MOJ
eISSN: 2379-6383


Research Article Volume 12 Issue 3
1Arsi University College of Health Sciences department of Public Health
2Oromia Regional Health bureau
Correspondence: Melese Tadesse, Arsi University College of Health Sciences department of Public Health, Tel +251913976496
Received: December 01, 2023 | Published: December 18, 2023
Citation: Tadesse M, Kaso M, Bekele D. Assessment of health problem and associated factors among flower farm workers in Ejere Woreda, West Showa Zone Oromia Regional State, Ethiopia. MOJ Public Health. 2023;12(3):162-172. DOI: 10.15406/mojph.2023.12.00427
Background: Floriculture is an agricultural sector that poses significant health risks, often due to unsafe work environments.
Objectives: The study aimed to assess health problems and associated factors among flower farm workers in Ejere Woreda, West Showa, Oromia, Ethiopia, in 2018.
Methods: A cross-sectional study incorporating quantitative and qualitative methods was conducted in Ejere Woreda from May 25 to June 30, 2018. A structured questionnaire was administered to 356 participants using simple and stratified random sampling, and qualitative data were gathered through in-depth interviews and observation checklists. Data were analyzed using EPI Info version 7 and SPSS 21. Descriptive statistics were computed, and the variables underwent binary logistic regression analysis, with a p-value < 0.3 for inclusion in multivariate logistic regression. Thematic analysis was applied to qualitative data.
Results: A total of 356 workers participated, with 296 (83.3%) reporting at least one health problem in the last 12 months. Among the conditions observed, headaches were the most prevalent (226, 76.4%), followed by musculoskeletal injuries (220, 74.3%), fatigue (206, 69.3%), respiratory injuries (185, 62.5%), dizziness (180, 60.8%), and skin injuries (17, 58.8%). Factors such as sex, job satisfaction, availability of personal protective equipment, and safety training showed significant associations with health problems.
Conclusion: The study revealed a high prevalence of health problems among flower farm workers, with job satisfaction, availability of safety training, and personal protective equipment shortages being significant factors. It is recommended that farm managements provide adequate safety training and full personal protective equipment to improve the health of workers.
Keywords: health problem, flower farm, farm workers
A health problem is defined as any personal injury, illness, disease, or death resulting from an occupational accident sustained by a worker in connection with the performance of their work.1 According to the International Labor Organization (ILO), over 2.3 million fatal and 313 million non-fatal occupational injuries are caused by occupational accidents and work-related diseases annually.2 Globally, 3 billion workers live without access to occupational safety and health services, with an estimated 250 million occupational injuries, 160 million work-related diseases, and 2 million worker deaths occurring each year.3 The economic impact of these issues is significant, with roughly 4% of gross national product due to workers compensation, loss of workdays, interruption of production, retraining, medical expenses and so on.4
Agricultural work is considered one of the most hazardous occupations in both developing and industrialized countries, with agricultural workers experiencing markedly higher rates of accidents and fatal injuries compared to workers in other sectors.5,6 Within the agricultural sector, floriculture stands out as a segment of horticulture concerned with the commercial production, marketing, and sale of various types of plants and flowers.7,8 In Ethiopia, the floriculture industry began to emerge in the late 1990s and has since become the second-largest flower exporter from Africa to the European Union (EU) after Kenya. The industry has created job opportunities for individuals with low educational levels and those living in poverty, contributing significantly to the country's foreign currency earnings.9
Despite its rapid expansion, the floriculture industry in Ethiopia faces environmental and occupational safety challenges. Environmentalists have reported excessive use of pesticides and chemical fertilizers, which not only have adverse effects on the environment but also pose risks to the health of workers in floriculture farms.6,10 Studies have shown that working in flower farms is associated with various health issues such as musculoskeletal problems, headaches, respiratory health problems, skin problems, kidney problems, fainting, and miscarriages.11 These health problems are linked to pesticide handling and the shortage of personal protective equipment (PPE), with poisoning injuries being particularly common among flower farm workers. The intense and acute pesticide exposures occur in closed plastic greenhouses without proper ventilation, further exacerbating the risks faced by workers. Additionally, inadequate use of PPE, lack of safety training, and prolonged exposure contribute to the high rates of occupational injuries in flower farm industries.6
Flower export plays a crucial role in Ethiopia's economy as one of the main sources of foreign exchange earnings. According to the Ethiopia Horticulture Development Agency (EHDA), the amount of foreign currency earnings from flower exports has been steadily increasing over the years.12,13
In a study conducted in Costa Rica, it was found that over 50% of flower workers experienced pesticide poisoning, while in Ecuador, the figure rose to 60%.14 Similarly, in Colombia, doctors in flower-producing regions have reported up to 5 cases of injuries per day according to the Victoria International Development Education Association.15 A comprehensive study across various floriculture farms in Ethiopia revealed that 76.5% of workers experienced fatigue, 73.4% suffered from headaches, 85.7% developed itchy rashes, 70.1% experienced eczema and a burning sensation, and 69.3% reported other related symptoms.6,16 Furthermore, cultivation activities have been closely linked to chronic respiratory symptoms such as cough, wheezing, bronchitis, and asthma. For instance, anhydrous ammonia (a fertilizer) has been associated with long-term lower respiratory tract illnesses, as well as symptoms of acute poisoning such as headaches, skin rashes, respiratory difficulties, eye injuries, dizziness, and even miscarriages.17 Prolonged hours of standing in the greenhouse and packing house have led to kidney injuries and other associated health issues among workers.5
Unfortunately, workers in flower farms are commonly exposed to dust, soil, sand, and clay, which can absorb organic dust particles, including pesticides released during groundwork.17 This exposure is exacerbated by the improper use of Personal Protective Equipment (PPE) and the lack of safety training, leaving workers directly susceptible to pesticides through skin contact, inhalation, and ingestion during their greenhouse work, packing, spraying, and irrigation activities.16,18
Conversely, the proper use of personal protective equipment and thorough training are vital components for ensuring the safety and well-being of workers in this industry.19 In Ethiopia, there are limited measures in place to control and improve workplace conditions, as indicated in Proclamation No. 377/2003, focusing on the working environment and its enforcement at the work sites.20
This study aims to provide critical information on the health issues and associated factors within the flower farming industry. This information is intended to serve as a tool for raising awareness across all levels, shedding light on gaps in existing policies and practices for the benefit of policymakers and managers. Furthermore, it is designed to contribute to the development of prevention strategies aimed at reducing morbidity, disability, and even fatalities among workers, essentially addressing the lack of available occupational health support within the floriculture sector while simultaneously promoting production opportunities.21,22
Study area and period
The study was carried out in the flower farms of Ejere woreda, within the West Showa Zone of the Oromia regional state in Ethiopia. This research was conducted during a period spanning from May 25, 2022, to June 30, 2022. Ejere woreda is situated approximately 48 kilometers away from Addis Ababa and encompasses 26 rural and 3 urban kebeles (small administrative units).
Data obtained from the Ejere woreda administration and the social and labor affairs office reflected the presence of seven flower farms P.L.C within the woreda, collectively employing a total of 2,034 workers. These farms are identified as Lenson Rose (Total = 1215, Male = 318 & Female = 897), Supper Flower (Total = 313, Male = 79 & Female = 234), Mini Plant Flower (Total = 50, Male = 9 & Female = 41), Joshua Flower (Total = 120, Male = 35 & Female = 85), Injorni Flower (Total = 88, Male = 19 & Female = 69), Green Horizon (Total = 109, Male = 24 & Female = 85), and Sheba Flower (Total = 139, Male = 42 & Female = 97).
