MOJ
eISSN: 2379-6383


Research Article Volume 13 Issue 3
Federal University of Maranhão, Medicine Course, Pinheiro, Maranhão, Brazil
Correspondence: Consuelo Penha Castro Marques, Departments of Medicine, Universidade Federal do Maranhão, Brasil, Tel (98) 99100-7752
Received: October 25, 2024 | Published: November 8, 2024
Citation: Lima RKMDS, de Souza ACL, Araujo ACRDAE, et al. Prophylaxis of venous thromboembolism after total knee arthroplasty. MOJ Public Health. 2024;13(3):171-176. DOI: 10.15406/mojph.2024.13.00457
Total knee arthroplasty (TKA) surgery is a high risk factor for the occurrence of venous thromboembolism. This represents the main preventable cause of death after major orthopedic surgeries, such as joint replacement surgeries, more than a third of affected patients die suddenly or within a few hours after the first manifestation, that is, before even receiving any type of treatment. Given this, this research aimed to identify the most suitable protocol for thromboprophylaxis in patients undergoing total knee arthroplasty. To this end, an exploratory descriptive study was carried out, an integrative review of the literature from the period 2018 to 2023, in the electronic databases Scielo, Pubmed, Google Acadêmico and RBO. To analyze the articles, the flow diagram was used. All research data was analyzed, subsequently tabulated in Word and the results were presented in tables highlighting the main points for better interpretation of the information collected. The results referring to the bibliography reviewed in this study demonstrated that the advent of new oral anticoagulants (NOACs) resulted in greater adherence, without significant loss of efficacy, resulting in a drop in the number of thromboembolic events up to 60 days after the TKA surgical procedure. With the advent of NOACs, the scientific community is still in debate to determine which protocol holds the title of “most efficient”. As this discussion deepened, we began to consider, in addition to the characteristics of each medication, general and individual aspects of patients recommended for the TKA procedure, thus making VTE prevention increasingly individualized. Therefore, it is concluded, in this review, that the most efficient thromboprophylactic protocol is related to the individual clinical and physiological conditions of each patient.
Keywords: thromboembolism, arthroplasty, anticoagulants, prophylaxis
Total Knee Arthroplasty (TKA) is a major, relatively safe orthopedic surgical procedure.1 However, patients undergoing it are considered at high risk for venous thromboembolism (VTE) given its most common manifestations, deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE).2 When prophylactic measures are not used, the incidence of DVT can reach 60% within 90 days after surgery, and the incidence of fatal PTE can reach 1.5%.3 In both situations, the main treatment consists of full anticoagulation and basically aims to prevent the recurrence of VTE.4
Postoperative edema in TKA is associated with quadriceps weakness, reduced gait speed and worse functional performance. Blood loss, in addition to causing asthenia and delayed rehabilitation, predisposes to the need for blood transfusion, which, in turn, causes immunosuppression, favors infection and is also associated with a greater chance of DVT.5 Therefore, due to these circumstances, orthopedic surgeries, especially hip and knee arthroplasties, are considered very high risk factors for the development of VTE.6
Among the other risk factors for the occurrence of VTE, the following stand out: smoking, diabetes mellitus, deficiency/mutation in coagulation factors, obesity, use of oral contraceptives or patches, hormone replacement therapy, varicose veins, Crohn's disease, colitis ulcerative, age over 60 years, previous history of DVT or pulmonary embolism (PE), family history of thrombosis and prolonged tourniquet time, if used in the procedure.7
Knowledge of the pathophysiology of venous thrombosis and its risk factors, as well as the patient's clinical and physiological history, are essential to assess thromboembolic risk and, therefore, establish appropriate prophylaxis plans. Its pathophysiological characteristics and potential must be constantly considered in clinical practice, not forgetting that the thromboembolic risk of each individual must be periodically assessed.6
The indication for thromboprophylaxis is based on the high incidence of these complications combined with the fact that the majority of patients present with non-specific symptoms, or even without any symptoms, as occurs in most cases.8 Approximately 50% to 60% of DVTs progress to PTE and 10% to 70% of PTE present with DVT. For example, in the ICU the incidence of DVT is 29-31% without prophylaxis and 12% with adequate prophylaxis, which attests to the importance of this care for a good patient prognosis, whether hospitalized in an intensive care unit or recovering home.2
Basically, there are mechanical and pharmacological methods used to prevent VTE. Among the mechanics, early mobilization of the patient stands out; intermittent pneumatic compression, used to reduce venous stasis, as well as to increase blood flow velocity and the level of circulating fibrinolysins; venous pumps, which can increase venous flow; and, finally, graduated compression socks, which provide gentle pressure on the legs to prevent blood accumulation.7 However, mechanical prophylaxis is generally less effective in reducing the prevalence of DVT and PTE, being an alternative to be used in combination or in patients who have absolute contraindications to drug prophylaxis.2
Regarding the pharmacological method, drugs prescribed to prevent the formation or growth of thrombi are called antithrombotics and basically consist of antiplatelet and anticoagulant drugs.7
The first anticoagulant discovered was heparin, a high molecular weight glycosaminoglycan that acts by inhibiting blood clotting through the potentiation of antithrombin III.9 Later, in the 1940s, dicumarol was discovered, a vitamin K antagonist, used as an oral anticoagulant. In 1954, warfarin was introduced, a synthetic derivative of dicumarol, widely used to this day. In the 2000s, direct oral anticoagulants emerged, such as dabigatran, rivaroxaban, apixaban and edoxaban, which act by selectively inhibiting specific coagulation factors, representing an evolution in anticoagulant treatment with less need for laboratory monitoring.10 These discoveries have revolutionized clinical practice, providing safer and more effective therapeutic options for patients with thromboembolic disorders.
