MOJ
eISSN: 2379-6383


Research Article Volume 13 Issue 3
Federal University of Maranhão, Medicine Course, Pinheiro, Maranhão, Brazil
Correspondence: Consuelo Penha Castro Marques, Federal University of Maranhão, Medicine Course, Pinheiro, Maranhão, Brazil, Tel +55 98 99100-7752
Received: August 22, 2024 | Published: September 11, 2024
Citation: Marques ALPC, Neto JCGP, Ferreira FRD, et al. Mortality from pemphigo in Brazil in 02 decades. MOJ Public Health. 2024;13(3):148-152. DOI: 10.15406/mojph.2024.13.00453
Pemphigus is a rare and sometimes fatal autoimmune disease in which the body itself gathers defense cells to attack the desmoglein proteins, responsible for adhesion between the layers of the skin, causing acantholysis. It usually manifests initially in the oral cavity, progressing to the skin of other regions of the body. Given the risk and the difficulty in diagnosing this pathology, the objective of this study was to study the epidemiological profile of mortality due to pemphigus in Brazil, from 2000 to 2020. Thus, a cross-sectional, epidemiological and descriptive-analytical study was carried out, with secondary data from TABNET-DATASUS-Ministry of Health-Brazil, corresponding to deaths occurring in the Brazilian population. The collected data were tabulated in Excel and the results presented in graphs and tables and expressed in absolute numbers and frequencies. They were statistically analyzed using the Bioestat 5.3 Program, in which the mean, standard deviation, and correlation (Pearson's Correlation Test) were analyzed, considering p-value <0.05. There were n = 1511 deaths from this pathology in Brazil, in the period under study, the year 2015 presented the highest number of deaths n = 116. The region with the highest mortality was the Southeast (46%); the most affected sex was female (59%); the age group with the most deaths was 80 years and + (29%); the most affected color/race was white (52.2%); there was a lower number of deaths in people with 12 years of schooling and more (4%); marital status, preferably affected, married (34%); place of occurrence: hospital (84%). Even though it is a rare, treatable disease with low lethality, a significant number of deaths from pemphigus occurred in Brazil during the decades under study. It is easy to treat with corticosteroids and other medications, but requires early diagnosis to contain its progression and improve prognosis. Therefore, these deaths indicate the need for better diagnosis and early treatment to inhibit mortality from pemphigus in Brazil.
Keywords: pemphigus, epidemiology, mortality
The global epidemiology of autoimmune diseases infers a disease burden of approximately 2% of the population, affecting both men and women, and in the last 40 years, in the United States, this rate has doubled.1 They encompass a broad group of diseases, complex and diverse, with some diseases still little investigated, which require further studies, to better understand the various molecular, genetic and immunological pathways, whose activation or even blockage of the pathway can lead to autoimmune intolerance disorders, whether due to genetic, hormonal, pathogenic, epigenetic and/or xenobiotic factors.2
Pemphigus is classified as a rare and sometimes fatal autoimmune, mucocutaneous, bullous disease in which the body itself gathers defense cells to attack the desmoglein (Dsg) proteins, responsible for adhesion between skin layers, with acantholysis and the appearance of interepithelial vesicles that easily burst and damage the tissue. Its diagnosis is made by symptoms, often present in the oral cavity, and may eventually present in other parts of the body. The Nikolsky Test is indicated for its diagnosis. It presents rare lesions, without delimitation of borders, with pseudomembranes, present in the labial and jugal mucosa, ventral tongue, palate, cheek and gums. It advances with the activation of various immune activation mechanisms, such as the production of autoantibodies by plasma B cells, activity of autoreactive CD4 + helper T cells (Th), and CD8 + T cells.3,4,5
Types of pemphigus: pemphigus vulgaris, pemphigus vegetans, pemphigus foliaceus and pemphigus erythematosus and paraneoplastic pemphigus.6 Difficulty in feeding and the accumulation of biofilm due to incomplete hygiene due to intense pain from pemphigus tissue lesions are controlled, in the vast majority of cases, with corticosteroids, in order to stop the worsening of ulcerations in the pathogenic picture and delay the appearance of PV wounds in other epithelial extensos of the patient, thus improving the prognosis of the individual with this rare autoimmune disease.4
Even with advances in the use of immunosuppressive drugs for the treatment of pemphigus, the disease still has a high mortality rate of around 10%, which may be associated with adverse events from the treatment itself. Therefore, professionals must improve their diagnosis to determine its extent and severity, thus ensuring improvements in treatment.7
Given the relevance of the topic, which does not present many advances in terms of the literature or even in terms of the management of the disease, which, although rare, causes great morbidity to its carriers, with serious consequences that can extend to death, this research is considered to be of great importance, which aimed to study the epidemiology of deaths from pemphigus in Brazil, from 2000 to 2020.
