MOJ
eISSN: 2379-6383


Review Article Volume 4 Issue 6
Department of Epidemiologist IDSR, DHMT Western Area (U & R) Freetown, Sierra Leone
Correspondence: Muhammad Ali Raja, Department of Epidemiologist IDSR, DHMT Western Area (U & R) Freetown, Sierra Leone, Tel +232 (0)78301961
Received: February 01, 2016 | Published: September 21, 2016
Citation: Raja MA. Measles outbreak investigation report western area. MOJ Public Health. 2016;4(6):180–184. DOI: 10.15406/mojph.2016.04.00101
Measles is a febrile rash illness by a Morbillivirus of Paramyxovirus family. It is transmitted from human to human by airborne droplets. It is fourth leading cause of mortality in children <5years in many African countries. In the pre-vaccine era an estimated 130million cases occurred each year. At the World Health Assembly in 2005, an ambitious global goal for measles control was established as part of the Global Immunization Vision and Strategy document1 that is, to achieve a 90% reduction in measles mortality by 2010 compared with 2000.1
As of 2007, four of the six WHO regional offices have a measles elimination goal (AMRO, EURO, EMRO, WPRO) and two have a mortality reduction goal (AFRO, SEARO). It is in these latter two regions where most of the global measles deaths occur. Worldwide, since the year 2000, the estimated number of measles deaths has been reduced by 68%. However, despite this remarkable progress in controlling measles, there were an estimated 17million cases and 242 000 deaths in 2006.2 Approximately 145 700 people died from measles in 2013 and most of them were young children <5years age group.3
In 2005, the resolutions WHA58.3 adopted IHR (2005). IHR (2005) entered into force on 15 June 2007 in accordance with Article 59, replacing IHR (1969). IHR (2005) is legally binding for WHO 194 Member States including all 46 WHO Member States in the African region. Endorsement of the International Health Regulations (2005) highlighted the importance of timely detection and response to events that are of potential international public- health concern4 including measles.
Clinical case definition of measles is any person in whom a clinician suspects measles OR Any person with fever and generalized maculopapular (i.e. non-vesicular) rash, and cough or coryza (i.e. runny nose) or conjunctivitis (i.e. red eyes). A suspected outbreak of measles is defined as the occurrence of five or more reported suspected cases of measles in one month per 100 000 population living in a geographical area (e.g. district/ block).5 A confirmed measles outbreak is defined as the occurrence of three or more confirmed measles cases (at least two of which should be laboratory-confirmed; IgM positive) in a health facility/district/block (approximate catchment population of 100 000) in a month.
In susceptible children with Vitamin A deficiency and malnutrition measles may result in severe illness and associated bacterial illness. In children with Vitamin A deficiency it can lead to corneal scarring and blindness, in older children & adults it can lead to Encephalitis leading to chronic disability or death, it can also lead to severe pneumonia and diarrhea leading to high morbidity & mortality especially in developing countries like Africa. Outbreaks with high case fatality rates have been reported across the globe in areas with low immunization coverage and where the pool of susceptible population (unvaccinated or uninfected) increases.
According to Sierra Leone MoHS National EPI policy the measles vaccine is given after the age of 09months. When the vaccine is given at 9months the sero-conversion is 85 % when it is given at 12months sero-conversion is 90% and after 15months it is 95%. MoHS is taking appropriate steps to introduce the second measles dose in routine vaccination schedule after 15months of age.
After the implementation of IDSR in Western Area the DHMT was systematically collecting, analyzing and interpreting the surveillance information received from 116 PHUs. There was a considerable rise in suspected measles cases seen over the last 11 weeks (36-46). The samples were collected and sent to lab for laboratory confirmation. During the EVD outbreak the reference lab for western area (CPHRL LAKKA) was not testing the measles samples due to some technical reasons like deficiency of lab reagents etc. There was a huge backlog of samples that was accumulated at DPC and it was just recent (19 November 2015) that the results were out from lab to all districts including western area. Western Area received results of samples that were sent to lab from September till November. There were a total of 14 samples of suspected measles cases sent to lab from 10 September till 19 November 2015. Out of these 14 samples results for 11 samples was out and out of those 11 results 08 were IgM positive for measles antibodies giving a sample positivity rate of 72%. The result of 03 samples is still pending.
