to months. The subsequent restrictions enhanced the multidimensional vulnerability of daily wage migrant laborers in various developing countries like India. The countrywide lockdown in India from March 25, 2020, which was further extended in four phases till May 31, 2020, to contain the spread of COVID distressed the labor migrants across the country. A survey in April 2020 revealed that the employers did not pay 90 percent of migrant laborers in various states, while 96 percent could not avail ration from the governments, and 70 percent did not get cooked food. There is a growing realization among researchers as well as program personnel that if the lockdown imposed on March 25th, 2020, would have been removed after the first 30-35 days; it might not have fuelled the nationwide reverse-exodus of migrant laborers. This is primarily due to the unavailability of working capital with the enterprises. Among about 63,000 registered enterprises in India, only about 9,500 have the working capital of Rs.100 million or more. Most MSMEs in the country could not support their employees after the initial few days/weeks. It is within this context, the continuation of countrywide lockdown to contain the spread of COVID shoved the labor migrants to highly vulnerable situations accompanying starvation, homelessness, and unforeseen destitution.
In India, moving from villages to bigger cities in search of better livelihood opportunities is not a new phenomenon. The heterogeneity in terms of work opportunity and the different wages of the rural and urban areas of the country have always made metropolitan areas a highly lucrative opportunity for laborers. The cities offer tremendous opportunities in industrial units, construction sites, housing, transportation, service industries, etc. On the contrary, villages and smaller towns, especially in the states dominating the agriculture-based economy, cannot provide better job opportunities to all the people. Hence, metropolitan areas have been better alternatives. India had a total of 5.6 crore migrant laborers in the Census 2011, and the numbers have further increased in the past decade. The major contributors to the rural-urban influx of migrant workers are the North-eastern states and the highly populous states like Uttar Pradesh, Madhya Pradesh, Bihar, Jharkhand, Odisha, Chattisgarh, Jharkhand, and West Bengal. As a result, during the unprecedented crisis of COVID-19, the mass reverse-exodus of migrant workers resulted in a subsequent number of returnees to six major states included in this study. This untoward homecoming of the migrants was accompanied by many of them carrying the virus from the highly populated metropolitan areas to their native places and hence increasing the number of cases at the origin.
With more than 9.6 million cases in the world and 0.5 million deaths as on June 27, 2020, the virus has become an essential concern for the world.2 Although China was the first country to witness this havoc, the world is now experiencing the same predicament. Worldwide, India, United States of America, Italy, Spain, Iran, the UK, and France have larger number of coronavirus cases and deaths.3 These are countries with excellent health care systems; having hospital beds per 1000 population, a manifold than India, still, they are having a tough time with the disease. India has already recorded over 511,478 confirmed COVID-19 cases, and the deadly virus has killed more than 15,731 people as on June 27, 2020.2 As of this date, each of the megacities in the country has more than 50k cases. These cities attract migrants in abundance. With the pandemic prolonging, it has created an enormous demand for essential supplies like protective gear, ventilators, testing kits, and health care professionals. In this regard, rural areas are subjugated, further having both the lack of provisions and the increasing number of cases. The 116 districts of the larger states are witnessing alarmingly high COVID-19 cases and deceased.
The government of India (GOI) had put various travel restrictions on inbound travel and quarantined the travellers who came into the country.4 Further, it had announced a nationwide lockdown for weeks starting March 25, 2020, for all people except those involved in providing essential services. Schools, colleges continue to be shut. It is making every possible effort to make people aware of the disease and the precautions to take to combat the spread of the disease and is sharing multiple strategies and guidelines to create awareness among the public. People are being encouraged to maintain good hygiene (washing hands with proper soap and water for 20 seconds every 20 minutes (WASH practices). The use of alcohol-based hand sanitizers, wearing a facemask, and the most crucial precaution is to follow physical distancing.5 The suspension of rail, inter-state bus services, and metro services were initiatives of unprecedented scale and reflected the government’s resolve to prevent the spread of the pandemic. The government is actively creating isolation wards and arranging testing kits, identifying those who have symptoms as well as providing fast-track provision of medical facilities to those who have symptoms. GOI also announced free cereals and cooking gas to 800 million people through direct transfers till November 2020. Besides, Rs 1.7 lakh crores relief package for those hit the hardest by the COVID-19 lockdown, along with insurance cover for frontline medical personnel, was also put out.6 Additionally, an economic package worth Rs.20 lakh crores for the hard-hit who employ skilled, semi-skilled, and unskilled migrant labourers was also announced.
