MOJ
eISSN: 2379-6383


In the United States, graduate medical education has relied heavily on financial support from the Federal government through Medicare funds. In an attempt to reduce the national debt, much of this funding is at risk of being drastically cut. Additionally, the US government needs to address a growing shortage in primary care physicians that is likely to be exacerbated by implementation of the Affordable Care Act. From the perspective of the Association of American Medical Colleges and considering three primary stake holders-namely, patients, physicians and Medicare-this paper examines an alternative to these cuts by offering a compromise: AAMC teaching hospitals will use Medicare funding to increase the number of primary care residency positions in lieu of the subsidy of indirect medical expenses. This proposed policy would increase the annual output of primary care physicians by 15,000 each year and Medicare would not reduce financial support of graduate medical education at AAMC teaching hospitals.
Keywords: graduate medical education, association of american medical colleges, federal funding, medicare, resident training
ACA, affordable care act; AAMC, association of american medical colleges; CMS, centers for medicare and medicaid services; DME, direct medical expense; EMR, electronic medical records; GDP, gross domestic product; GME, graduate medical education; HHS, department of human health services; IME, indirect medical expense; IIPCP, incentivizing and increase in primary care physicians; IPAB, independent payment advisory board; PCPs, primary care physicians; ROI, return on investment
Introduction to GME funding
Graduate Medical Education (GME) is a term used to describe the formal training, usually hospital-based, that is pursued after obtaining a medical doctorate. The federal government is the largest supporter of GME subsidization, which is funded through Medicare. This funding is divided into two categories: “direct payments to pay the salaries of the residents and the supervising physicians’ time; and indirect payments to subsidize other hospital expenses associated with running training programs, such as longer inpatient stays and more use of tests”.1 In recent efforts to cut federal spending, the Obama administration has proposed a$60billion dollar reduction in GME funding over the next decade that “could result in serious access issues for patients in need of care”.2 “Other issues at stake include whether or not the nation is training enough doctors or other health professionals”.1 Between direct medical expense (DME) and indirect medical expense (IME) federal funding, IME funding is the most at risk of a “draconian” cut.1 This initiative, IIPCP, intends to redistribute $6billion dollars spent on IME funding from Medicare each year to specifically fund 15,000 new primary care residencies with in AAMC teaching hospitals across the United States. The IIPCP would use IME funding to address the increase in need of primary care physicians (PCPs) as an alternative to the drastic cut to Medicare GME support. The purpose of this paper is to evaluate the IIPCP initiative from the perspective of the Association of American Medical Colleges (AAMC) and three primary stakeholders- namely, consumers, physicians and Medicare.
AAMC
Introduction to the AAMC: The AAMC is a nonprofit organization based in Washington D.C. Established in 1876, the AAMC represents 141 accredited medical schools and 400 teaching hospitals and systems. By way of representing these institutions, the AAMC indirectly represents 128,000 faculty members, 75,000 medical students and 110,000 resident physicians.“Through its many programs and services, the AAMC strengthens the world’s most advanced medical care by supporting the entire spectrum of education, research and patient care activities conducted by our member institutions”.3
AAMC stakeholder profile: The AAMC represents all of the accredited medical schools and teaching hospitals in the United States (141 and 400 respectively); thus, its key stakeholders consist of the employees of these institutions (including the hospital executives), 128,000 faculty members, 75,000 medical students and 110,000 resident physicians.4 Additionally, every employee at the AAMC member institutions is affected by the fiscal success or failure of the organization in which they are employed. On a broader level, Americans seeking healthcare are also stakeholders because they rely on the success of AAMC teaching hospitals to deliver many of their healthcare services.
AAMC current structure: The AAMC is governed by a 17-member Board of Directors:
Chair: Valerie N Williams, Ph.D., M.P.A., Vice Provost for Academic Affairs and Faculty Development, University of Oklahoma Health Sciences Center
Chair-elect: Lorris Betz, M.D., Ph.D., Senior Vice President Emeritus of Health Sciences, University of Utah
Immediate past chair: Mark R. Laret, Chief Executive Officer, University of California, San Francisco Medical Center
President and CEO
Furthermore, each medical school has a primary and up to three alternative students, who participate in the Organization of Student Representatives. Professional development groups, advisory panels and special-issue task forces sponsor more than 70 meetings each year.