Among these, the most commonly used have been enoxaparin, a low molecular weight heparin (LMWH), and rivaroxaban, a new oral anticoagulant (NOAC) that directly inhibits factor Xa.4 However, the effectiveness of VTE prevention achieved is accompanied by an increase in the incidence of local (bruising, superficial and deep infection) and systemic (relevant nasal, gingival and intracranial bleeding) postoperative reactions, creating an issue that has not yet been resolved by the scientific community, which considers the risk-benefit relationship in VTE prophylaxis in view of the aforementioned adverse effects and their consequences.3
Given this, the general objective of this study was to analyze the possibility of a more suitable protocol for thromboprophylaxis in patients undergoing total knee arthroplasty (TKA) after the advent of NOACs.
This study used an integrative literature review. The research consisted of five guiding stages:
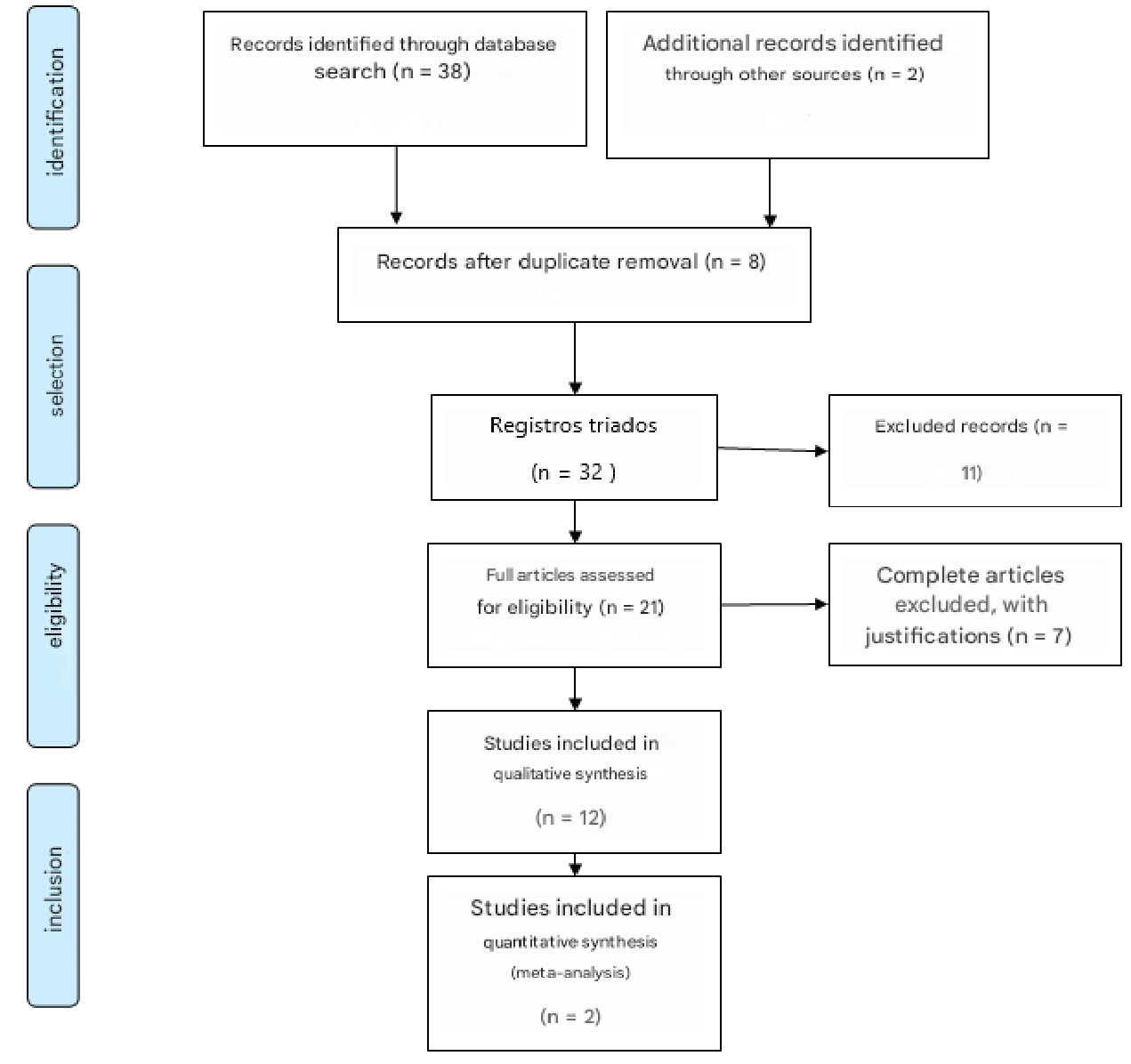
Figure 1 PRISMA diagrama flow 2009.
Source: Adapted by the author, with material taken from: Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
For more information, visit www.prisma-statement.org.
The search was carried out in the electronic databases Scientific Electronic Library Online (SCIELO), Publicações Médicas (PUBMED), Google Acadêmico and Revista Brasileira de Ortopedia (RBO). The PRISMA flow diagram (Moher et al., 2009) will be used to search and analyze the articles (Figure 1). The descriptors were selected by consulting the Health Sciences Subject Descriptors (DECs). The descriptors considered were: “Arthroplasty and Coagulation”, “Arthroplasty and Thromboprophylaxis”, “Thromboembolism and Arthroplasty”, of which only those referring to thromboembolism prophylaxis after total knee arthroplasty were selected.