This study is a cross-sectional, quantitative, time-series (from 2000 to 2020) and epidemiological study on mortality from pemphigus in Brazil, with data from the entire Brazilian population notified with deaths from pemphigus in 02 decades, such data were collected through the official website of the Brazilian Ministry of Health - Mortality Information System (SIM), in which the variables related to deaths from pemphigus were explored: Brazil, Region, Number of deaths by place of residence, Sex, Age group, Color/race, Education, Marital status, Place of Occurrence, ICD-10-L10 Category and year of processing.
These data were tabulated in EXCEL spreadsheets and submitted to statistical analysis using the BIOESTAT 5.3 program for descriptive and analytical statistical study. Initially, the general characteristics of the study were described in absolute numbers and frequencies. Then, the means, standard deviation and coefficient of variation were calculated, and subsequently the correlation between the variables under study that were shown to be suitable for correlation analysis. Since this was a population study, the Pearson Correlation Test was used, considering a p-value <0.05 as statistically significant.
Regarding ethical aspects, since this is a collection of secondary data available in an official and public database of the Ministry of Health-Brazil (DATASUS), without individual identification, without access to data that infringes any violation of the privacy of individuals, this research did not require submission/approval by a Research Ethics Committee.
Deaths from pemphigus in Brazil from 2000 to 2020 totaled n=1511 cases, demonstrating an oscillating trend, with an increasing trend until 2018, although some years are below the trend line, as shown in Graph 1. The year 2015 was the year with the highest number of deaths from this pathology with n=116, the year 2001, in turn, was the year with the lowest number of deaths from pemphigus in Brazil with n=33. The largest growth peaks in these deaths were observed in 2006 (n=72), 2010 (n=87), 2015 (n=116) and 2016 (n=107) and 2018 (n=113). The last years of the study showed a decrease in 2019 (n=84), already with a slightly increasing trend in 2020 (n=90). The mean was = 71.95± 26.13 and Coefficient of Variation (CV)=36.32%.
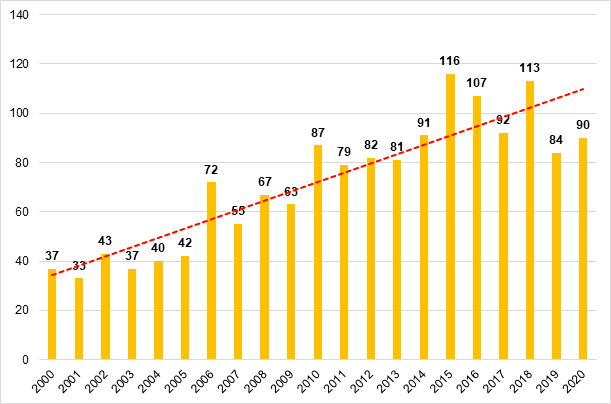
Graph 1 Distribution of deaths from pemphigus in Brazil, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System - SIM, 2024.