Study design
A cross sectional study designs with quantitative by supplemented qualitative approach was conducted.
Source and Study population Source population
All flower farm workers found in Ejere woreda, West Showa Oromia regional state, Ethiopia
Study population
Selected flower farm workers in Ejere Woreda, West Showa Oromia regional state, Ethiopia.
Inclusion and exclusion criteria Inclusion criteria
The study encompassed all permanent or temporary employees directly involved in the production process within the selected flower farms. This inclusive scope involved individuals engaged in various tasks such as greenhouse activities, packhouse operations, chemical storage management, flower handling, as well as those involved in the spraying and irrigation processes. Specifically, the study targeted individuals who had worked for at least 12 months in the farm, covering both existing employees and those who had been transferred or newly hired but had also accumulated a minimum of 12 months of continuous work without a break. The rationale behind this inclusive approach stems from the assumption that individuals at this level of tenure and involvement within the flower farming operations have been substantially exposed to potential work-related injuries and health hazards. By including this range of workers, the study aims to capture a comprehensive understanding of the challenges and risks faced by those who have sustained significant exposure to the working environment over an extended period.23–25
Exclusion criteria
The study specifically excluded farms that had not been operational for the 12 months leading up to the research period. Additionally, individuals who were not directly involved in the production process, such as management staff, and others who were not directly engaged in activities like greenhouse work, pack house operations, chemical handling, and flower processing, were not part of the study cohort. The rationale behind this exclusion stems from the recognition that the nature of their work and the associated exposures may differ significantly from those directly engaged in the production process. The decision to exclude these individuals is founded on the understanding that their occupational exposures and potential health risks would likely differ from those encountered by employees directly involved in the hands-on production activities within the flower farms. By focusing exclusively on workers directly engaged in the production process, the study sought to maintain a specific and targeted focus on the unique challenges and health hazards faced by this particular group.
Sample size and sampling procedures
Sample size determination
There are two ways for calculation of sample size that based on the objective:
1st way for the first objective
By using single population proportion formula, based on study done on magnitude of occupational injuries and associated factors among small-scale industry workers in Mekelle city, northern Ethiopia show that the one year prevalence rate at least one occupational injuries among worker was 58.2%34 with 5% degree of precision, zα/2 is a standard z-score and 1.96 corresponding to 95% confidence interval (CI) the sample size is calculated.
= 378 or By Open Epi info version 2.3 = 378
then nf »»319+ 10% non-respondent = 356
Where
ni: Sample size calculated from infinite population (ni=378)
nf: Total sample size was studied (nf=356)
N: Source population (total workers =2034)
P: Proportion of occupational injured =58.2% at 95% confidence level (1.96) w: the margin error between the sample and the population = 5%
2nd Way for the second objective
To assess associated factors of Health problem, it was used double population proportion formula. Based on occupational induced health problems in sebeta surrounding floriculture workers6 by taking the most significant among factors and making assumptions as following: respondents who were used properly PPE as non-exposed (59.4% ) & who were not used properly PPE as exposed group (91.1%).
Where
Then when it’s calculating by Open Epi info version 2.3, the sample size was 68
= 68+ 10% non-response rate =75
At the end by using the above two sample size calculation, the larger one of the number had been sample size of this study. It was 356.
Sampling procedure Quantitative Data
Four farms were selected for the study using simple random sampling (lottery) from a total of seven farms in the Ejere woreda. The sample was allocated proportionally to the selected farms. Subsequently, within each selected flower farm, workers were stratified according to their departments using stratified random sampling. Once again, the sample was proportionally allocated based on the number of workers in each department, and a sample frame was created from worker attendance records. The workers were then selected using simple random sampling (Open Epi info Version 2.3) according to the inclusion and exclusion criteria. If a worker was absent or declined to participate during data collection, the next available worker was included in the study immediately. In the end, a sample size of 356 workers was obtained (Figure 1).
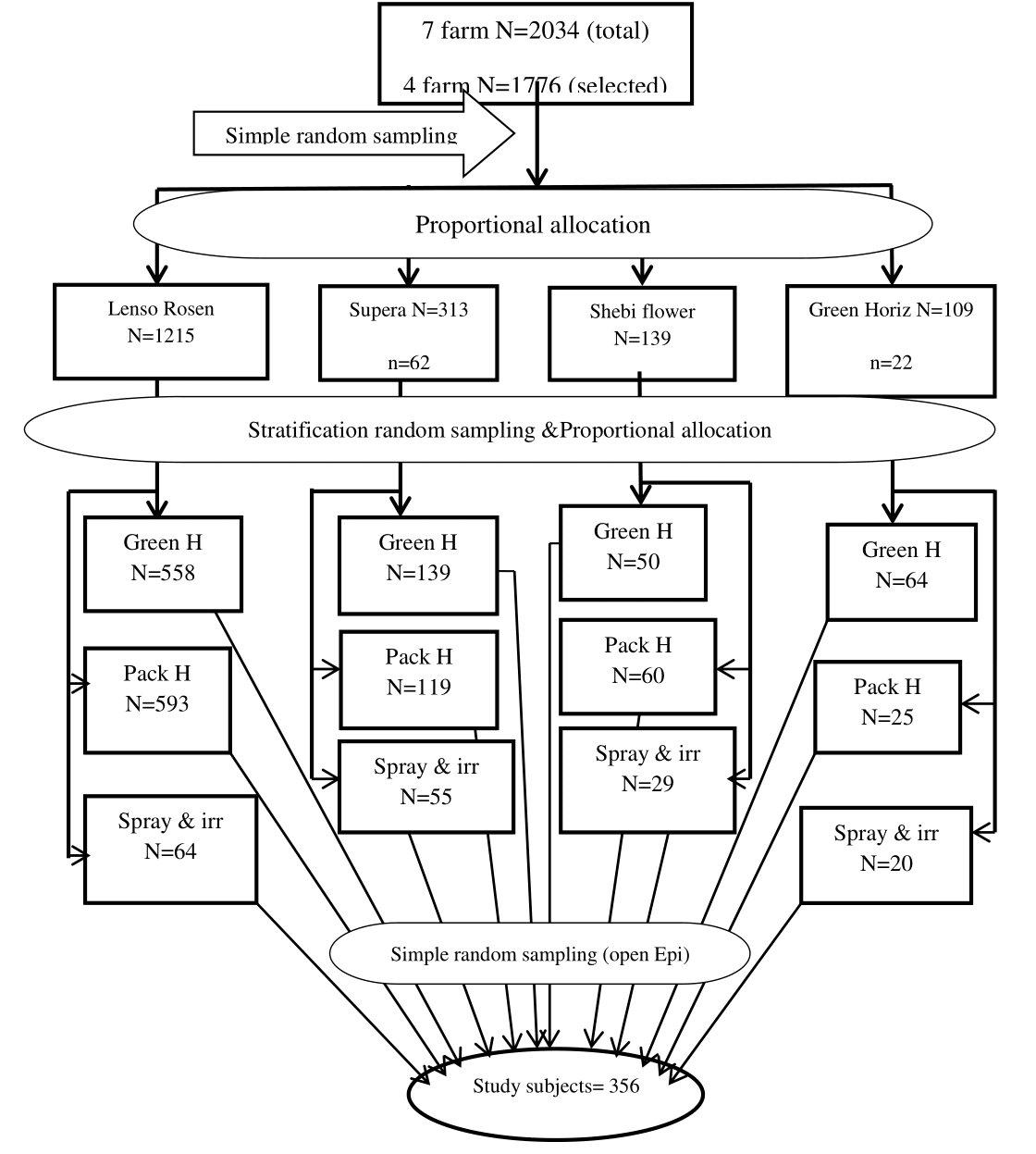
Figure 1 Schematic representation of sampling procedure of Assessment of health problem and associated factors among flower farm workers in Ejere Woreda, west Shoa zone Oromia regional state, Ethiopia/2022.