Soon after receiving the lab results the DMO for Western Area convened the Public Health Emergency Management Committee meeting. The committee assessed the situation and after using the IHR (2005) decision instrument the outbreak was notified to National Level considering its impact on public health. It was decided to review the existing resources to determine the need for additional resources. The DMO then formulated individual committees & sub committees for specific response activities. The district rapid response team was made alert and was asked to gather additional information from the reporting health facilities in order to have much clear evidence. It was decided that after a couple of days when the individual committees will finish the tasks of assessment and detailed analysis another PHEMC meeting will be held to monitor the situation and plan for final public health response.
The DHMT with technical support from World Health Organization started analyzing the data. Basic descriptive epidemiology was applied and available data was analyzed in terms of time, place & person to get the clear view of the situation.
Analysis by time
Following graph shows the # of suspected measles cases that were reported through IDSR system along with those that were investigated by the DSOs (Figure 1).
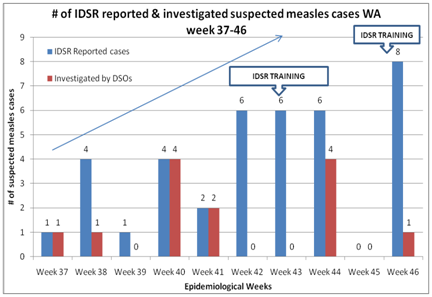
Figure 1 # of suspected measles cases that were reported through IDSR system along with those that were investigated by the DSOs.
The graph shows the # of suspected measles cases reported through IDSR from week 37-46 & those which were investigated. A total of 35 suspected cases were reported while 13 were investigated by DSOs. This difference in reported vs investigated cases can be attributed to the IDSR training rounds that were carried out from week 42 till week 46. During the trainings the DSOs were involved in facilitating the trainings resulting in non-response to the cases. The graph also shows considerable improvement in reporting as the IDSR trainings were cascaded showing improvement of health care providers in detecting the suspected measles cases and reporting them immediately to DHMT.
Following graph shows the number of samples that were sent to DPC for onward submission to CPHRL and the samples that tested positive. Current protocol is that district investigates the cases, collects the samples and submits to DPC. DPC then assigns the EPID # to the cases and submits the samples to the CPHRL (Figure 2).
The graph shows that the from week 37 till 46 a total of 13 samples were sent to lab out of which result came out for 11 samples out of which 08 were positive. The overall sample positivity rate remained quite high which was 72%. In week 37 & 38 the positivity rate was 100%, in week 40 it was 75% and in weeks 41 & 44 it was 50%.
Following graph shows the time taken by district RRTs to respond to alert after initial notification from the health facilities: (Figure 3).
The analysis shows that 87.5% [7] of the alerts were investigated within 24 hours of initial notification while 12.5% (1) of investigations were within 24-48 hours timeframe. It shows excellent capacity of district rapid response teams to respond to immediate notifiable diseases including measles.
Following graph shows the delay in days for feedback of lab results after the initial submission of samples: (Figure 4).
There was considerable delay in lab results after the initial submission of samples. Maximum delay was of 72 days while minimum delay was of 23 days.
Analysis by person
Following graph shows the analysis of positive cases by age groups: (Figure 5).
The graph shows various age groups those were affected. It is clear <5 years children were most affected 62.5% (5) followed by children between 5-10 years 25% (2) and least affected were children between 10-15 years age group 12.5% (1).
Following graph shows the analysis of positive cases by sex groups: (Figure 6).
It is evident that females are affected more than the males. 06 (75%) out of 08 positive cases are females while 02 (25%) are males. The prevalence of measles is more in females as compared to males. Further analytical studies are required to explore the cause.
Following graph shows the vaccination status of the measles positive cases according to information available on case investigation forms (Figure 7).
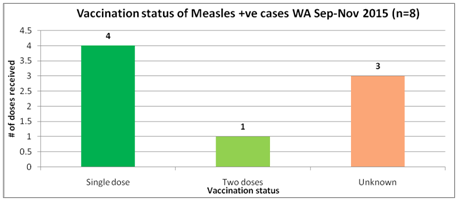
Figure 7 vaccination status of the measles positive cases according to information available on case investigation forms.