Regarding the Brazilian Regions (Graph 2), mortality from pemphigus was highest in the Southeast region with 46%, followed by the Northeast region with 22%, South with 14%, North with 11% and Central-West with 7%. In the Southeast, we obtained a mean=32.86±12.39 and CV=37.70%; in the Northeast mean=16.00±7.39 and CV=46.18%; in the South mean=10.43±3.20 and CV=30.71%; in the North mean=7.71±5.48 and CV=59.42%; in the Midwest mean=4.95±3.17 and CV=64.01%.
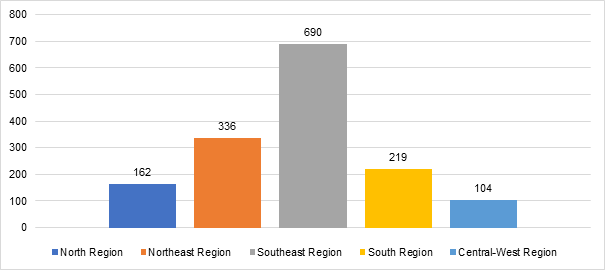
Graph 2 Distribution of deaths from pemphigus in Brazil, by Region, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System - SIM, 2024.
Regarding the distribution of deaths from pemphigus in Brazil per year (Graph 3), it is observed that there was an oscillating trend in all regions over the years under study. In the Southeast there was a higher peak in 2018 with n=57 deaths and fewer deaths in 2003 with n=11; in the Northeast we had the biggest peaks in 2015 and 2019, both with n=26 and fewer deaths in 2004 with n=03; in the South the biggest peak was in 2015 with n=17 and fewer deaths in 2007 with n=05; in the North, the biggest peak was in 2016 with n=19 and fewer deaths in 2000 and 2001, both with n=02 and in the Central-West the biggest peak was in 2014 with n=12 and fewer deaths in 2002 with n=0.
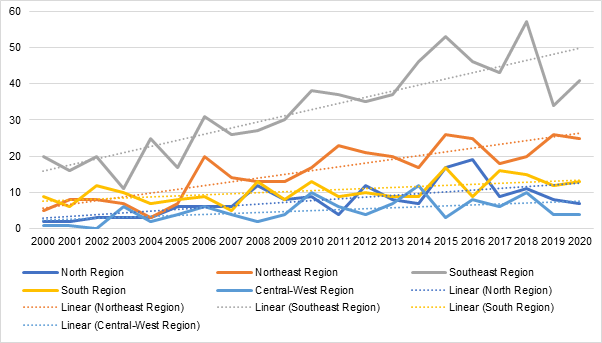
Graph 3 Distribution of deaths from pemphigus in Brazil, by Region/Year, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
There was a correlation in the distribution of deaths from pemphigus between most regions, except between the North and Central-West, as well as between the South and Central-West, therefore, applying the Pearson Correlation Test and considering p<0 .05 for statistical significance, we obtained the following results from the correlation analysis: North and Northeast: p=0.0009 and r (Pearson) =0.6672; North and Southeast: p=0.0004 and r (Pearson) = 0.7055; North and South: p=0.0244 and r (Pearson) =0.4890; North and Midwest: p=0.1493 and r (Pearson) = 0.3259; Northeast and Southeast: p=< 0.0001 and r (Pearson) =0.7916; Northeast and South: p=0.0355 and r (Pearson) =0.4606, Northeast and Central-West: p=0.0472 and r (Pearson) =0.4376; Southeast and South: p=0.0053 and r (Pearson) =0.5852; Southeast and Midwest: p=0.0037 and r (Pearson) =0.6047; South and Midwest: p=0.4892 and r (Pearson) =0.1597.
Concerning gender (Graph 4), males had n=615 and females n=896 deaths, it is noted that females had a higher frequency of deaths due to this disease, representing 59% of cases, and males 41%.