It is worth mentioning that the decision to lock down the entire country may not be epidemiological. Still, it might have been governed by socio-economic and political decisions, which provide time to strengthen the preparedness to minimize the risk rather than expecting to eliminate the threat. During the 70 days of lockdown, the Government of India, as well as state governments with rapidly increasing COVID cases, could manage to strengthen their preparedness to deal with COVID cases. Yet there has not been a substantial change in the public health response in low prevalence states. As a result, the labor migrants returning to the six states did not find any significant change in preparedness as a public health response.
In the absence of any vaccine, which is the most effective way of dealing with this situation and to end the global COVID-19 pandemic, it is crucial to strengthen tracking, testing, and treating the cases even at the district level. This may limit the spread of the disease through the process of migration and reverse migration of laborers. The condition is even more challenging as infected persons could be asymptomatic and hence, segregating infected persons from the uninfected is very difficult. The therapeutic strategies to deal with the infection are only supportive and preventive aimed at reducing transmission in the community.7 To curtail the spread, social distancing, along with proper hygiene, is the only workable solution along with quarantining of suspected cases and timely treatment of confirmed cases.
The various attempts to contain the transmission of COVID-19 and eventually to minimize its socio-economic and health effects on the community are sombre and daunting as the multidimensional vulnerability of people against protection strategies is highly diversified. These vulnerabilities have multiple facets ranging from fear & stigma, social, economic to wide-ranging health issues. The reversal of labor migrants from May 01 to 31, 2020, has further increased the complexities of the multiple dimensional vulnerabilities. This paper primarily focuses on returned labor migrants from May 01 to May 31, 2020, because GOI started Shramik trains from May 01, 2020, the International Labour Day, and it continued till June 03, 2020, when many other special trains started across the country. That is why an estimated 104 Lakhs labor migrants returned to their native places during this period by various means of transportations, including Shramik Trains, who were initially quarantined for two weeks. The critical research issues addressed in this paper are ‘What are the various dimensions of the vulnerability of labor migrants involved in the process of reversal from high containment zone in metropolitan or million-plus cities in the times of COVID-19?’ And, ‘whether return migrants were the cause of a spike in the number of cases in the migrant-receiving states?’
Keeping in view the aforementioned context of reversal of labor migrants from metropolitan or million-plus cities to their native places, primarily in the rural districts of migrant-receiving states, and the above research questions, the specific objectives of the paper are
This paper uses multiple sources of data on COVID cases. The SARS-CoV-2 attributable cases and deaths are extracted from the COVID-19 India Org website (https://www.COVID-19india.org/). The figures are recorded at two points of time (May 01 and June 27, 2020) for 640 districts of India, categorized as per the Census 2011. The total number of COVID cases per lakh population is computed using a district-level projected population for the year 2020. The district-level ‘population figures’ were estimated employing the ratio method on the population, projected for states of India for the year 2021 by the RGI and Planning Commission. The data on reverse migration has been collated from the Ministry of Railways and reliable news reports based on official press releases. Six states with the highest share of reverse migration were selected for this study. Estimates for the indicators measuring vulnerability towards preventive practices of COVID-19 at the household level were retrieved from the fourth round of Indian version of Demographic Health Survey known as NFHS-4 (2015-16).1 This cross-sectional survey provides data on demographic and health indicators at national and sub-national levels.
Descriptive statistics are utilized for estimating the level of reverse migration in the respective states and their vulnerabilities towards various socio-demographic and health factors. Bivariate analysis is applied to analyze the vulnerability of households in these states based on the selected indicators- crowding in the household, location of the water source, toilet facility, and availability of soap at the place of hand wash. This technique allows the assessment of variations among households based on socio-demographic factors as a function of the selected indicators. Furthermore, a geospatial analysis investigates the heterogeneity in the prevalence of COVID cases per 100000 population and Case Fatality Ratio. Case Fatality Ratio (CFR) is the number of deaths attributed to SARS-CoV-2 per 100 confirmed cases.