AAMC market size: Annually, over 400million Americans visit teaching hospitals for specialized surgeries and other complex treatments. These teaching hospitals serve as leaders in life-saving services such as trauma and burn centers. They are also in the forefront of research, innovation and training over 100,000 physicians each year. The AAMC members, at its 400 teaching hospitals, represent: “47 percent of all organ transplant centers; 60 percent of all level-one trauma centers; 67 percent of all burn beds; 22 percent of all cardiac surgeries; 41 percent al Alzheimer’s centers and provide nearly half of all hospital charity care nationwide”.4 According to a 2009 initiative that the AAMC implemented to measure the economic impact of AAMC members, the combined economic impact on the United States equaled $512,286,592,095. The economic impact is measured in the form of a direct business volume of $222,733,300,911 and an indirect economic impact of $289,553,291,184 that is estimated using a multiplier of 2.3. This means, “For every dollar directly spent by a medical school or teaching hospital, an additional $1.30 is indirectly generated for a total impact of $2.30”.5 In addition to business volume, the AAMC member institutions accounted for more than 3.3million full-time jobs. Furthermore, the AAMC member institutions generated more than $22billion in state tax revenue generated through income taxes and sales tax, corporate net income tax and capital stock/franchise taxes5 (Table 1).
States |
State Rank |
Total Economic Impact |
Total |
Total Government |
New York |
1 |
$ 69,365,955,031 |
476,240 |
$ 3,359,078,175 |
Pennsylvania |
2 |
$ 42,111,601,119 |
257,824 |
$ 1,853,816,983 |
California |
3 |
$ 41,644,267,579 |
234,862 |
$ 2,021,755,594 |
Massachusetts |
4 |
$ 32,310,974,785 |
184,049 |
$ 1,508,196,323 |
Texas |
5 |
$ 31,566,102,793 |
210,501 |
$ 968,186,757 |
Ohio |
6 |
$ 27,197,352,694 |
200,094 |
$ 876,546,659 |
Illinois |
7 |
$ 25,450,786,398 |
147,156 |
$ 805,253,886 |
Michigan |
8 |
S 24,193,228,100 |
150,962 |
$ 1,261,661,489 |
Florida |
9 |
$ 19,439,944,164 |
147,029 |
$ 977,886,813 |
North Carolina |
10 |
$ 15,049,651,900 |
112,973 |
$ 588,668,923 |
New Jersey |
11 |
$ 12,979,569,543 |
80,283 |
$ 505,203,940 |
Maryland |
12 |
$ 11,875,337,024 |
75,080 |
$ 649,667,988 |
Missouri |
13 |
$ 11,595,798,281 |
76,539 |
$ 354,347,561 |
Georgia |
14 |
$ 10,912,119,779 |
81,632 |
$ 218,562,088 |
Tennessee |
15 |
$ 10,625,599,180 |
76,403 |
$ 316,496,724 |
Virginia |
16 |
S 9,911,458,631 |
66,514 |
$ 321,133,221 |
Connecticut |
17 |
$ 8,649,070,534 |
60,080 |
$ 428,182,473 |
Wisconsin |
18 |
$ 8,485,257,185 |
42,799 |
$ 403,157,556 |
Minnesota |
19 |
$ 8,430,426,634 |
65,430 |
$ 495,554,749 |
Indiana |
20 |
$ 7,964,823,326 |
52,025 |
$ 274,821,274 |
South Carolina |
21 |
$ 6,937,400,208 |
35,510 |
$ 301,059,857 |
Arizona |
22 |
$ 6,342,395,460 |
41,332 |
$ 373,060,978 |
District of Columbia |
23 |
$ 6,253,916,710 |
44,639 |
$ 843,889,342 |
Louisiana |
24 |
$ 6,088,577,583 |
39,099 |
$ 194,108,159 |
Alabama |
25 |
$ 5,233,789,818 |
33,262 |
$ 227,203,499 |
All Other States |
$ 51,671,187,636 |
360,284 |
$ 2,402,320,695 |
|
US Total |
$ 512,286,592,095 |
3,352,604 |
$ 22,531,821,705 |
|
Table 1 Summary of Economic, Employment and Government Revenue Impact for RAMC Members, 2008
*Table from Umbach, 2009
AAMC values: The AAMC addresses their key values in terms of “areas of impact”. Through these areas of impact, they strive to promote: “A continuum of medical education that inspires learners to serve the public, promote health and improve care. A sustainable health care system in which academic medicine plays a unique and important role. New knowledge throughout the full spectrum of medical research that improves the health of all. A culturally competent, diverse and prepared health and biomedical work force that leads to improved health and health equity”.3 The AAMC states that their cultural values that drive their decision-making and action include innovation, collaboration and excellence.