The inclusion criteria included works in Portuguese and English between 2018 and 2023 that addressed at least one of the specific objectives outlined in the study. As for the exclusion criteria, works that did not address at least one of the specific objectives, that were outside the period mentioned, articles that did not address the topic studied, works that were not published in full, as well as duplicate articles were excluded. In order to evaluate the articles selected, a systematic instrument was drawn up to collect the information, using the Microsoft Excel program to tabulate and analyze the data obtained, with the aim of answering the guiding question of this study.
As this is a bibliographical study, it does not require the approval of the Research Ethics Committee. This work was based on the guidelines and regulatory standards established in resolutions 466/2012 and 580/2018 of the National Health Council of the Ministry of Health.
According to the bibliographic search, the final sample was 14 articles published in the evaluated databases. Regarding the origin of publication, this review contains mostly Brazilian articles. Regarding the field of knowledge, 100% of the materials used were from the health area.
As for the years of publication, 2018 and 2022 were the years in which there were the highest number of articles published, with 5 and 4 publications, respectively, representing 60% of the articles reviewed. There are no motivations for these results found. According to the objectives, both general and specific, divided into analysis categories, such as:
The results referring to the bibliography reviewed in this study demonstrated that the advent of new oral anticoagulants resulted in greater adherence without significant loss of efficacy, resulting in a drop in the number of thromboembolic events up to 60 days after the TKA surgical procedure. Table 1 shows the results of the bibliographic search.