It is worth mentioning that by the end of the second lockdown, a substantial proportion of labor migrants employed in unorganized informal sectors and living in low-income urban communities, including designated or non-designated slums at various urban agglomerations, started getting infected by COVID. Fearing community transmission, a substantial proportion of them begun returning to their native places regardless of the scanty mass-transit system in place. The compromised opportunities included Shramik trains, overcrowded trucks/lorries, while others had to walk long distances. With people flooding back to their villages, the susceptibility of rural parts of the country to the virus increased. There was a gradual shift of COVID-19 cases from urban to rural areas. Cases have spurred in the rural areas and towns of states like Uttar Pradesh, Bihar, Madhya Pradesh, Maharashtra, Jharkhand, and Odisha due to the return migration of daily wage earners from Ahmedabad, Delhi, Jaipur, Mumbai, Punjab, Surat, and other cities/states. Quarantining the returnees for the prescribed period is essential to avoid community transmission. Home states faced a tough time dealing with a large number of returnees. Consequently, the states are facing hardships in maintaining physical distancing, testing each of the migrants, providing proper food, and maintaining hygiene in quarantine centers, which enhanced their vulnerability.
Further, the public health systems up to the district level in the migrant-receiving states are not well equipped to deal with testing and treatment of COVID-19 cases. Additionally, returnees quarantining at homes have other kinds of problems to deal with viz. inability to maintain physical distancing and the etiquettes of hygiene at home. These factors increase the risk of COVID-19 to return migrants as well as their family members and close relatives in multiple ways and enhances the challenges for the public health system to equip them with trained and committed staff in the primary health care system along with adequate supplies of logistics and medicines within a short period. Overall, five identified dimensions made the migrant laborers highly susceptible to the pandemic
This has nearly affected 41 million daily wage earners who migrated from rural areas to urban for livelihood as per Census 2011.8
There has been an unprecedented level of effects of the lockdown on the economy concerning the laborers and labor migrants. The nation’s economy plunged, unemployment surged, and innocent lives were lost. The prevailing rate of unemployment at the time of lockdown tripled and reached up to 26 percent. Adding to the precarity of the migrants losing their jobs in towns, villages do not have the employment capacity to absorb so many return migrants. On the other hand, even within four weeks of the chaotic and painful process of reversal of labor migrants, the cities are facing a shortage of workers. There are no laborers to work in small factories, construction firms, etc. With lockdown easing and industries opening, Kerala, Karnataka, Telangana, Punjab, and various other states have already begun to face a shortage of workers for its industries.9 The extent of unemployment varied significantly by gender and poverty, leading to the plight of labor migrants from larger cities and urban agglomerations to their places in the states dominating the agriculture-based economy.
With such a nationwide shutdown imposed, there were lakhs of laborers, daily wage earners, hawkers, and small business people who were hard hit. Helpless people could not manage to afford the food or livelihood. The majority of them were on either a per-day basis or a contractual basis. Earning such a meagre amount, they have to arrange for their food shelter and, in most cases, have to send remittances back in their villages to their families. Hence, survival in cities became next to impossible. The laborers returned using various modes of transportations, including Shramik trains, bus, truck, autorickshaw, and even over a walk. This leads to a complete hustle amongst them, with first of its kind of general exodus of people to their home states or villages. People walked barefooted, thousands of kilometres without proper food or water facilities. Many of them lost their lives to road accidents, starvation, overexertion due to walking, etc. Many innocents lost their lives while the government was protecting the people from the deadly virus. Indian Railways operated a total of 4,165 Shramik Special trains to transport stranded migrant workers during May-June, 2020, and ferried over 63 lakh people amid the pandemic. Around half of the Shramik trains (2069) originated from Gujarat, Maharashtra, and Punjab, whereas Uttar Pradesh and Bihar were the destinations of 90 percent of these trains. Other major destinations of these Shramik trains were the states of Jharkhand, Odisha, Madhya Pradesh, Rajasthan, and West Bengal. Most of the labor migrants returned from megacities during the process of reversal of laborers during May 01 and 31, 2020, were from 116 districts of six larger states listed in Table 1.