Qualitative data
Qualitative data collection involved individuals who were not part of the quantitative data. In-depth interviews were purposively conducted, selecting workers with over three years of experience in the production process. Fifteen subjects were included until information saturation was reached. Additionally, four selected flower farms were observed using an observational checklist. This approach aimed to gather information that cannot be quantified, thereby complementing the quantitative data.
Study variables
Dependent variable:
Independent variables:
Socio demographic variables:
Work environment variables:
Personal factors /Behaviors variable:
Institutional factor:
Data collection tool and procedures
Quantitative data were collected using a structured and pre-tested questionnaire that was based on related studies and available health risks in the workplace.16 Four data collectors and one supervisor, all health professionals, were recruited for data collection, and they received one day of training. To ensure contextual and terminological appropriateness, 10% of the questionnaires (42 in number) were pre-tested at an unselected flower farm (Joshua farm) in the Ejere woreda. After adjustments, the questionnaires were administered to the entire sample of workers. The questionnaire was initially written in English, translated into Afan Oromo by experts, and then translated back into English to ensure translation consistency. For qualitative data, an observational checklist was used to observe the working environment, and in-depth interviews were conducted to gather information on work environment issues. Key informants for the interviews were purposively selected based on their experience and position in the flower farm.
Data quality assurance
To ensure data quality in the study, appropriate and representative study units were selected, and maximum efforts were made to minimize bias and errors. These efforts included training data collectors and supervisors, as well as spot-checking and reviewing questionnaires on a daily basis by the principal investigator and supervisors. Additionally, pre-testing was conducted prior to the data collection process, and the questionnaires were prepared in English, translated into Afan Oromo, and then translated back into English to maintain consistency.
Data processing and analysis Quantitative data
After cleaning, the quantitative data was entered into Epi Info version 7 and then exported to the Statistical Package for the Social Sciences (SPSS) version 21 software for analysis in line with the study's objectives. The analysis focused on explanatory and response variables utilizing the software's capabilities. Descriptive analysis of the variables was conducted using frequencies and percentages, by categorizing all variables, and cross tabulation was performed using SPSS. To explore the association between determinants and occupational injury, a binary logistic regression analysis was conducted. In this analysis, the dependent variable was categorized as Health Problem (No=0, Yes=1). Variables identified as potential independent predictors in the binary logistic regression, with a p-value < 0.3, were entered into the multivariable logistic regression analysis to identify significant variables. Finally, the association between dependent and independent variables was assessed using odds ratios (OR) with 95% confidence intervals (CI), and a p-value less than or equal to 0.05 was considered statistically significant.
Qualitative data
The qualitative data was analyzed thematically and logically. Thematic analysis was employed to analyze the results of the in-depth interviews. The in-depth interviews were transcribed word by word after repeated listening and careful understanding. The transcribed data was then translated from Afan-Oromo language to English. The completed translations of the respondents' statements were broken down into similar topics, expressing the meaning of each respondent's input. Furthermore, the interviews with key informants were summarized by thematic areas corresponding to the topics in the quantitative results. This approach was taken to support and strengthen the findings, ensuring a comprehensive and well-rounded understanding of the data.
Ethical considerations
It's evident that the study adhered to rigorous ethical standards throughout its implementation. Ethical clearance from the Ethical Review Committee of Arsi University's College of Health Sciences Department of Public Health was secured, demonstrating a commitment to ethical research practices. Additionally, written permission was obtained from the Ejere Woreda administration, ensuring compliance with local regulations and demonstrating respect for community involvement in the study.26,27
The proactive communication and obtaining of permission from the owners of the flower farm prior to interviews and data collection activities further underscore the ethical approach. Written consent from each study subject was obtained after a detailed explanation of the study's purpose, the type of data being collected, the methods of data collection, and their full right to refuse or withdraw at any time without providing reasons, ensuring informed participation and respect for autonomy. The anonymization of study subjects by replacing names with codes on the questionnaire was a thoughtful measure to guarantee the confidentiality of the information provided. This approach is in line with best practices for protecting participants' privacy and confidentiality.
Furthermore, it's commendable that the interviewer took the time to inform the study participants about common causes and methods of preventing occupational injuries after completing the interview, thereby providing educational value and fostering a sense of care for the participants.28–30
Socio demography
The study included a substantial sample size, comprising a total of 356 individual workers from four selected flower farms, resulting in an impressive response rate of 100% for the quantitative data collection. This high response rate enhances the robustness and reliability of the study's findings.
In terms of demographic distribution, the majority of the respondents (306 individuals, accounting for 86%) were females, indicating a pronounced gender imbalance with a female to male ratio of 6:1. The mean age of the respondents was 24.65 years, with a standard deviation (SD) of 5.70 and a range of 30 years (17 - 47). Notably, a significant proportion (202 individuals, representing 56.7%) fell into the age category of less than or equal to 24 years old.31
Regarding educational attainment, the majority of the respondents (192 individuals, making up 53.9%) had completed primary school. The ethnic composition of the participants revealed that 336 individuals (94.4%) belonged to the Oromo ethnic group. Furthermore, a substantial portion (197 individuals, accounting for 55.3%) of the respondents were single in terms of marital status.
In the context of employment status, the study found that the majority of respondents (272 individuals, representing 76.4%) were permanent workers, while the remaining 84 individuals (23.6%) were categorized as temporary workers within the selected flower farms (Table 1).