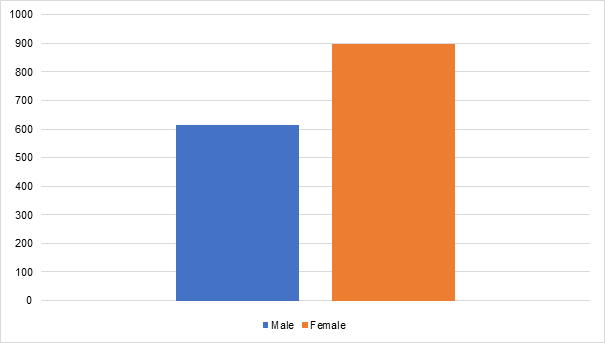
Graph 4 Distribution of deaths from pemphigus in Brazil, by sex, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
Regarding the age group (Graph 5), up to 9 years of age the number of deaths due to pemphigus is low with n=3, for each age group; from 10 to 14 years old, an increase of more than 100% in the number of deaths with n=8 can be seen; observing continuous growth throughout subsequent age groups; from 15 to 19 years old the number of deaths was n=15; 20 to 29 years old there were n=38 deaths; 30 to 39 years old o n=84; from 40 to 49 years old n=163; from 50 to 59 n=198; from 60 to 69 years old n=286; from 70 to 79 years old n=279 and in the age group of 80 years old and over n=431 deaths. From 40 years of age to 80 and over, there are 90% of all cases of death from pemphigus in Brazil, with the age group of 80 years and over representing 29% of all cases.
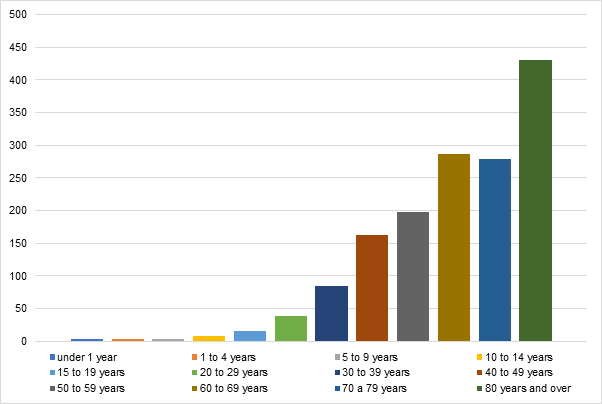
Graph 5 Distribution of deaths from pemphigus in Brazil, by age group, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
Regarding color/race (Graph 6), deaths from this disease were more frequent in Whites with n=788 deaths, representing 52.2% of the sample; followed by Pardos with n= 485, representing 32.1%; Blacks with n=123, representing 8.1%; Ignored with n=75, representing 5%, Yellow and Indigenous, both with n=20, representing 1.3% each. White and brown people account for the vast majority of deaths, accounting for 84.3% of the sample.
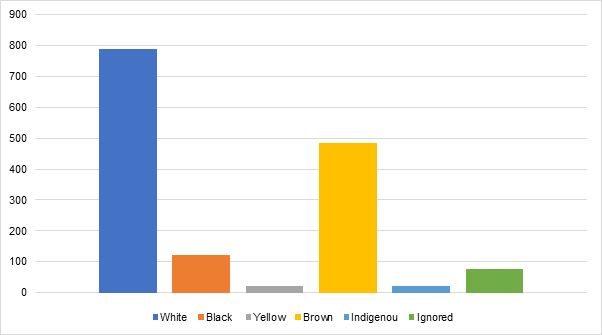
Graph 6 Distribution of deaths from pemphigus in Brazil, by color/race, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
As for education (Graph 7), those with 12 years or more of education had the fewest deaths with n=67 cases (4%). Many have unknown education: n=401 (27%); none: n=262(17%); 1 to 3 years: n=356 (24%); 4 to 7 years n=266 (18%); 8 to 11 years: n=159 (10%). It is therefore observed that 41% of the sample studied for up to 3 years.