Sources: Census of India 2011 and 67 lakh migrants return to 116 dists in 6 states
It is evident from Table 1 that 74.0 percent of the recent volume of out-migrants (population who migrated during the last 0-9 years, i.e., 2001 to 2011) of Bihar returned following COVID triggered lockdown across the country (23.6 lacks). Most of the return migrants were from 32 districts of Bihar. Another larger state, Uttar Pradesh, received 34.6 percent of their recent volume of out-migrants (17.5 lakhs), and they were mainly from 31 districts of the states. Madhya Pradesh experienced returning of 10.7 lacks (87.9 %) of their recent out-migrants, who were primarily from 24 districts. Rajasthan (12.1 lakhs from 22 districts), Odisha (2.2 lakhs from 4 districts), and Jharkhand (1.1 lakhs from 3 districts) have also reported the return migration at a large scale with a share of 85.7 percent, 35.0 percent, and 15.9 percent of the recent volume of out-migrants respectively. The combinations of origins and destinations of Shramik trains match with the major corridors of labor migration from the major out-migrating states, which attracted a lot of attention of researchers and policy planners engaged in curtailing the migration HIV link through the process of migration and return migration in India over the last decade.10
|
States |
Total out migrants, (based on place of the last residence, 0-9 years) |
Number of out-migrants by major destination states |
Number of return migrants Due to COVID 19 and lockdowns |
Number of districts for which return migration data is counted* |
||||
|
Maharashtra |
Delhi |
Gujarat |
Punjab |
Others |
||||
|
Bihar |
31.88 |
3.27 |
5.22 |
2.52 |
1.78 |
19.08 |
23.6 |
32 |
|
UP |
50.46 |
12.11 |
9.69 |
5.37 |
3.02 |
20.28 |
17.48 |
31 |
|
Rajasthan |
14.1 |
2.36 |
0.98 |
3.30 |
0.70 |
6.75 |
12.09 |
22 |
|
MP |
12.19 |
3.48 |
0.57 |
1.50 |
0.16 |
6.49 |
10.72 |
24 |
|
Odisha |
6.26 |
0.71 |
0.22 |
1.18 |
0.06 |
4.09 |
2.19 |
4 |
|
Jharkhand |
6.92 |
0.64 |
0.38 |
0.38 |
0.11 |
5.41 |
1.1 |
3 |
Table 1 Total number of out-migrants (in 100 thousand, i.e., lakh) as per 2011 census and number of return migrants in the six states during the process of reversal of workers due to lockdown
*These districts have been identified as major 116 districts receiving a major share of migrants. Data available so far does not include West Bengal and Chhattisgarh, two major destinations for returning migrants.
The inability of the labor migrants to follow preventive measures at their place of origin is concerning. The most recent Indian DHS known as NFHS1 showed that nearly half of the Indian households (49%) face overcrowding with three or more people using a room for sleeping.1 Hence, migrants returning will not bring much relief in the fight to maintain social distancing. Such households were significantly higher in rural areas (51%), and in the socially deprived and economically marginalized communities, (53%-56% scheduled caste/tribe households; 55% Muslim households, and 62% poorest households). It is evident from Table 2 that among the six out-migrating states, where maximum labor migrants returned during the nation level exodus of lockdown, the proportion of households with household crowding was the highest in Uttar Pradesh (59%) followed by Bihar (55% ), Madhya Pradesh (52%), Rajasthan (49%), Odisha (45%) and Jharkhand (40%). Proportions of households with overcrowding were disproportionately higher among SC/ST, among Muslims, and those from the poorest wealth quintiles. All the above six states are highly populous. They have a large number of labor migrants inhibited there in urban slums and other similar living structures in metropolitan or million-plus cities. Hence, maintaining physical distancing with such a higher influx is implausible. Most of these states have a significant proportion of SC/ST population living in remote rural areas, the socially deprived, and economically marginalized, having poor or no access to healthcare, and hence, now require focused attention on the public health system to save them from succumbing to the vulnerabilities.