AAMC vision/mission: The AAMC’s vision is clearly stated on the AAMC website as: a healthy nation and world in which: “America’s system of medical education, through continual renewal and innovation, prepares physicians and scientists to meet the nation’s evolving health needs. The nation’s medical students, biomedical graduate students, residents, fellows, faculty and the health care workforce are diverse and culturally competent. Advances in medical knowledge, therapies and technologies prevent disease, alleviate suffering and improve quality of life. The nation’s health system meets the needs of all. Concern for compassion, quality, safety, efficacy, accountability, affordability, professionalism and the public good guide the health care community. Medical schools and teaching hospitals continually earn the trust and support of the public for their special missions”. Likewise, their website mission statement reads: “The AAMC serves and leads the academic medicine community to improve the health of all”.
Consumer/patient
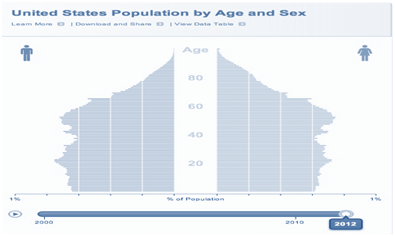
Introduction to the consumer: According to the Census Bureau’s population clock, there are approximately 317million people who make up the US patient/consumer population, making the US the third most populated country in the world. When looking at the birth rate compared to the death rate, this number is growing at net gain of 1 person every 16seconds.6 Along with a population that is rapidly growing, the US is experiencing an aging population. In fact, the number or older persons will likely grow by 135% by the year 2050. Furthermore, the portion of the population over the age of 85 is projected to increase by 350%.7 With an aging population comes an increased utilization of healthcare services and a shift from treating acute conditions to managing long-term chronic disease. Figure 1 represents the US population distribution by gender and age. Not only is the American patient population aging and increasing in size, but there is also a marked shift in treatment needs from acute to chronic conditions. Seventy-five percent of all healthcare spending is related to the treatment of chronic disease and approximately 1 in 2 adults have at least one chronic disease.8 The implementation of the Affordable Care Act (ACA) will potentially increase the number individuals covered by health plans by means of increasing the cost-pool with younger, healthier patients; however, the consumer’s expectations in regards to availability and quality of care remains constant. Thus, it will be imperative to find a solution to meet the increase in demand for primary care.
Consumer market size: Patients in the US spend an average of $8,680 per person per year on health care equaling an aggregate $2.7trillion dollars. This makes the US the most expensive country in the world based on healthcare dollar spent per person. Furthermore, healthcare spending is 17.9 percent of gross domestic product (GDP). Of this $2.7trillion dollars, hospital care and physician services were the two largest contributing categories totaling 850.6billion and 541.4billion respectively. From an aggregate perspective, Medicare, Medicaid, or private health insurance pays the majority of consumer healthcare costs, with a minority coming from out-of-pocket payments. Medicare, the largest contributor the healthcare spending, pays$554.3billion and accounts for 21 percent of national health spending. Medicare’s total healthcare spending increased 4.3 percent from 2010. Medicaid was the second largest contributor to health spending at $407.7billion. Private health insurance spending increased by 3.8 percent. Finally, out-of-pocket spending increased by 2.8 percent to $307.7billion which can be attributed to higher cost-sharing and an increased level of enrollment in consumer-directed health coverage plans.9
Consumer values/ expectations: Consumer healthcare expectations come in the form of three values: access, quality and cost. These three values are interrelated and have been coined in several industries as the “iron triangle” one aspect cannot be changed without affecting the other two (Figure 2) the “iron triangle of healthcare” is visualized. Thus, at the brink of the ACA implementation, with cost and access being the two areas most affected, it is natural for the consumer to become most concerned with how this will impact the quality of health care they receive.