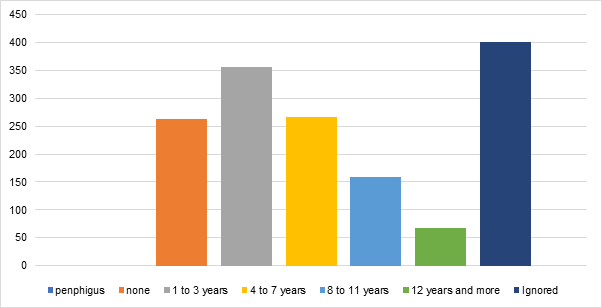
Graph 7 Distribution of deaths from pemphigus in Brazil, by education level, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
When studying marital status (Graph 8), it was observed that the majority of cases occurred in married couples: n=520 (34%); followed by singles: n=388 (26%); widowers: n=376 (25%); legally separated: n=76 (5%); other: n=41(3%); ignored: n=110(7%).
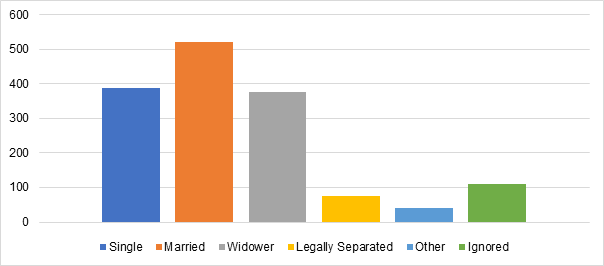
Graph 8 Distribution of deaths from pemphigus in Brazil, by marital status, from 2000 to 2020.
Source: Prepared by the authors, with data from the Brazilian Ministry of Health - MS/SVS/CGIAE - Mortality Information System – SIM, 2024.
Finally, regarding the place of occurrence (Graph 9), it was observed that the vast majority died in the hospital n=1268, representing 84% of deaths; followed by Household with n=193, representing 13%; Others with n=24, representing 1.60%, Other health establishment n=21, representing 1.40%; Public road n=03 and location of Ignored Occurrence n=02, each representing 0% of the sample.
Through this research, a worrying number of deaths caused by pemphigus (n=1511) was observed over the 20 years of study, with an increasing trend until 2018, with some decreases throughout the period and showing a decreasing trend. in 2019 and, shortly thereafter, an increase in 2020, thus highlighting the need for greater attention to this pathology. According to Pires et al.,8 mortality rates for this pathology range from 3.62% to 20%, which validates the need for more studies that can express the real incidence of deaths caused by pemphigus.
In relation to the Brazilian Regions, the number of deaths due to pemphigus showed considerable differences in distribution, being significantly higher in the Southeast, followed by the Northeast. Corroborating the results of this research, Magalhães, et al.,9 states that among the main places with the occurrence of the pathology are the states of São Paulo and Minas Gerais, members of the Southeast Region. According to a study by Celere,10 carried out in the northeast of the State of São Paulo, in the Southeast Region, endemic pemphigus foliaceus presented a mortality rate of 1.9 per 100,000 inhabitants in the period from 1995 to 2004 and a mortality rate of 1.8 per per 100,000 inhabitants in the period from 2005 to 2014 in the municipality of Batatais, while pemphigus vulgaris showed mortality of 0.6 per 100,000 inhabitants in the period from 1995 to 2004 and mortality of 0.3 per 100,000 inhabitants in the period from 2005 to 2014 in the municipality of Ribeirão Preto, which proves the numerically significant existence of deaths caused by this pathology in the Southeast region.
The North region ranks 4th nationally in terms of numbers of deaths, corroborated by Pires et al.,8 based on a study carried out in the state of Pará over a period of 8 years, showing a relatively small number of patients compared to other federative units. The present study points out that the Central-West Region has the lowest rates of deaths caused by pemphigus, however, Campbell et al.,11 infers that the Central-West Region concentrates a high number of cases, with significant involvement of indigenous populations.