|
Authors and year |
Article |
Country of origin |
Design |
Highlights |
|
Alameri MA, et al.1 |
Venous thromboembolism prevention protocol for adapting prophylaxis recommendations to the potential risk post total knee replacement: a randomized controlled trial. |
Saudi Arabia |
Randomized study conducted in two Arab medical centers, involving 242 patients. They evaluated the risk stratification protocol and education about VTE after TKA. |
The proposed VTE risk stratification protocol, applied in conjunction with patient education programs, reduced VTE complications and readmission events after TKA surgery. |
|
Oliveira A, et al.2 |
Venous thromboembolism prophylaxis for hospitalized patients. |
Brazil |
Study based on the Venous Thromboembolism Prophylaxis Protocol in Hospitalized Patients, from Unimed Recife. |
After using the clinical protocol in 6.335 eligible patients hospitalized from January to December 2020, there was a significant reduction in the occurrence of DVT and PTE. |
|
Colleoni JL, et al.3 |
Venous thromboembolism prophylaxis after total knee arthroplasty: aspirin vs. Rivaroxaban. |
Brazil |
Randomized study carried out with 32 patients indicated for TKA. Compares the efficacy and safety of aspirin and rivaroxaban in preventing VTE after TKA. |
No differences were identified between the groups (rivaroxaban and aspirin) regarding local complications, systemic complications, DVT, readmission, reoperation and death (p > 0.05). |
|
Pereira JARM.5 |
Edema and blood loss after total knee arthroplasty with mechanical thromboprophylaxis or enoxaparin: randomized clinical trial. |
Brazil |
Randomized clinical trial that aims to evaluate edema in the operated lower limb and blood loss after total knee arthroplasty (TKA) in patients undergoing two thromboprophylaxis methods: pharmacological and mechanical. |
Exclusively unilateral mechanical prophylaxis reduces edema in the leg and ankle and also blood loss in the postoperative period of TKA, when compared to exclusively pharmacological prophylaxis with enoxaparin. |
|
Kakkos SK, et al.,6 |
Clinical Practice Guidelines on the Management of Venous Thrombosis. |
Europe |
European clinical practice guideline for the treatment of Venous Thrombosis. |
Delimitation of the concept, diagnosis, complications and treatment of thromboembolic events in the lower limbs. |
|
Gali J, Camargo D.7 |
Thromboprophylaxis in total knee arthroplasty. |
Brazil |
The authors describe an update on the main methods of preventing deep vein thrombosis after total knee arthroplasty. |
Rivaroxaban was compared to enoxaparin in the Record studies. There was less bleeding at the surgical site in TKA with the use of rivaroxaban. |
|
Afshari A, et al.,8 |
European guidelines on perioperative venous thromboembolism prophylaxis: Mechanical prophylaxis. |
Europe |
European guideline for perioperative venous thromboembolism prophylaxis. |
After joint replacement surgery, combination therapy also significantly reduced the rate of DVT (from 18.7 to 3.7% after elective knee arthroplasty and from 9.7% with anticoagulation alone to 0.9% with additional mechanical compression . |
|
Marrannes S, et al.,17 |
Prevention of venous thromboembolism with aspirin following knee surgery: A systematic review and meta-analysis. |
Europe |
Systematic review to compare the effectiveness of aspirin prophylaxis after knee surgery with current standard prophylactic agents (low molecular weight heparin [LMWH], vitamin K antagonists, and factor Xa inhibitors). |
No significant difference in the effectiveness of VTE prevention was found between aspirin, LMWH, and warfarin. Factor Xa inhibitors were more effective, but increased bleeding complications were reported. |
|
Yi Y, et al.,15 |
New Oral Anticoagulants for Venous Thromboembolism Prophylaxis in Total Hip and Knee Arthroplasty: A Systematic Review and Network Meta-Analysis. |
Europe |
Systematic review and meta-analysis with the objective of synthesizing the evidence on NOACs in the prevention of venous thromboembolism (VTE) in patients with total hip and knee arthroplasty (THA and TKA). |
Evidence suggests that NOACs exert more benefit in VTE prophylaxis, and none of the individual NOACs increased hemorrhage compared with non-NOACs. Among several NOACs, rivaroxaban is recommended in patients with a lower risk of bleeding, and apixaban is recommended in patients with a higher risk of bleeding. |
|
Albricker ACL, et al.,11 |
Joint Guideline on Venous Thromboembolism. |
Brazil |
Joint guideline on venous thromboembolism. |
After an initial episode of DVT, recurrence may occur in approximately 25% of patients within 5 years and be responsible for the increased risk of pulmonary embolism and post-thrombotic syndrome. |
|
Anderson DR, et al.,12 |
Aspirin or Rivaroxaban for VTE Prophylaxis after Hip or Knee Arthroplasty. |
Europe |
Multicenter, double-blind, randomized, controlled study involving patients undergoing total hip or knee arthroplasty. |
Major bleeding complications occurred in 8 patients (0.47%) in the aspirin group and in 5 (0.29%) in the rivaroxaban group (difference, 0.18 percentage points of age; 95% CI, -0.65 to 0. 29; P = 0.42). Clinically important bleeding occurred in 22 patients (1.29%) in the aspirin group and in 17 (0.99%) in the rivaroxaban group (difference, 0.30 percentage points; 95% CI, -1.07 to 0.47; P = 0.43). |