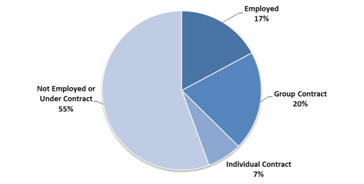
Physician
Introduction to the physician: There is a growing trend of physicians and physician offices merging and becoming part or larger networks, such as hospital systems, insurance companies and management firms. Many of the ACA provisions have spurred a closer financial and practice affiliation between physicians because of a desire to maintain negotiating power. Furthermore, many hospitals have been hiring more physicians as full-time employees to ensure that they are adequately staffed for the growing influx of new demand created, in part, by the ACA.10 Figure 3 depicts the share of physicians employed by hospitals.
Physician profile: The ratio of primary care physician to specialty physician is approximately 1:2, which has been criticized as not being in line with the physician needs of the US population. The majority of US physicians have completed fouryears of medical school and a minimum of threeyears residency. Based on the investments required for this type of educational training, physicians argue that specialty positions are more financially incentivizing than the primary care position alternatives. Table 2 lists the average physician compensation by specialty in 2010. In terms of overall physician supply, the federal Health Resources and Services Administration projects a deficit of 55,000 to 150,000 physicians by the year 2020.10
Physician Compensation |
2010 |
Change From 2009 |
Family Practice |
$ 189,402 |
2.94% |
Internal Medicine |
$ 205,379 |
4.21% |
Pediatric/Adolescent Medicine |
$ 192,148 |
0.39% |
Anesthesiology |
$ 407,292 |
-3.83% |
Cardiology: Invasive |
$ 500,993 |
3.97% |
Dermatology |
$ 430,874 |
4.16% |
Emergency Medicine |
$ 277,297 |
5.65% |
Gastroenterology |
$ 463,955 |
-0.33% |
Hematology/Oncology |
$ 382,934 |
3.78% |
Neurology |
$ 249,867 |
5.02% |
Obstetrics/Gynecology |
$ 281,190 |
-0.51% |
Orthopedic Surgery |
$ 514,659 |
3.71% |
Psychiatry |
$ 200,694 |
3.88% |
Pulmonary Medicine |
$ 300,019 |
4.07% |
Radiology: Diagnostic |
$ 471,253 |
-1.58% |
Surgery: General |
$ 343,958 |
2.34% |
Urology |
$ 372,455 |
-4,66% |
Table 2 Physician Compensation by Specialty
Source: Medical Group Management Association.
Physician market size: There are 972,376 physicians and medical residents within the United States. The majority of these physicians still operate in a decentralized network of private practice offices; however, this is quickly changing as the number of doctors on hospital payrolls, from 2000 to 2010, increased by 32%. This “cottage industry” approach to medicine has been criticized as one of many reasons for inefficiencies in our healthcare system. Additionally, although 20% of physicians are employed by hospitals, over one-half of graduating medical residents in 2010 took jobs at hospitals. From a financial perspective, payments to physicians accounts for approximately 20% of medical spending; however, physicians direct approximately 90% of total health care spending via referrals, tests and hospital admissions.10
Physician values: According to the author of The Five Core Virtues of the Modern Physician, there are several virtues/values to which the ideal physician dedicates himself/ herself. These include excellence, compassion, loyalty, fortitude and honesty.11 As the healthcare landscape continues to evolve, physicians value a system that promotes a landscape where they can adhere to their basic values without losing their voice in the system. Physicians do not always believe that more comprehensive coverage equals more comprehensive care and sometimes it comes at the expense of one or more of their values.
Physician expectations: In the 2013 Physician Practice Preference and Relocation Survey, an annual survey of over 2,500 doctors, surveyors found that “in an era when hospitals are competing on a national level for every physician they hire, practice preferences can be very helpful in composing a recruiting strategy and compensation package that will stand out and attract doctors”. The survey also determined that “Physicians were generally dissatisfied with their incomes in 2012 and blame declining reimbursements and administrative hassles as major factors in their stagnant compensation”. In addition to financial expectations, the survey found that “physicians want greater involvement in hospital decision making and desire services that facilitate their practice of medicine”.12 Medicare Introduction to medicare: Created in 1965, Medicare is a social insurance program that offers access to health insurance for patients who meet certain criteria regardless of income or medical history. The entitlement program offers health coverage through four parts-Medicare parts A, B, C and D which provide coverage for hospital care, medical care, supplemental care and prescription drugs, respectively. Medicare is funded by several sources including payroll taxes, premium payments and surtaxes added to premium payments. Medicare is operated by the Centers for Medicare and Medicaid Services (CMS) and is part of the Department of Human Health Services (HHS). In 2010, CMS realigned their organizational structure as shown in Figure 4. Although Medicare is operated under the CMS division of HHS, the Social Security Administration is responsible for determining Medicare eligibility and collecting some premium payments (Figure 5).