The analysis showed that 04 (50%) of the 08 positive cases had received single dose of MCV, 01 (12.5%) had received two doses while the vaccination status of 03 (37.5%) positive cases was unknown. The unknown vaccination status was due to unavailability of vaccination cards and parents difficulty in recalling about the MCV vaccine. For the case who received two doses of MCV can be due to receiving additional dose during SIAs.
Analysis by Place
The data showed that 06 wards in Western Area were affected by the outbreak. Out of these 06 wards 05 are in Western Urban (350,351,352,356 & 382) while one ward in Western Rural was affected (344). Following table shows the individual wards, reporting health facilities, ward population and attack rates: (Table 1).
The highest attack rate (0.03%) was seen in ward 344 which falls in western urban. The reporting health facility was Newton CHC and 03 positive cases were reported and all were from same location which was Catholic Farm Newton. Rest all the locations were from Western Urban with single positive case reported.
Following spot map shows the wards from where the measles cases were reported (Figure 8): Following table summarizes the locations from where the cases were reported: (Table 2). Following table shows the attack rates among various age groups: (Table 3).
District |
Ward |
Name of HF |
Population |
Reported cases |
AR % |
Western Urban |
350 |
Koya Town CHC |
10,093 |
1 |
0.009 |
Western Urban |
351 |
Wellington CHC |
34,460 |
1 |
0.002 |
Western Urban |
352 |
Phillip Street MCHP |
28,566 |
1 |
0.003 |
Western Urban |
356 |
Approved School |
38,696 |
1 |
0.002 |
Western Urban |
382 |
Gray Bush CHC |
11,191 |
1 |
0.008 |
Western Rural |
344 |
Newton CHC |
8,521 |
3 |
0.03 |
TOTAL |
131,527 |
8 |
0.006 |
Table 1 The individual wards, reporting health facilities, ward population and attack rates
Ward # |
Reporting Health Facility |
Address of Positive Case |
# Of Cases Reported |
350 |
Koya Town CHC |
14 Taylor Street Welington |
1 |
351 |
Wellington CHC |
1 Upper Taylor Street |
1 |
352 |
Phillip Street MCHP |
Phillip Street |
1 |
356 |
Approved School |
3 Sawyer Terrace |
1 |
382 |
Gray Bush CHC |
21 King Sillah Street |
1 |
344 |
Newton CHC |
Catholic Farm Newton |
3 |
Table 2 Locations from where the cases were reported
Age Groups |
Population |
Cases |
Attack Rates |
0-5 years |
23,280 |
5 |
0.002 |
5-9 years |
19,597 |
2 |
0.01 |
10-14 years |
15,125 |
1 |
0.006 |
Table 3 Attack rates among various age groups
The highest attack rate was in 5-9 year age group which 0.010 % was followed by 10-14 years which was 0.006 % and lastly 0-5 years which was 0.002%. (Total population at risk in all 06 affected wards is 131,527. The estimate for 0-5 year age group was taken to be 17.7%, for 5-9 years was 14.91% & for 10-14 years it was 11.53%. These population estimates are taken from MoHS Child Health/Expanded Programme on Immunization Comprehensive EPI Multi Year Plan 2012-2016 and from Demographics of Sierra Leone).6
MCH week activities
The upcoming MCH Week from 26-30 November is targeting 9months children who had not received MCV 1 in routine immunization (defaulters) and will also target all children 15-23months as an initial process of introduction of Measles Second Dose into the routine schedule.
Ring vaccination campaign
DHMT is planning to target all children between 10-14months and 2years to 15years age group in ring vaccination activities immediately after the MCH week. The ring vaccination will target the selective locations based on the risk assessment. The logistics required for this activity are being estimated and DPC will be informed soon about the resources required to carry out the activity.
All the Health Facilities In charges in western area were given briefing during the training for MCH week. All health facilities were asked to remain vigilant. Following actions were taken:
Information was also shared with WHO WAERC Team and following support was requested from all EPIs:
For appropriate case management Vitamin A capsules were made available to all health facilities especially the facilities reporting the cases. Apart from that antibiotics for treatment of complicated cases were also made available.
Enhanced social mobilization
Social mobilization activities should also be enhances as it is integral part of outbreak response to do risk communication to the affected communities. Communicating advice and guidance is the most important public health tool in managing risk. Following points should be remembered:
None.
The author declares no conflict of interest.

©2016 Raja. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.