Variable |
Category |
Frequency |
% |
Sex |
Female |
306 |
86 |
Male |
50 |
14 |
|
Age |
<=24 |
202 |
56.7 |
25 – 35 |
129 |
36.2 |
|
>35+ |
25 |
7 |
|
Religion |
Orthodox |
217 |
61 |
Catholic |
2 |
0.6 |
|
Protestant |
121 |
34 |
|
Muslim |
3 |
0.8 |
|
Others |
13 |
3.6 |
|
Educational level |
Can’t read and write |
8 |
2.2 |
Can read and write |
71 |
19.9 |
|
Primary school (1-8) |
192 |
53.9 |
|
Secondary school (9-12) |
65 |
18.3 |
|
Higher education |
20 |
5.7 |
|
Ethnicity |
Oromo |
336 |
94.4 |
Amhara |
19 |
5.3 |
|
Tigirie |
1 |
0.3 |
|
Marital status |
Single |
197 |
55.3 |
Married |
155 |
43.5 |
|
Divorced |
4 |
1.1 |
|
Residence |
Rural |
176 |
49.4 |
Urban |
179 |
50.6 |
|
Employee pattern |
Permanent |
272 |
76.4 |
Temporary |
84 |
23.6 |
|
Monthly salary in birr |
<=980 |
34 |
9.6 |
981- 1653 |
301 |
84.6 |
|
1654 -2326 |
11 |
3.1 |
|
>2327+ |
10 |
2.8 |
Table 1 Socio-demographic characteristics of selected flower farm workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018(n=356)
Note: Others: wakefata and religion name that not list in choose, <=: less than or equal
For qualitative data, fifteen key informant interviews were interviewed, and four flower farms were observed by observational checklist
Magnitude of occupational injuries
The data presented reflects a significant prevalence of health problems among the respondents within the 12 months preceding the study period. Specifically, 296 individuals (83.1%) reported experiencing at least one health problem during this time frame. Within this group, a substantial majority of 282 individuals (95.3%) indicated that these health problems developed after joining their current job, suggesting a potential association with the nature of their work or working conditions.
The types of injuries and health issues reported encompass a range of physical concerns, shedding light on the occupational health challenges faced by the respondents. Notably, a high proportion of individuals reported specific types of injuries or health issues, including skin injuries (171 individuals, accounting for 58.8%), musculoskeletal injuries (220 individuals, representing 74.3%), and respiratory injuries (185 individuals, making up 62.5%). Furthermore, a concerning number of respondents reported injuries related to specific organs or systems, such as kidney injuries (103 individuals, 28.9%), reproductive health injuries confirmed by a physician (34 individuals, making up 9.6%), and cancer cases confirmed by a physician (8 individuals, accounting for 2.2%). The data also indicates that among female respondents, a notable portion (22 individuals, 7.2%) reported experiencing miscarriages, with 10 of these cases (45.5%) being induced and 12 (54.5%) identified as spontaneous abortions. These findings signal potential reproductive health challenges among female workers, warranting further attention and investigation (Table 2).
Variables |
Category |
Frequency |
% |
Had occupational injured |
Yes |
296 |
83.1 |
No |
60 |
16.9 |
|
Onset of Injuries |
Before |
14 |
4.7 |
After |
282 |
95.3 |
|
Skin injures |
Yes |
171 |
58.8 |
No |
125 |
42.2 |
|
Musculoskeletal |
Yes |
220 |
74.3 |
No |
70 |
23.7 |
|
Respiratory injuries |
Yes |
185 |
62.5 |
No |
111 |
37.5 |
|
Had kidney conforming by physician |
Yes |
103 |
28.9 |
No |
253 |
71.1 |
|
Had cancer conformed by physician |
Yes |
8 |
2.2 |
No |
348 |
97.8 |
|
Reproductive health problem |
Yes |
34 |
9.6 |
No |
322 |
90.4 |
|
Any abortion /Miscarriage/ |
Yes |
22 |
7.2 |
No |
284 |
92.8 |
|
Frequency of miscarriage |
At once only |
20 |
91 |
Two and more than |
2 |
9 |
|
Type of abortion |
Spontaneous |
12 |
54.5 |
Induced |
10 |
45.5 |
|
Injuries workers had sick leave |
Yes |
113 |
38.2 |
No |
183 |
62.8 |
|
Duration of sick leave |
Till recovery |
11 |
9.7 |
Working on medication |
45 |
39.8 |
|
1-5 day only |
57 |
50.5 |
Table 2 Magnitude of Health Problem in selected flower farm among workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018(n=356)
Note: One respondent may have more than one injured
Among the health problems reported, 153 (51.7%) cases were related to itchy rashes, while 146 (49.3%) cases involved a burning sensation in the skin injuries. In terms of musculoskeletal injuries, back pain was the most prevalent, affecting 164 (74.5%) individuals, followed by lower extremity pain in 155 (52.4%) cases, arthritis/joint pain in 132 (44.6%) cases, and upper extremity pain in 126 (42.6%) cases. Furthermore, during working hours, the most commonly reported health issue was coughing, with 152 (51.4%) cases (excluding clearing throat or single cough). Chest tightness (breathing difficulty) was reported by 106 (35.8%) individuals, sneezing or blocked nose problems by 112 (37.8%) individuals, and asthma was the least common respiratory problem, affecting 21 (7.1%) individuals. Additionally, among the study participants in selected flower farms, the most prevalent health problem was headache, reported by 271 (76.4%) individuals, followed by fatigue in 247 (69.3%) cases, dizziness in 216 (60.8%) cases, and sleeping problems in 186 (52%) cases during work hours (Figure 2 – Figure 3).
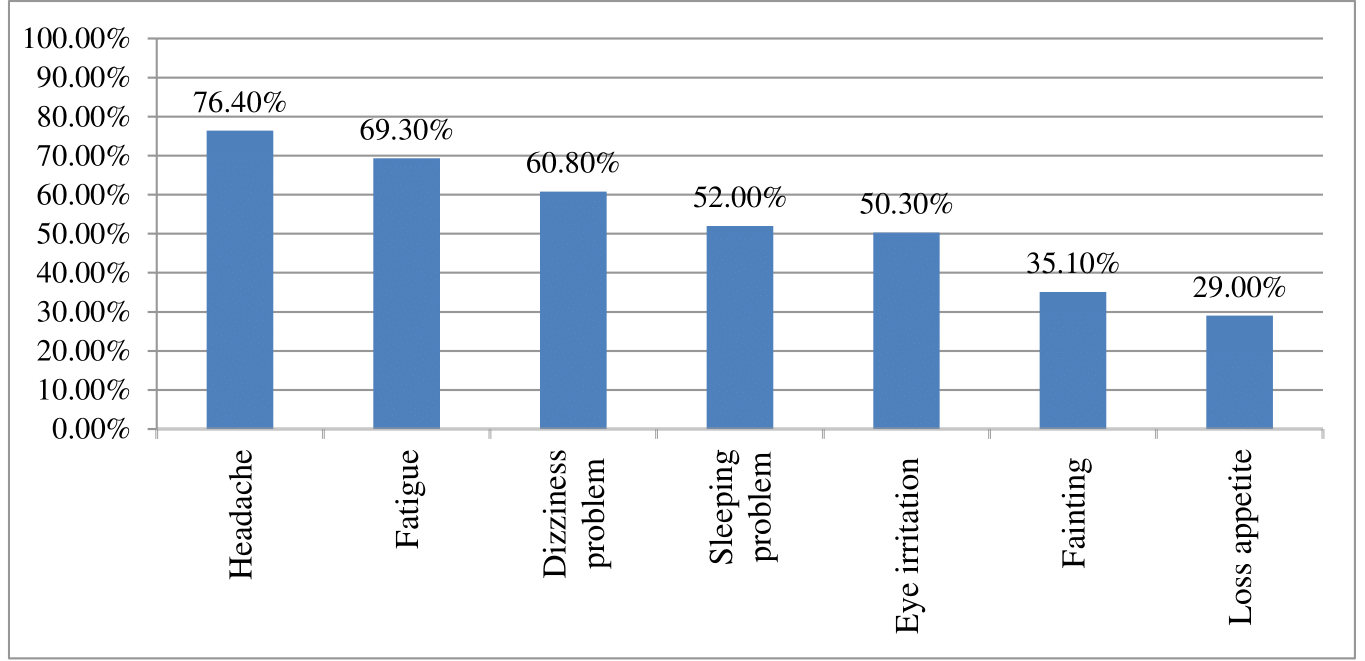
Figure 2 Prevalent of other Health Problem in selected flower farm among workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018.