|
Papakonstantinou PE, et al.,13 |
Anticoagulation in Deep Venous Thrombosis: Current Trends in the Era of Non- Vitamin K Antagonists Oral Anticoagulants. |
Europe |
Review article that evaluates advantages and disadvantages of NOACs in relation to vitamin K antagonists. |
NOACs offer a simple route of administration (oral agents), a rapid onset of action, along with a good efficacy and safety profile compared to Vitamin K Antagonists (VKAs). |
|
Rodarte RRP, et al.,14 |
Systematic review of prophylaxis for venous thromboembolism after knee arthroplasty: enoxaparin versus rivaroxaban. |
Brazil |
Systematic review of the literature to compare the effectiveness of enoxaparin and rivaroxaban in preventing this complication and the risk of intraoperative bleeding. |
Observed in their study of clinical trials that rivaroxaban 10 mg compared to enoxaparin 40 mg (control) showed superiority in terms of venous thromboembolism events in total knee arthroplasty (RR 0.32; 95% CI 0.15-0.67). |
|
Gali JC, Silva PAC DA,16 |
Summary of prevention of deep vein thrombosis in total knee arthroplasty. |
Brazil |
Succinct and updated description presenting a comparison between thromboprophylactic methods and protocols after TKA. |
In a randomized, double-blind study of 2,531 patients, rivaroxaban was superior to enoxaparin for preventing DVT after TKA, with similar rates of bleeding. |
Table 1 Description of studies included in the integrative literature review
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a well-known preventable complication after medium and major orthopedic surgeries on the lower limbs.2 It represents the third most common cause of acute cardiovascular syndrome in the world, with a potential risk of death. Approximately 34% of affected patients die suddenly or within a few hours after the first manifestation, that is, before they even receive any type of treatment.11 And it basically consists of the emergence of thrombi resulting from the reduction in blood flow caused by venous stasis, endothelial injury and hypercoagulability (Virchow's triad), which are consequences of long periods of anesthesia added to the trauma resulting from the surgical technique used.6
In a more specific analysis of the pathophysiology of VTE, molecular biology has explained the relationships between inflammatory mediators and the coagulation mechanism, with stimulation of procoagulant substances and inhibition of anticoagulants and fibrinolytics. These mediators can be released into the systemic circulation, they can also be released locally in the traumatized area or even contained within the thrombus itself, increasing its volume. The factors causing this increase are the recruitment and accumulation of activated platelets and leukocytes at the site of the thrombus by triggers of vascular thrombosis and inducers of the inflammatory response. Under normal conditions, blood presents a laminar flow, in which the different cellular elements are distributed in layers depending on their electrical charges, the red blood cells in a central position, faster, and the platelets more peripherally, in a slower layer. The normal endothelium is not reactive to these components or coagulation proteins, maintaining a thrombohemorrhagic balance with a slight tendency towards anticoagulation, which provides the ideal condition for adequate blood flow.11
However, due to extrinsic factors (e.g. trauma, surgery) and/or intrinsic factors (e.g. cytokines and other inflammatory mediators) endothelial injury occurs. In response to this injury, the thrombohemorrhagic balance changes, favoring the production of thrombin and the formation of thrombus, which can be enlarged by selectins, proteins responsible for the adhesion of leukocytes to the vascular endothelium in the early cascade of events that lead to the processes of inflammation.6
The guideline published in 2012 by the American Academy of Orthopedic Surgeons (AAOS) on the prevention of VTE in patients undergoing elective knee arthroplasty reported the risk of hemorrhage and complications associated with bleeding. In this document, the indication for prophylaxis followed the categories of patients, who were classified according to whether there were risk factors present or not, in addition to what was already offered by the TKA procedure. Firstly, for patients without a high risk of thromboembolism or venous bleeding, the use of pharmacological agents and/or mechanical compression devices was recommended. For patients with a history of previous VTE, pharmacological prophylaxis in association with mechanical compression devices was indicated; For those who have absolute contraindications to drug prophylaxis, such as a known bleeding disorder and/or active liver disease, the use of mechanical compression devices and early ambulation only is suggested.7
Among the drugs indicated for VTE prophylaxis after TKA surgery, antiplatelet and anticoagulant drugs stand out. The most recommended, initially, was aspirin, a low-cost antiplatelet drug considered safe which, in association with mechanical prophylactic methods, proved to be significantly effective in preventing VTE.12