|
Vulnerabilities to COVID for return migrants in their place of origin states |
Total |
SC/ST |
OBC |
Others |
Hindu |
Muslims |
others |
Poorest |
Poorer |
Middle |
Richer |
Richest |
|
Household crowding (3 or more persons per room used for sleeping) |
||||||||||||
|
Bihar |
54.5 |
61.3 |
55.5 |
42.2 |
53.4 |
60.6 |
42.3 |
64.7 |
53.1 |
41.9 |
30.3 |
12.6 |
|
Uttar Pradesh |
58.8 |
65.1 |
61.0 |
46.2 |
56.7 |
69.2 |
43.2 |
69.6 |
65.6 |
59.4 |
53.6 |
31.2 |
|
Rajasthan |
49.4 |
60.1 |
47.6 |
35.2 |
48.9 |
58.7 |
35.0 |
69.6 |
60.3 |
50.0 |
41.0 |
24.0 |
|
Madhya Pradesh |
52.8 |
59.9 |
52.8 |
36.8 |
52.7 |
58.7 |
33.8 |
63.5 |
59.5 |
54.3 |
45.5 |
26.2 |
|
Odisha |
45.1 |
48.8 |
43.8 |
38.7 |
45.0 |
57.2 |
39.9 |
54.5 |
48.0 |
40.5 |
31.4 |
17.1 |
|
Jharkhand |
39.5 |
41.3 |
40.0 |
29.7 |
38.5 |
48.4 |
35.7 |
46.1 |
41.4 |
38.9 |
26.7 |
13.9 |
|
Water source located outside premises |
||||||||||||
|
Bihar |
13.8 |
21.6 |
12.7 |
6.8 |
14.3 |
10.7 |
14.2 |
20.8 |
9.1 |
3.9 |
2.2 |
1.3 |
|
Uttar Pradesh |
28.1 |
39.5 |
26.8 |
18.2 |
30.1 |
19.3 |
15.3 |
42.4 |
32.2 |
23.5 |
16.3 |
8.7 |
|
Rajasthan |
42.3 |
55.9 |
39.1 |
26.9 |
43.9 |
34.8 |
9.1 |
78.1 |
58.6 |
39.7 |
24.2 |
8.4 |
|
Madhya Pradesh |
54.9 |
69.3 |
51.5 |
31.9 |
56.7 |
34.4 |
25.1 |
83.7 |
69.3 |
49.3 |
25.3 |
7.3 |
|
Odisha |
68.1 |
81.3 |
66.6 |
43.6 |
68.2 |
42.7 |
80.2 |
87.8 |
74.4 |
59.2 |
36.7 |
11.0 |
|
Jharkhand |
64.4 |
78.5 |
58.6 |
36.6 |
63.7 |
51.8 |
81.3 |
84.2 |
69.3 |
52.1 |
26.0 |
7.5 |
|
No toilet facility within household premises |
||||||||||||
|
Bihar |
66.5 |
82.1 |
67.9 |
41.0 |
67.8 |
59.9 |
56.5 |
94.0 |
62.9 |
18.8 |
2.4 |
0.8 |
|
Uttar Pradesh |
54.2 |
72.9 |
55.7 |
28.7 |
60.0 |
28.0 |
17.3 |
92.7 |
73.5 |
40.6 |
11.0 |
0.9 |
|
Rajasthan |
46.0 |
63.4 |
43.6 |
22.4 |
48.1 |
34.5 |
5.4 |
94.3 |
75.6 |
42.1 |
11.5 |
0.5 |
|
Madhya Pradesh |
57.2 |
75.1 |
53.5 |
27.1 |
59.8 |
24.9 |
19.4 |
95.2 |
80.6 |
44.3 |
9.8 |
0.6 |
|
Odisha |
65.0 |
80.8 |
60.9 |
39.1 |
65.3 |
38.5 |
71.7 |
92.6 |
77.6 |
47.7 |
9.4 |
0.6 |
|
Jharkhand |
70.0 |
83.8 |
66.0 |
35.2 |
70.5 |
54.6 |
82.1 |
95.7 |
81.6 |
51.0 |
9.1 |
0.3 |
|
No Soap/detergents at the place of hand wash |
||||||||||||
|
Bihar |
58.4 |
70.6 |
59.3 |
40.7 |
59.9 |
50.9 |
36.3 |
77.4 |
57.5 |
31.6 |
13.7 |
3.1 |
|
Uttar Pradesh |
28.8 |
39.4 |
29.3 |
14.9 |
30.8 |
20.1 |
7.1 |
55.0 |
32.6 |
17.3 |
7.6 |
2.2 |
|
Rajasthan |
34.6 |
46.9 |
33.6 |
16.6 |
35.8 |
28.0 |
12.2 |
73.5 |
54.1 |
29.7 |
12.8 |
3.0 |
|
Madhya Pradesh |
40.0 |
56.0 |
35.3 |
16.9 |
41.9 |
17.3 |
14.2 |
74.3 |
48.2 |
24.8 |
9.4 |
3.1 |
|
Odisha |
65.5 |
76.6 |
63.7 |
44.7 |
65.6 |
47.1 |
71.7 |
85.3 |
73.3 |
56.7 |
30.7 |
7.9 |
|
Jharkhand |
64.3 |
76.7 |
60.5 |
35.5 |
63.5 |
53.4 |
79.8 |
87.0 |
71.0 |
48.1 |
20.7 |
7.7 |
Table 2 Distribution of households (in %) by their vulnerability to preventive practices of COVID-19 in six states, who have received the majority of labor migrants in the process of reversal of migration due to lockdown