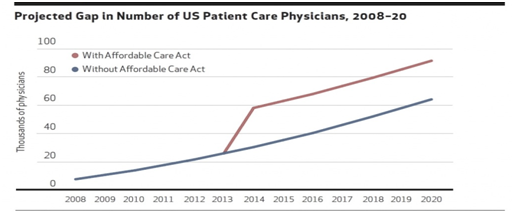
Figure 5 Projected Gap in number of US Patient Care Physicians, 2008-20.20
Note: Numbers shown represent gap between projected number of physicians needed and supply.
Medicare market size: There are approximately 50.7million total Medicare beneficiaries in the United States, comprised of 42.1million elderly (age 65+) and 8.5million disabled beneficiaries. In order to qualify for Medicare, US citizens need to qualify in at least one of three eligibility requirements:
As mentioned earlier, Medicare represents 21% of national healthcare spending, making it the largest contributor. Medicare spends $554.3billion for 50.7million Medicare beneficiaries and accounts for 15% of the national budget.9,13 During years in which there is a surplus in funds- where taxes collected for Medicare exceed monies paid out the excess funds are reinvested in the Medicare trust (known as the Medicare HI Trust). The trust has been running a deficit since 2008 and at this rate, will be depleted by 2024.13 Because of the recent pressures to control Medicare spending, the ACA has created the Independent Payment Advisory Board (IPAB) which will be allowed to submit legislative proposals to reduce the cost of Medicare if the program’s per-capita spending grows faster than per-capita GDP.14
Medicare vision/mission: According to the CMS website, the CMS’ mission statement, vision and strategic action plans are as follows:
Mission: “To ensure effective, up-to-date health care coverage and to promote quality care for beneficiaries”
Vision: “To achieve a transformed and modernized health care system.
CMS will accomplish our mission by continuing to transform and modernize America’s health care system”
CMS’ Strategic Action Plan Objectives: “Skilled, Committed and Highly-Motivated Workforce, Accurate and Predictable Payments High-Value Health Care, Confident, Informed Consumers, Collaborative Partnerships”.
Policy brief
The IIPCP policy will prevent impending Medicare graduate medical education (GME) funding cuts by redistributing Medicare indirect medical expense (IME) funding to address the growing need for primary care providers. AAMC teaching hospitals will continue to receive direct medical expense (DME) funding with no changes to the current model; however, Medicare will utilize the previous IME annual budget to increase the number of primary care residencies by 15,000. IME funding will now be known as IIPCP funding. This funding, previously used to subsidize indirect medical costs incurred by teaching hospitals, will be distributed to teaching hospitals as outlined below.
Medicare support of GME
Distribution of IIPCP funding
For example: if a teaching hospital has received $800,000 in annual IME funding, they will be required to increase their PCP residencies by two positions. $800,000 IME dollars/ $400,000 cost per new resident=increase in two positions.
For example: if a teaching hospital has received 750,000 in IME funding they will be required to increase their PCP residencies by 1.875 positions. Since it is impossible to have a fraction of a person, this institution would be required to increase their PCP residencies by two positions and then would receive an extra 50,000 in IIPCP funding subsidize the difference.
Opting-out
IIPCP Implementation
New structure: The success of the IIPCP policy will rely heavily on careful implementation and utilization of the correct resources. Many of the AAMC teaching hospitals are already making the necessary investments that are outlined in this section; however, it is imperative that all AAMC teaching hospitals make certain capital and technological investments that will promote the success of this policy.