With regard to anticoagulants, coumarins were the first to be used for the prevention of VTE, more specifically warfarin, an oral anticoagulant that is a vitamin K antagonist. However, this drug is accompanied by a series of disadvantages: a long time to onset of action, long half-life, need for monitoring (INR) and the interaction between coumarins and diet.7 Its greatest contribution to the topic in question is related to obtaining statistical data from studies that compare it with other anticoagulant agents, such as low molecular weight heparins (LMWH) and factor Xa inhibitors, such as enoxaparin and rivaroxaban, respectively.13
Regarding the last two classes mentioned above, it can be said that they are the main drugs currently used in VTE prophylaxis after TKA, with rivaroxaban being the main representative of NOACs.14
Enoxaparin is a low molecular weight heparin (HPBM) synthetic from unfractionated heparin (UFH) that acts by inhibiting factor Xa of the coagulation cascade. It is a widely studied injectable anticoagulant, when compared to rivaroxaban, and proven effective.13 Its recommended prescription is a dosage of 40 mg subcutaneously 24 hours after closing the surgical incision and maintained for 10 to 14 days, this being the time interval that presented the best results in preventing VTE and safer in terms of the occurrence of major bleeding.7 However, when compared to the associative method of aspirin and mechanical compression, the use of LMWH showed higher rates of readmission, major complications and wound problems after primary total arthroplasties.12
Regarding rivaroxaban, it can be said that it is the anticoagulant with the greatest scientific relevance today. It is a direct inhibitor of factor Xa and is administered orally at a dosage of 10 mg once a day, six to eight hours after surgery.15 When compared to enoxaparin at a dose of 40 mg 24 hours after closing the surgical wound, rivaroxaban showed a lower incidence of venous thromboembolism as well as less bleeding at the surgical site after knee joint replacement.14
Dabigatran is an oral anticoagulant that directly inhibits thrombin. The recommended dosage is 110 mg four hours after surgery, then 110 mg twice a day for 10 days for TKA.15 In a study of 1,728 patients undergoing primary joint arthroplasty, the use of dabigatran caused significant bleeding from the surgical wound postoperatively. Patients who used dabigatran had a higher incidence rate of DVT when compared to those who used enoxaparin and aspirin.16
Like enoxaparin, apixaban is also a factor Xa inhibitor. Its suggested dose is 2.5 mg twice a day, starting 12 to 24 hours after the operation and continued for 12 days after TKA.15 A study comparing the use of 2.5 mg apixaban twice a day with 40 mg daily enoxaparin showed that the former is more effective than the latter, without increasing bleeding.16 A systematic review with meta-analysis and indirect treatment comparison compared the use of rivaroxaban, apixaban and dabigatran versus enoxaparin for prophylaxis against DVT after TKA. The study concluded that when compared to enoxaparin, rivaroxaban presented a higher risk of bleeding and dabigatran presented a similar risk, being lower only in apixaban. The risk of DVT was lower with rivaroxaban and similar with the others.2
Faced with the changing landscape resulting from the eventual emergence of New Oral Anticoagulants (NOACs), prophylactic methods now include numerous medication options. However, the scientific community is still in debate to determine which protocol holds the title of “most efficient”. As this discussion deepened, we began to consider, in addition to the characteristics of each medication, general and individual aspects of patients recommended for the TKA procedure in a more complex way, thus making VTE prevention increasingly individualized.17
The protocols that incorporated NOACs, with rivaroxaban as their main representative, showed satisfactory safety in terms of the occurrence of major hematomas or bleeding up to 60 days after the surgical procedure, whether associated or not with aspirin and mechanical methods. It also showed high adherence when compared to injectable methods, such as low molecular weight heparin (HPBM) and unfractionated heparin (UFH), due to greater ease of administration and the lack of need for frequent laboratory monitoring.
With regard to effectiveness, the prescription of a protocol proved to be relative, as the approach must be individualized, considering the risk-benefit for each patient according to their clinical profile, and closely monitored for adjustments as necessary. However, despite the inherent relativity of the medication method, early ambulation after the procedure is recommended, as well as the use of compression stockings, as basic mechanical methods are essential and improve the prognosis regardless of the associated medication method.
None.
The authors declare there is no conflict of interest.
None.

©2024 Lima, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.