The other two indicators adversely affecting physical distancing in low-income urban communities/ slums are; location of the source of drinking water outside household/dwelling/yard (35%) and no toilet facility within the household premises (38%). Given the situation of migrants receiving states, returned labor migrants from low-income urban communities to their villages are also likely to face a similar challenge of physical distancing. The proportion of households facing such barriers were quite substantial in Bihar (14% & 67 %), Uttar Pradesh (28% & 54%), Rajasthan (42% & 46%), Madhya Pradesh (55% & 57%), Odisha (68% and 65%) and Jharkhand (64% &70%) (Table 2). In each of the six states, the proportion of such households is extremely high among those lying at the bottom of the socio-economic ladder. Thus, the labor migrants returned during the process of return migration following the lockdown, in 116 districts of six major states, are likely to face a triple burden of barriers in maintaining physical distancing, and this augments their vulnerability in resource-poor rural settings of these states.
The second essential means of protection from COVID-19 is the hand hygiene with clear guidelines about frequency and modalities to wash hands with soap or detergent and to sanitize with alcohol-based sanitizers. The NFHS-41 data, however, portrays that despite over 96 percent of households having a designated place for handwashing, almost one out of seven households did not have water available and over one-third households did not have soap or detergent at the place designated for handwashing. The proportion of such households was significantly higher in rural areas (49%), scheduled tribe households (58%), and those from the poorest households (73%). Regional disparity in the proportion of households lagging of the essential facilities to ensure hand hygiene by its members demonstrates comparatively larger concentration of such households in the eastern part of the country (57%), comprising of Bihar, Chhattisgarh, Jharkhand, Odisha, and West Bengal, which are primarily out-migrating states.1 The proportion of such households is substantially higher in the above-discussed six states, having the maximum number of return migrants during the nationwide lockdown. Table 2 portrays a significant proportion of such households in various states viz. Bihar (58%), Jharkhand (64%), Madhya Pradesh (40%), Odisha (66%), Rajasthan (35%), and Uttar Pradesh (29%). Such low prevalence may adversely affect the practices of hand hygiene by labor migrants returning to the states. Similar to other covariates of vulnerability to COVID-19, the likelihood of maintaining hand hygiene was further constrained in the households in the SC/ST caste category and those in the poorest wealth quintile.