Investment level: Initially, the AAMC teaching hospitals will have to make large investments including up to date EMR software (approximately $200million per hospital), new resident salaries ($1.02million per hospital per year), new supplies, new PCP faculty members and building space. Because of these costly investments, AAMC hospitals will need to make the appropriate cuts in expenditure to cover the IME subsidy that are used to receiving. This will be done through extensive analysis and underwriting of each department. Certain specialty residency programs may need consolidations and require better control over other capital expenditures and operational costs. As the new residencies help create more efficiently-executed operations, the hospitals will begin to improve their per patients costs ultimately leading to cost savings over the course of ten years.
Capital investment: With implementation of the IIPCP policy, the $6billion that teaching hospitals receive in IME funding from Medicare will no longer be used to subsidize the higher patient’s costs. Under the IIPCP, hospitals will receive approximately $15million on average; this funding will be used to pay for new PCP faculty salaries, new PCP resident salaries and training equipment for these programs. In a study conducted at the University of Washington, the average added cost to a teaching hospital per PCP resident is approximately $27,20015 thus, with an expansion of 15,000 new PCP residents; it will cost AAMC teaching hospitals an aggregate $405,000,000 each year. Because the number of residency position will be split among hospitals, this would equal an average of 37.5 new residents per teaching hospital for an average of $1,020,000 per hospital per year. This average varies significantly among the residency programs because there are not standardized benchmarks to compare costs. Health IT is another capital expenditure required to support new physicians and can cost hospitals $15,000-$70,000 per provider. This means that with an additional 37.5 new residents per year, this will cost each hospital a projected $560,000-$2,625,000 per year in health IT.16 The remainder of the funding will help these hospitals invest in millions of dollars worth of building space, facilities, technology and medical equipment to effectively run the new residency programs. Some hospitals are also creating more outpatient clinical training sites, which will be a large capital expenditure but will eventually lead to lower per patient costs.
New health technology: Due to the increase in PCP residents and faculty members within the AAMC teaching hospitals seeing patients, efficacy and efficiency will rely heavily on good communications between PCPs and their specialist counterparts. Many teaching hospitals are investing in sophisticated health information technology such as Electronic Medical Records (EMR) as a means to better communicate and coordinate care. Along with the implementation of new health IT, significant training and integration among specialties will be critical to producing effective communication.
EMR: For a large AAMC teaching hospital, the investment in the latest EMR system can cost upwards of $200million.17 If including the added costs of linking and integrating systems and training, EMR implementation costs can be raised to approximately $1billion. Although large hospitals are making large investments the potential of an increase efficiency and lower healthcare costs overtime are worth the risks involved. Many teaching hospitals will have to make these investments in health information technology regardless of an increase in residency positions and the increase will likely exacerbate the need for technologically sophisticated communication tools among departments. The adoption of an integrated EMR network has several key benefits. Teaching hospitals can reduce the patient costs by minimizing complication, limiting duplicate tests and improving patient outcomes. Indirect stakeholders, such as patients who receive better outcomes, receive many non-financial benefits. Also, physicians, nurses and hospital employees who can better communicate without having to scan and fax records to make clinical decisions. As standardization of EMR continues to improve, many more benefits will arise over the new few years and EMR adoption will steadily increase.
Financial risk: If the hospitals do not actuate an increase in net profits from the benefits of seeing more patients at a lower cost, it could result in one of two scenarios: first, they would run the risk inadequately training the new influx of residents (this could indirectly inflate per patient costs due to poor medical decisions leading to patient complication); the second risk would be the risk of having net losses over several years resulting in bank ruptcy. Many teaching hospitals do not receive adequate funding to account for the added costs of residency training programs. Because of this, they are utilizing clinical revenues to help pay for these programs unmet financial needs. With a 15,000-position increase in PCP residencies, these teaching hospitals run the risk of overusing their clinical profits. Increased controls over capital and operational disbursements will be necessary to mitigate these risks.
Mitigation of risk: In an effort to make up for the lack of subsidization for higher patient costs, the hospitals will have to find ways to reduce expenditures and increase profits. One way to do this is to reduce direct costs associated with the residency programs themselves. Teaching hospitals should look at reducing the number of specialty faculty members and increasing the resident to faculty member ratio as a way to cut salary costs. Another way to increase profits is by decreasing per patient costs and increasing clinical revenues. Because of the increase in PCP providers within the institutions, teaching hospitals may be able to increase the number of patients they treat while reducing the costs incurred per patient. They will need to better utilize inpatient capacity and re-design the front-end services (registration, underwriting, cashiering etc.) as a means to increase professional fees and improve collection rates.