Note: One respondent may have more than one injured
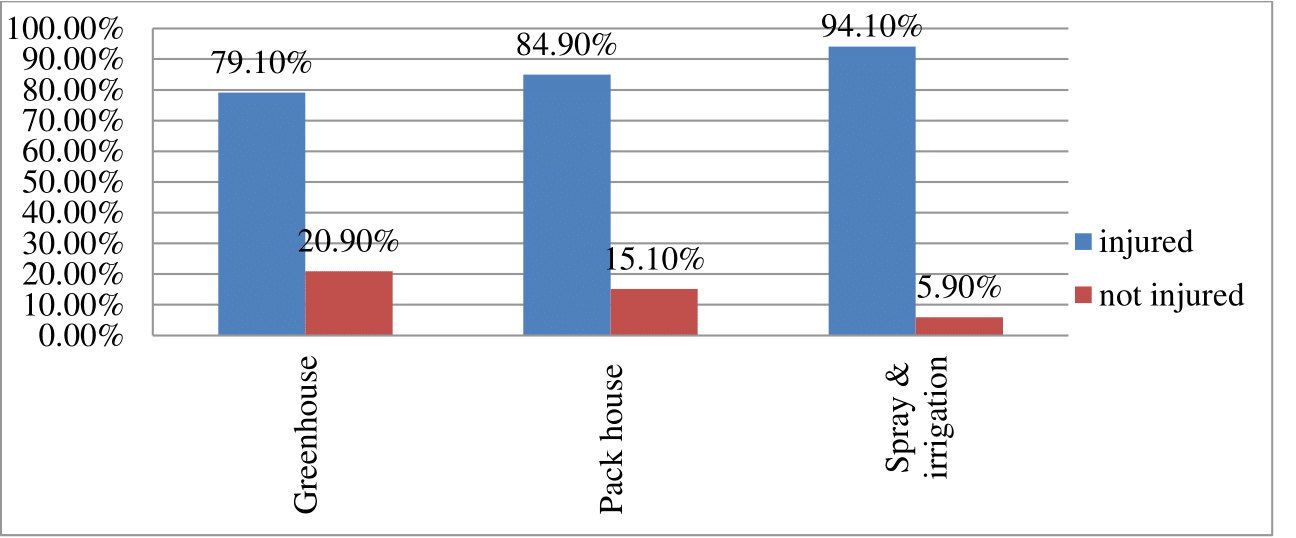
Figure 3 Prevalent of workers Health Problem in work section of selected flower farm among workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018.
Regarding physical body injured, out of the respondents192 (53.9%) were face injured, 173 (48.5%) were hand injured, 97 (27.2%) were legs injured, 55 (15.4%) were eye injured, 44 (12.4%) were ear injured and 14(3.9%) were other body parts injured.
Commonly observed health problem
As informative interviewees said that the commonly observed occupational Health Problem among flower farm workers like headache, skin injuries (itchy rash & burning), musculoskeletal injuries (back pain, upper extremity, lower extremity), eye irritation, respiratory injuries (especial, cough during work time, breathing difficult, sneezing or block nose), kidney injuries, fatigue, dizziness and fainting during work time.
As one respondent said that (Female and age = 31)
“previously I was healthy; after I join this work I feel chest tightness, cough, sometime during work feel eye irritation, back pain, from my nose watery fluid drops out, headache and burning sensation on my face during I wash.” From Green House
As one respondent (Female and Age =23)
“Before coming here I haven’t seen any illness on myself but when I entered in this compound, just come to me like eye irritation, fainting with dizziness and feeling to become fall down. It’s like as made of demon or evil.” From Pack house worker
Among the work section departments in selection flower farms, the most prevalent workers injured 94.1% were in spray & irrigation and followed by 84.90% were pack house & 79.10% were greenhouse respectively (Figure 4).
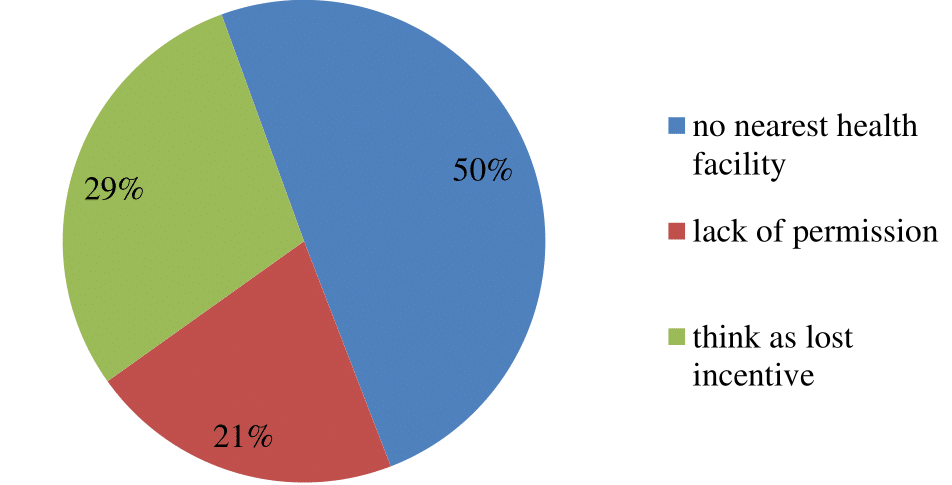
Figure 4 Reason of Health Problem workers was not visited health facility in selected flower farm workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018.
Out of Health Problem respondents, the medical coved 209 (70.6%) by their self and 87(29.4%) by farm whereas 110(37.2%) were visited health facility and 186 (62.8%) not visited health facility as reported in selected flower farm workers. Concerning the reason of Health Problem workers were not visited health facilities as reported, 93(49.7%) were not nearest to health facility, 39 (21%) were lack of permission and 54 (29.3%) were think as lost incentive salary (Figure 4).
Work environmental factor
In selected flower farm workers were described three work sections by the respondents. Those work section were 163 (45.8%) green house (include supervisory), 159(44.7%) pack house and 34(9.6%) spray and irrigation. Out of the respondents, 78 (21.9%) were directly used chemical hazard and 278 (78.1%) were used indirect at work place. Regarding service years mean of the respondents was 3.15±2.5 (SD) with range 12 years (minimum 1 and maximum 13)whereas more than half of respondent 212 (59.6%) were service years between 1 - 3 years, followed by5.1+ years were 76 (21.3%) and were 68 (19.1%) between 3.1- 5 years respectively. Similarly, the work hour of the workers in week the most of the respondents were reported 221 (62.10%) >48 hour and next 135 (37.9%) less than or equal to 48 hours in weeks.
Situation of work environment
The type of work performed in flower farms involves various tasks such as making flower beds, spraying chemicals, having close contact with soil mixed with chemicals, cultivating flowers in high temperatures, and dealing with dust. In situations where the greenhouse becomes dusty and excessively hot, workers are instructed to report it to their supervisors. The supervisors then prioritize the flowers by opening the greenhouse from the top to improve ventilation. However, during this time, the workers are not given permission to rest or leave the greenhouse.