Data Source- JHU CCSE
In India, reverse migration of the labor migrants commenced around the end of April and continued till the first week of June, 2020. The national COVID caseload expanded by 14 times between May 01, 2020, and June 27, 2020. On May 01, India had 37,262 confirmed cases and 1,230 deaths; by May 31, the numbers were 190,645 and 5,405 respectively, which further increased to 5,29,484 confirmed cases and 16103 deaths by June 27, 2020 (Figure 1). More than half of the infected cases are the return migrant laborers from larger urban agglomerations. In Bihar, one in four return migrants were corona positive.11 People traveling from Mumbai, Pune, Thane, and Malegaon have been the primary source of infection in many districts across the country.12
The situation in the six selected states is significantly different from the rest of the migrant-receiving states and also varies among these six states. Post the first week of May, these states, which earlier had low COVID-19 attributable cases, witnessed an exponential increase in confirmed cases. The major destinations with predominantly high reverse migration, Bihar, Uttar Pradesh, Rajasthan, and Madhya Pradesh, evidently experienced a high growth rate in COVID cases. It is evident from Figure 2 that each one among these six states has a very controlled number of CIVID infections till May 15, 2020, when most of these returnees were kept in quarantine. Subsequently, the growth in COVID cases increased substantially. Madhya Pradesh and Rajasthan have a higher number of cases in the first two of these eight weeks, but subsequently, the number of confirmed cases increased substantially in Uttar Pradesh. A similar situation was observed in case of Bihar. Inversely, the states of Odisha and Jharkhand endorsing a relatively low increment in the COVID cases are also the states where the volume of returning migrants was small when compared with the six selected states.13
The recent trend in the increasing number of COVID cases portrays two contrasting patterns. First, old containment zones in cities like Mumbai, Delhi, Ahmedabad, Chennai, Indore, Jaipur, Pune, Bhopal, etc., are converting into hotspots with community transmission, where the infected persons are not able to identify the source of infection. On the other hand, the migrant-receiving states/districts witnessed a sharp spurt in the total number of cases since the people started returning. Figure 3 portrays a relative situation of districts in the country in terms of the number of COVID cases per 100,000 population and Case Fatality Ratio. The number of districts with a prevalence of COVID cases of 20 or more per 100,000 populations (projected population for March 31, 2020) has increased from 10 on May 01, 2020, to 160 on June 27, 2020. There is over a sixteen-fold increase in clusters of a higher number of COVID cases within a short span of eight weeks when labor migrants experienced reverse migration and exposed to the local environment. Distribution of such districts on May 01, 2020, was limited to major urban agglomerations like Mumbai, Delhi, Chennai, Ahmedabad, Indore, Bhopal, Jaipur, etc., which on June 27, 2020, spread out across the country from North to South and East to West (Figure 3).14-16
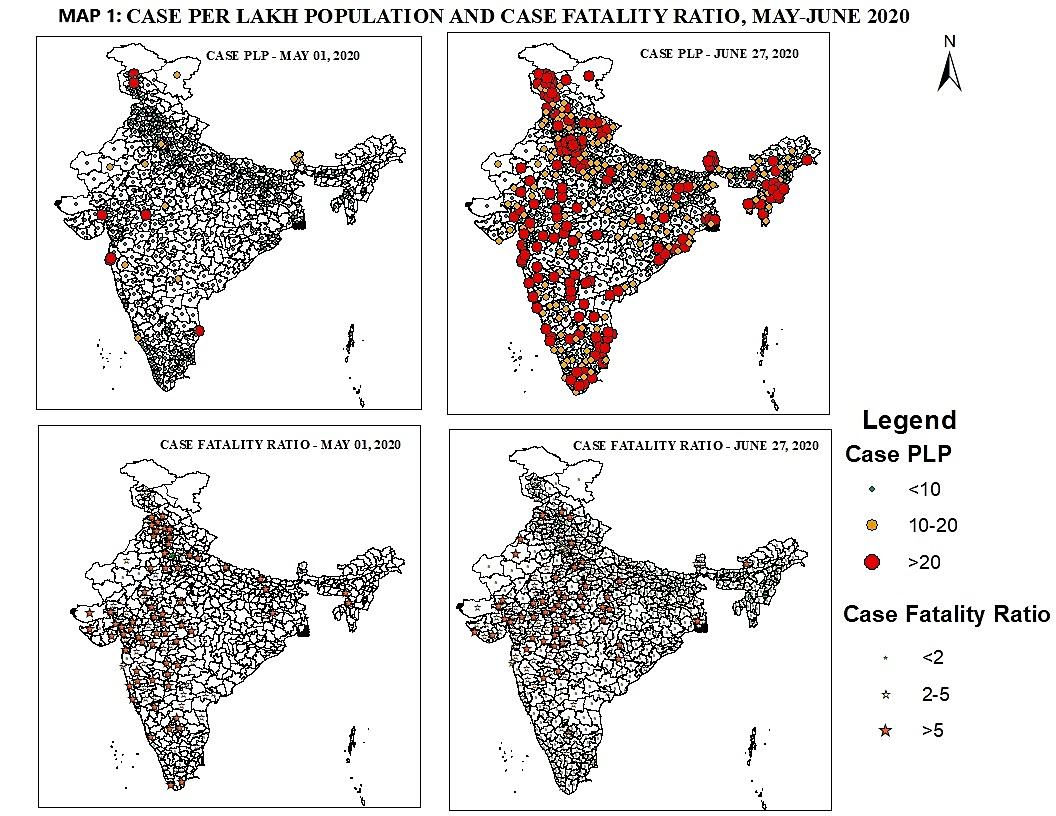
Figure 3 Spatial heterogeneity in the prevalence of COVID-19 cases per 100,000 population and Case Fatality Ratio across 640 districts in the country on May 01st and May 31, 2020, Source of Map: COVID-19 official Portal, GOI.