It is estimated that around 3 to 5% of the world's population is affected by autoimmune diseases, with a higher frequency in women.12 In relation to pemphigus, the distribution of deaths in Brazil regarding sex follows the global trend: it was noted that females had a higher frequency of deaths from this disease, representing 59% of cases, corroborating research that showed more deaths among women by pemphigus in other countries, as observed in the study by Kridin et al.13
As most autoimmune diseases are more common in women, there are some theories that propose explanations for this bias, including: hormonal effects and those related to the menstrual cycle, in addition to genes related to the immune system located on the X chromosome. However, The specific pathophysiological mechanisms of autoimmune bullous diseases and autoimmunity in general in women remain enigmatic.14
Within the context of pemphigus vulgaris specifically, one study found that female patients had a later age of onset as well as higher rates of mucosal disease compared to male patients.15 In this scenario, additional investigations are essential to better define gender-specific differences in mortality risk and autoimmune expression.
Regarding the age group, 90% of all cases of deaths from pemphigus in Brazil are in the age group over 40 years old, with the age group 80 years old and over representing 29% of all cases, corroborating studies showing that pemphigus can appear in any age group, but the majority of patients are between 45 and 65 years old at the time of diagnosis.16
The mean age of onset of the s subtype of pemphigus vulgaris was higher than that of several other autoimmune diseases, such as systemic lupus erythematosus, systemic sclerosis, and psoriasis, but sharing a similar age of onset to rheumatoid arthritis and Sjögren's syndrome, which they tend to occur in the mid or late 40s.17
About color/race, deaths from this disease were more frequent in whites with 52.2% of the sample, so that whites and browns account for the vast majority of deaths with 84.3% of the sample. Knowing that this is a multifactorial disease, so that geographic location, racial and ethnic differences combined with genetic factors can influence its incidence, a careful analysis in future work focused on specific racial groups becomes essential to define a more comprehensive scope. wide range of significant agents that interfere with the spectrum of pemphigus.18
Regarding education, pemphigus has a higher mortality rate in people with low education, especially in individuals with no or few years of education, reflecting family socioeconomic factors that are linked to access to health services, late diagnosis and untreated aggravating diseases. Furthermore, the information collected is in accordance with the literature, as stated by Barcelos et al.,19 that the predominant level of education is that of individuals with primary education.
About marital status, the greatest incidence in married individuals stands out, according to a study by Brandão, et al.,20 on immunobullous dermatoses, in which 64.3% have this marital status. Therefore, it is clear that deaths also follow this line, with higher prevalence in married people, followed by singles and widowers.
Regarding the place of occurrence, the vast majority died in hospital, justified by the pathophysiology of the disease, in which more severe cases present worse symptoms and complications, such as dehydration, nutritional difficulties and infections, which lead the patient to require intensive support. tertiary care, thus correlating the place of death with the highest occurrence with the most severe forms.19,21 Furthermore, deaths can also occur at home, but this is much less common, generally associated with difficulty in diagnosis and atypical manifestations, which mean that the patient does not seek health services or does not have a definitive diagnosis of pemphigus.22,23
Mortality from pemphigus in Brazil in the last two decades is increasing, presenting itself as a serious problem, especially in the Southeast and Northeast of the country, predominantly in women, between 40 and 80 years of age, in white people, with little or no education, mostly among married people, with places of death in the hospital environment. This study has the limitation inherent to its design, as it is an epidemiological study with a secondary database, therefore with the limitation of a study restricted to the variables available in the database, without allowing inferences of causal relationships, however, its data allow generate hypotheses for future studies, as well as subsidize data for public health actions. The epidemiological data found demonstrate the need for improvements in the approach to the pathology, making it necessary, therefore, to carry out more studies, especially field studies, which allow clinical monitoring of patients, which enable better recognition of the disease in the national territory, in addition to facilitate the structuring of policies that aim for a multidisciplinary approach for affected individuals, so that there can be better management of the condition.
None.
The authors declare no conflict of interest.
None.

©2024 Marques, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.