One of the respondents, a 27-year-old female, described her experience as follows:
"I have personally observed the occurrence of health issues when I sweep the surface where the flowers grow (flower bed). The dust gets dispersed in the air, and due to the high temperature, I experience chest tightness, coughing, fatigue, and even fainting. Additionally, when I touch my skin, I feel a burning sensation and develop a rash." (Greenhouse worker)
Hygiene of work area
The workers who handle spraying tasks have reported that they wash their exposed body parts immediately after spraying and use plastic bags when mixing acids. These practices are implemented to minimize the potential hazards associated with the chemicals they handle. On the other hand, greenhouse workers have reported a lack of soap and insufficient shower facilities considering the number of workers. However, the workers involved in chemical spraying have access to adequate facilities to fulfill these requirements.
Workplace supervision and follow up
According to the informants, they are aware that regular support supervision takes place on a quarterly basis, and medical checkups are conducted as part of the occupational health and safety (OHS) regulations. However, it has been mentioned that there is a lack of regular work area supervision and periodic medical checkups due to the absence of a full-time OHS officer. Additionally, there is no health facility nearby to provide immediate medical attention and treatment for any injuries they may sustain.
Personal and Institutional factor
Among the respondents, a total of 302 individuals (84.8%) reported not properly using Personal Protective Equipment (PPE). The main reason cited by 199 individuals (65.9%) for not using PPE properly was that the PPE they had available was perforated or damaged. Additionally, 22 respondents (22.5%) reported a lack of awareness about the importance of using PPE, while 35 individuals (11.6%) stated that they were not comfortable wearing PPE.
Furthermore, among the respondents working in selected flower farms, 241 individuals (67.7%) reported a shortage of PPE. Additionally, 265 respondents (74.4%) expressed dissatisfaction with their current job, whereas 236 individuals (66%) reported not having received any training on occupational health and safety (Table 3).
Variable |
Category |
Frequency |
% |
Properly use of PPE |
Yes |
54 |
15.2 |
No |
302 |
84.8 |
|
Reason not use PPE |
Perforated |
199 |
65.9 |
Not comfortable |
35 |
11.6 |
|
Lack of awareness |
68 |
22.5 |
|
Shortage of PPE |
Yes |
241 |
67.7 |
No |
115 |
32.3 |
|
Satisfy with current job |
Yes |
91 |
25.6 |
No |
265 |
74.4 |
|
Drinking alcohol |
Yes |
111 |
31.2 |
No |
245 |
68.8 |
|
Smoke cigarette |
Yes |
21 |
5.9 |
No |
335 |
94.1 |
|
Occupational safety training |
Yes |
121 |
34 |
No |
235 |
66 |
Table 3 Personal and institution factors of selected flower farm among workers in Ejere woreda, west shoa Oromia, Ethiopia, 2018(n=356)
In selected flower farms, the shortages of PPE in type were reported as followed. Among the type of PPE provided for the workers, gloves 241(67.7%), coverall 195 (54.8%), boots 148 (41.6%), facemask 111 (31.2%) and goggles 68 (18.8%) were not availed in 12 months priority periods of the study.
Availability of personal protective equipment
The lack of availability of personal protective equipment (PPE) and the delayed replacement of perforated PPE were identified as significant contributors to health problems among farm workers during interviews.
One male respondent, aged 34 highlighted the issue, stating, "If protective equipment becomes perforated, it is not replaced promptly. For example, a colleague of mine had perforations in his gloves a year ago, and chemicals reached his skin, causing an injury. As a result, he had to seek repeated medical attention at St. Paulo Hospital." From Spray and Irrigation
Another respondent, a 22-year-old female, mentioned, "The gloves and boots provided for use are uncomfortable and ill-fitting. The gloves are too big and do not fit tightly around the fingers, making it difficult to work. As a result, I choose not to use them." From Green House Workers
Health & safety training
This lack of consistent health and safety training and support for farm workers is concerning, especially considering the potential health risks associated with pesticide exposure and other hazards in the agricultural industry. It's clear that there is a need for more comprehensive and accessible training programs that are regularly scheduled and available to all employees. Additionally, the issue of medical check-ups and monitoring for potential health issues related to chemical exposure should be addressed to ensure the well-being of workers. It's important for employers to take these concerns seriously and prioritize the health and safety of their employees.
Work environment observation
Overall, it is evident that there are significant gaps in the health and safety measures in place for farm workers, particularly in the areas of training, access to personal protective equipment, and medical facilities. It is crucial for farm owners and managers to prioritize the well-being of their employees and take proactive steps to address these issues. This may include implementing regular and comprehensive training programs, ensuring the availability of personal protective equipment, and providing access to medical care and facilities. Additionally, measures should be taken to ensure that all workers have access to proper sanitation facilities and that potentially harmful chemicals are used in a safe and responsible manner. By addressing these concerns, farm owners can create a safer and healthier working environment for their employees.
In conclusion, the study highlights the need for improved health and safety measures for farm workers, particularly in the areas of training, access to personal protective equipment, and job satisfaction. Addressing these issues is crucial for creating a safer and healthier working environment for farm employees. It is important for farm owners and managers to prioritize the well-being of their workers and take proactive steps to address these concerns. By doing so, they can help reduce the risk of injuries and health problems among their employees.32,33
Association factor
Binary logistic regression analysis
In binary logistic regression analysis, only independent variables like sex, age category, alcohol drinking, not satisfy with current job, shortage of PPE and lack of safety training were showed significant association with Health Problem but the rests insignificant.
The male respondents were 5.61 [OR: 5.61, 95% CI: (1.33 - 23.76)] times more likely to develop Health Problem than female respondents. The study participants who were not satisfied with their current job were 5.48 more likely to be injured than those satisfied worker [COR: 5.48, 95% CI: (3.05 -9.86)]. Similarly, the shortage of PPE was 2.48 [COR: 2.48, 95% CI: (1.4 - 4.40)] times more likely to developed injuries than full available of PPE. The findings revealed a significant association between workers who had not received occupational safety training and the occurrence of health problems. Those who had not undergone such training were four times more likely to develop health problems than their counterparts who had received proper occupational safety training (COR: 4.06, 95% CI: 2.27 - 7.24) (Table 4).