Several districts in the states of Uttar Pradesh and Bihar, receiving a large share of labor migrants returned from high containment zones of metropolitan cities of the country, witnessed a sudden jump in per lakh caseload in 8 weeks. A significant increase was observed in Azamgarh (from 0.0 to 4.0), Agra (9.7 to 23.2), Basti (0.9 to 6.1), Jaunpur (0.2 to 9.7), Lucknow (4.0 to 19.6), and Varanasi (1.4 to 10.7). Similarly, 11 districts of Bihar, traditionally known for out-migrating hubs, the prevalence of COVID cases on May 01, 2020, was less than one, which increased to around ten or more per 100,000 population. Some of these districts are Arwal, Begusarai, Bhagalpur, Jahanabad, Khagaria, Samastipur, Madhubani, Munger, Kishanganj, etc. There has been a substantial increase in the number of COVID cases in Burhanpur (0.1 to 45.8), Khandwa (3.1 to 20.3), Indore (40.9 to 123.5), and Ujjain (6.5 to 38.1) districts of Madhya Pradesh. In Odisha, the major increase in COVID cases due to reverse migration of laborers were in Ganjam (0.0 to 32.5) and Jajpur (2.1 to 21.3). Another migrant-receiving state, Jharkhand, had two districts with sudden spurts in the number of COVID cases after reverse migration Garwah (0.2 to 6.9) and Koderma (0.1 to 22.6).17-20
The hiking number of COVID 19 cases in the rural zones, specifically the districts receiving migrant laborers from metropolitan or million-plus cities, are expected to face a rise of a humongous burden on the already poor health system. The public health facilities of these districts are already in a pathetic situation, with weak infrastructure facilities, a larger proportion of vacant positions, and a lack of medicines. Apart from this, health workers in these rural dominated districts lack exposure and awareness about managing COVID cases and the strategies to handle the crisis. Lack of oxygen facilities and ventilators are other significant challenges in those resource-poor public hospitals.
There are various dimensions of vulnerability for the return migrants at their place of origin that are predominantly rural and have inadequate health infrastructure to deal with the unprecedented crisis at hand. The increasing number of COVID-19 cases, which has increased over 14 times within a short span of 8 weeks, and enormous problems of household crowding, especially in the households of migrant laborers belonging to socially deprived and economically marginalized groups, lack of hand hygiene provisions, and loss of jobs and wages, demand a focused intervention addressing their health as well as economic well-being. The relief package by the Government of India for the wellbeing of labor migrants may be beneficial for their social and economic wellbeing in the long run. But, a better initiative would have been instant financial support via a conditional cash transfer scheme. The public health system needs to establish and strengthen their CIVID care centers in each of about 700 district hospitals in the country to ensure tracking, testing, and treatment of COVID cases as district levels.
On the other hand, for reinstating them in the labor market, the state governments at the origin, as well as the destinations, should develop a suitable mechanism to ensure social security schemes to protect them under any socio-economic or health emergency. The government of India, as well as state governments, should do their best to ensure that the recent surge in unemployment is not converted into hunger, and the lack of working capital to MSMEs should not lead to bankruptcy. This will require the strengthening of the labor market with ample job opportunities by implementing swift laborer-centered structural reforms by focusing on the formalization of entrepreneurship and planned urbanization.
This paper has three limitations. First, it does not analyze the vulnerability for the states of West Bengal and Chhattisgarh, despite the massive influx of returnee labor migrants. This is primarily due to the unavailability of data. Second, data on a few dimensions of contextual and ecological vulnerability dates back to 2015-2016, the year the Indian DHS was conducted. Although the estimates are considered to be the most reliable, some of the predictors may vary to some extent in the current year. Finally, this study does not explore the vulnerabilities due to the prevalence of co-morbidities and the health system adequacy in the states included in the study.
None.
None.
The authors declare that there was no conflict of interest.

©2020 Singh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.