Variable |
Category |
Health Problem |
p |
COR (CI: 95%) |
||
Yes |
No |
|||||
Sex |
Female |
248(81%) |
58(19%) |
Ref |
||
Male |
48 (96%) |
2(4%) |
0.019 |
5.61(1.34 -23.76)* |
||
Age Category |
< = 24 |
159(78.7%) |
43(21.3% |
Ref |
||
25 -35 |
115(89.1%) |
14(10.9%) |
0.032 |
2.22(1.161-4.251)* |
||
35+ |
22(88%) |
3(12%) |
0.437 |
1.56(0.510 -4.732) |
||
Work section |
Green House |
129(79.1%) |
34(20.9%) |
|
Ref |
|
Pack house |
135(84.9%) |
24(15.1%) |
0.18 |
1.48(0.834-2.636) |
||
Spray and Irrigation |
32(94.1%) |
2(5.9%) |
0.056 |
4.22(0.962-18.482) |
||
Employment pattern |
Permanent |
222(81.6%) |
50(18.4%) |
|
Ref |
|
Temporary |
74(88.1%) |
10(11.9%) |
0.169 |
1.68(0.221-1.310) |
||
Educational level |
Can’t read and Write |
6(75%) |
2(25%) |
0.78 |
1.79(0.15 -4.06) |
|
Can read & Write |
62(87.3%) |
9(12.7%) |
0.135 |
1.81(0.83-3.96) |
||
Primary school(1- 8) |
152(79.2%) |
40(20.8%) |
|
Ref |
||
Secondary school(9-12) |
57(87.7%) |
8(12.3%) |
0.132 |
1.88(0.82-4.25) |
||
Higher education |
19(95%) |
1(5%) |
0.122 |
5(0.65-38.48) |
||
Alcohol drinking |
Yes |
100(90%) |
11(10%) |
0.021 |
2.27(1.13 -4.56)* |
|
No |
196(80%) |
49(20%) |
Ref |
|||
Satisfy with job |
Yes |
57(62.6%) |
34(37.4%) |
|
Ref |
|
No |
239(90.2%) |
26(9.8%) |
0 |
5.48(3.05-9.86)* |
||
Shortage of PPE |
Yes |
211(87.6%) |
30(12.4%) |
0.002 |
2.48(1.41 – 4.37)* |
|
No |
85(73.9%) |
30(26.1%) |
|
Ref |
||
Safety training |
Yes |
84(69.4%) |
37(30.6%) |
|
Ref |
|
No |
212(90.2%) |
23(9.8%) |
0 |
4.06(2.27-7.24)* |
||
Table 4 Summary of binary logistic regression of factors associated with occurrence Health Problem among flower farm workers in Ejere woreda, west showa Oromia, Ethiopia 2018(n=356)
*Significant at p-value <0.05, p: p-value, Ref: referent
Multi logistic regression analysis
After the bivariate logistic regression was done for each variable, to control confounder, unstable estimates in the subsequent models and to get more candidates variables for significant, only variables with P-value <0.3 were taken to a multivariate regression using backwards stepwise methods. The independent variable such as educational level, age category, work section, employment pattern and alcohol drinking did show insignificant association but sex, not satisfy with current job, shortage of PPE and lack safety training were showed significant association with Health problem. The male respondents were 5.54 [AOR: 5.54, 95% CI: (1.54 - 24.81)] times more likely to develop occupational injuries than female respondents. Similarly, among respondents not satisfy with current job was four [AOR: 4.30, 95% CI: (2.15-8.60)] times more likely to injuries than satisfy with current job. In other, shortage of PPE was three [AOR: 3.11, 95% CI: (1.62- 5.96)] times more likely developed injuries than available of PPE for workers. At the end, respondents who had safety trained 2.19 [AOR: 2.19, 95% CI: (1.09 - 4.39)] time more likely to prevented than respondents who had not safety training (Table 5).
Variable |
Category |
Health problem |
COR (CI: 95%) |
P |
AOR (CI: 95%) |
|
Yes |
No |
|||||
Sex |
Female |
248(81%) |
58(19%) |
1 |
ref |
|
Male |
48 (96%) |
2(4%) |
5.6(1.34 -23.76)* |
0.025 |
5.54(1.54-24.81)** |
|
Age Category |
< = 24 |
159(78.7%) |
43(21.3% |
1 |
ref |
|
25 -35 |
115(89.1%) |
14(10.9%) |
2.22(1.16-4.25)* |
0.056 |
2.47(1.18-5.16) |
|
35+ |
22(88%) |
3(12%) |
1.98(0.51-4.73) |
0.171 |
2.57(0.67-9.95) |
|
Work section |
Green House |
129(79.1%) |
34(20.9%) |
1 |
ref |
|
Pack house |
135(84.9%) |
24(15.1%) |
1.48(0.83-2.64) |
0.103 |
1.76(0.882-3.488) |
|
Spray & Irrigation |
32(94.1%) |
2(5.9%) |
4.2(0.96-18.48) |
0.591 |
0.558(0.66-4.68) |
|
Employment pattern |
Permanent |
222(81.6%) |
50(18.4%) |
1 |
||
Temporary |
74(88.1%) |
10(11.9%) |
1.7(0.22-1.31) |
0.502 |
1.17(0.63-2.57) |
|
Educational level |
Can’t read & Write |
6(75%) |
2(25%) |
1.10(0.53 -2.31) |
0.516 |
1.32(0.58-3.15) |
Read & Write |
62(87.3%) |
9(12.7%) |
1.53(0.67-3.55) |
0.446 |
1.443(0.56-3.71) |
|
Primary school (1-8) |
152(79.2%) |
40(20.8%) |
1 |
|||
Secondary school (9-12) |
57(87.7%) |
8(12.3%) |
1.68(0.69 -4.06) |
0.392 |
1.55(0.27-4.26) |
|
Higher education |
19(95%) |
1(5%) |
4.75(0.61-36.82) |
0.286 |
3.18(0.38-26.69) |
|
Alcohol drinking |
Yes |
100(90%) |
11(10%) |
2.27(1.13 -4.56)* |
0.511 |
1.33(0.58-3.04) |
No |
196(80%) |
49(20%) |
ref |
|||
Satisfaction with job |
Yes |
57(62.6%) |
34(37.4%) |
|
ref |
|
No |
239(90.2%) |
26(9.8%) |
5.48(3.05-9.86)* |
0 |
4.30(2.15-8.60)** |
|
Shortage of PPE |
Yes |
211(87.6%) |
30(12.4%) |
2.48(1.41- 4.37)* |
0.001 |
3.11(1.62-5.96)** |
No |
85(73.9%) |
30(26.1%) |
|
ref |
||
Safety training |
Yes |
84(69.4%) |
37(30.6%) |
|
ref |
|
No |
212(90.2%) |
23(9.8%) |
4.06(2.27-7.24)* |
0.027 |
2.19(1.09-4.39)** |
|
Table 5 Summary of multi logistic regression of associated factors with Health problem among flower farm workers in Ejere woreda, west showa Oromia, Ethiopia, 2018(n=356)
**Significant at p-value <0.05, p - p value, Ref -referent
One significant finding from the study underscores its primary objective: it is evident that workers in the floriculture industry experience health issues. Among the 356 participants, the majority – 296 individuals (83.1%)- reported experiencing at least one health problem prior to the study period. This percentage is lower than the outcomes of a study conducted in the flower farms surrounding Sebeta in Oromia, which revealed that 95.86% of workers had encountered at least one occupational health issue in the floriculture industry.6 The variance may be attributed to differences in sample size, improved awareness among workers compared to previous years, and the recent implementation of preventive regulations by various governing bodies.
However, our findings show a higher prevalence of health problems compared to studies carried out in Ecuador, where 60% of workers, and in small-scale industries in northern Ethiopia (Mekele), where 58.2% of workers, experienced at least one occupational injury.15,34 Among the identified health issues in our results, the most prevalent occupational injuries were musculoskeletal issues (74.3%), respiratory injuries (62.5%), skin injuries (58.8%), fatigue (69.3%), and headaches (76.4%). These figures diverge from a study in the East Shoa region of Oromia, where the predominant occupational health symptoms included skin problems (68.3%), musculoskeletal health problems (63.3%), and respiratory problems (45.5%), and a study in the Sebeta area, where 67.8% reported skin problems, 81.1% had respiratory problems, 76.5% experienced fatigue, and 73.4% reported headaches in the flower farms.6,17 Further findings revealed that among those injured, there were reports of coughing (51.4%), eye irritation (50.3%), fainting (35.1%), dizziness (60.8%), confirmed cases of kidney injuries diagnosed by a physician (34.8%), and reproductive health problems diagnosed by a physician (11.5%) within the selected flower farms. These values exceeded those reported in a study conducted in the special zone of Hollota, where coughing (36.6%), eye irritation (30%), and fainting (19%) were recorded, as well as in the East Shoa region of Oromia, where dizziness (26.2%), kidney injuries (23.3%), and reproductive problems (3.9%) were observed.11,17 These disparities may be attributed to working conditions that expose employees to poor ventilation, the use of damaged personal protective equipment, worker negligence, and a lack of occupational health and safety training.35
Qualitative findings from interviews supported these observations, revealing that working in closed spaces during chemical spraying, being exposed to excessive dust and high temperatures in greenhouses, and the improper use and infrequent replacement of damaged personal protective equipment were significant challenges in the flower farms. In support of these observations, a male spray worker recounted an incident where his colleague's punctured hand gloves, through which chemicals contacted his skin, resulting in injury. Despite seeking medical attention, the issue persisted due to the prolonged use of the compromised protective gear.
Similarly, a female worker in the greenhouse described experiencing chest tightness, coughing, fatigue, fainting, and a burning sensation on her skin after being exposed to dust while sweeping the flower beds in a high- temperature environment, subsequently leading to the development of a skin rash.
Of the female respondents, 22 individuals (7.2%) reported experiencing miscarriages, with 45.5% being induced and 54.5% being spontaneous. These figures are lower than those reported in a study conducted in Florida crop farms23 and in the Batu region of the Oromia regional state.36 This discrepancy may be attributed to improved awareness of youth-friendly services and increased access to family planning compared to previous years.
In the results, it was found that male respondents were 5.54 times more likely to experience injuries compared to female respondents [Adjusted Odds Ratio (AOR): 5.54, 95% Confidence Interval (CI): (1.24 – 24.81)]. This aligns with a study conducted around the Rift Valley farms in Ethiopia, which found that male workers were five times more likely to experience health problems than female workers on the farms [Adjusted Odds Ratio (AOR): 5.41, 95% Confidence Interval (CI): (1.53-19.11)].40 This observation may be due to male workers being assigned to work in areas involving chemical spraying and mixing, with male workers often being exposed to more hazardous and challenging work environments compared to their female counterparts.
Additionally, the findings revealed that 74% of workers expressed dissatisfaction with their current job, and those dissatisfied were 4.30 times more likely to incur injuries compared to those satisfied with their roles in the flower farm. Similarly, a study conducted in the Tendaho Agricultural Development S.C. in the Afar region state showed that 65.7% of respondents were dissatisfied with their current job and were more prone to injuries than those satisfied.3 This percentage is higher, potentially attributed to factors such as low wages and handling of workers, concerns related to potential chemical hazards, lack of nearby health facilities for treating injuries, and a shortage of sanitary facilities. An observational checklist highlighted that the four flower farms were not near health facilities, lacked comprehensive first aid kits, only provided shower facilities for chemical sprayers without considering other employees, and failed to provide an adequate number of gender-segregated latrines. Furthermore, some harmful chemicals were being used in the production process, including fertilizers, protection against pests such as mites, herbicides, protection against fungal infections, as well as in mixing chemicals and destroying non-essential eggs in the flower beds.
Furthermore, the findings demonstrate that participants who received no safety training were 2.64 times more likely to experience health problems compared to those who had undergone safety training. This observation aligns with studies conducted in Kenya11 and in the flower farms surrounding Sebeta in the Oromia region state.6 This similarity may be attributed to the low priority given to policy implementation in both countries, the negligence of farm owners in providing adequate support for their employees, and a lack of efficacy in worker representation bodies advocating for employee rights. Qualitative insights from interviews bolster this notion, revealing a discernible absence of training and orientation programs on health and safety for new workers upon their hiring, with only partial guidance provided by supervisors or more experienced workers.
Furthermore, the shortage of Personal Protective Equipment (PPE) was associated with a threefold higher likelihood of developing health problems compared to the situation where PPE was fully available for workers [Adjusted Odds Ratio (AOR): 3.12, 95% Confidence Interval (CI): (1.62 - 5.96)]. This figure exceeds the results of a study on occupational exposure to pesticides and associated health problems in Kenya's floriculture industry, which found that having inadequate PPE was linked to a twofold increase in disease symptoms,37 as well as a study in the Sebeta surrounding flower farms where the absence of PPE was linked to a twofold increase in disease symptoms.6 This disparity may stem from farm owners' neglect in providing sufficient PPE, with their focus primarily on profit margins, a lack of oversight from regulatory bodies, and workers not proactively requesting PPE when supplies are depleted. An observational checklist revealed that chemical sprayers were unable to properly use personal protective equipment due to the farms' insufficient and incomplete provision of PPE and workers' failure to request it.38–40
Strengthen
The study utilized both quantitative and qualitative methods as a means to triangulate information and delve into ideas not fully addressed by the quantitative approach alone. Additionally, the study found that the participants exhibited a 0% non-response rate, indicating a high level of engagement and participation among the individuals involved.
Limitation
The study did not employ any chemical or physical examination tests for the outcome or exposure variable. Solely relying on respondents' answers to questionnaire items administered by the interviewer may result in potential overestimation or underestimation of the findings. Recall bias may also be a factor, given that respondents were asked to recall injuries that occurred within the 12 months preceding the study period. The use of a cross-sectional study design makes it challenging to establish cause-and-effect relationships. Furthermore, due to the limited availability of comparable studies within the country, conducting comprehensive comparisons poses a significant challenge.
Workers at flower farms reported a substantial number of health problems in the 12 months preceding to data collection, according to this study's responder. The most common problems among those affected were headaches (76.40%), followed by back discomfort (55.4%), itchy rashes (51.70%) from skin injuries, and cough injuries (51.4.5%) from respiratory injuries in the musculoskeletal injury category. Alternatively, among the occupational factors of working in flower farms, sex, lack of PPE, job dissatisfaction, and lack of safety training have all showed a significant association with the development of occupational injuries. Conversely, other variables such as improper PPE use, alcohol consumption, work section, age category, and service years have demonstrated an insignificant association with health problems. Qualitative data essentially revealed various often encountered health problems as well as the factors that contributed.
First of all, we would like to thanks Arsi University College of Health Science for giving us permission to conduct this research. Our thanks goes to our colleague of Public health department for their guidance, constructive comments and technical support from the proposal development till writing this thesis.
Next, we are grateful for Oromia Health Bureau for their financial supporting for data collection of the study. Furthermore, our acknowledgment goes to Ejere Woreda, Farm administration and staffs of each farm that facilitate and helped us a lot in the process of data collection. It is also our pleasure to acknowledge all study participants for their willingness to participate in the study.
Last but not least, we would like to Thanks Arsi University public Health Post Graduate library for their facilitating internet accessibility.
The author declares there is no conflict of interest.

©2023 Tadesse, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.