Financial impact of IIPCP over 10years: Over the next ten years, the potential impact of the IIPCP on profits and losses at teaching hospitals will be an initial loss and a gradual transition to increased profitability after approximately five years. At ten years, profit levels will most likely reach their maximums in terms of percentage in net growth. The first few years will most likely result in losses for the hospitals due to the utilization of clinical revenues to help cover training costs for their new resident training programs. As these hospitals become more efficient at training the new PCP residents, they will most likely see these losses level off and begin to see a profit when the new efficiency of having a greater number of PCP residents seeing patients will increase productivity of their clinical workload. Also, due to lower required salaries for PCP faculty versus specialist faculty members, hospitals will realize a cost savings in faculty pay. Because PCP faculty members can teach a greater number of residents at once, due to similar content, hospitals will be able to hire fewer faculty members. In contrast, having a vast array of specialty residencies requires faculty members belonging to each respective specialty. This initiative would help consolidate the diversity of specialty training programs. The final consideration that the AAMC faces in implementing the IIPCP is consistency. If the IIPCP is implemented, consistency will be difficult to measure between organizations in the efficacy of their resident training programs. It will be detrimental to determine a level of standardization in training programs for the AAMC member teaching hospitals to continue to receive funding from Medicare on an annual basis. This standardization will also be necessary to measure the success of this policy and to continue to maintain federal support. The AAMC teaching hospitals will need to utilize this measurement on PCP output to show a ROI to the US government in closing physician gap shortages.
AAMC’s interest in the IIPCP
The IIPCP policy initiative would allow the 400 AAMC teaching hospitals to continue to receive the annual $6billion in federal subsidy that Medicare has allocated for IME funding. The IME funding is at a high risk of being eliminated by cuts to federal spending and the funding could be used to effectively increase their number of PCP residency positions by 15,000. Teaching hospitals rely heavily on the IME funding which accounts for more than three times what they receive in DME funding ($9.5billion versus $3billion respectively). Cuts in IME funding would impose financial strains on these teaching hospitals. These strains could initiate budget cuts resulting in fewer residency slots rather than incentivizing them to increase the number of positions to meet the demand of the projected influx of more patients. Although members of the AAMC would prefer that no budget cuts be made to federal support of GME, this policy would prevent the elimination of funding that is impending if no compromise is made. By redistributing funding of indirect medical expenses to funding of new PCP residencies, the policy would incentivize teaching hospitals to analyze their residency programs and run more efficient programs.
In addition to maintaining federal aid, AAMC teaching hospitals would also benefit by being able to continue their mission of leading the academic medical community while improving the health of all by addressing the need for more PCPs. Incentivizing more PCPs is critical to keep up with the demand of the millions of new Americans seeking treatment. If not changed, the trend of the number of PCPs versus patient demand will continue to be disjointed (Figure 4). Hospital executives are under the most pressure finding a solution to the potential of losing IME funding. They are the most in tune with the financial analytics and are directly responsible for managing revenues, profits and losses. The hospital executives’ main interests are to continue to receive the IME portion of Medicare funding because if this portion of support ceases, they will have to continue to reach deeper into clinical revenues to help fund residency training programs. These executives rely heavily on clinical revenues to help pay for many other aspects of the hospital operations and many hospitals cannot afford to redirect these funds.
Pros/cons for the consumer
Pros: As the government begins the early stages of the implementation of the ACA, many consumers are confused regarding the potential changes to healthcare. Although the ACA promises a solution to access, there is still no solution to the growing need for more primary physicians. The ACA has, in fact, exacerbated the need for more PCPs. From the consumer perspective, having health insurance does not necessarily mean having access to care. Patients are already experiencing a difficult time scheduling appointments with PCPs, with in an appropriate time frame and this has been a cause for over-utilization of hospital emergency departments; this only adds to the amount of wasteful spending on healthcare and ultimately increases costs to the consumer. The increase in number of patients seeking health care will only further make scheduling more difficult unless this physician shortage is addressed.
The IIPCP will allow AAMC hospitals to phase-in new PCPs in a gradual manner over the next ten years as more patients sign up for health coverage. As mentioned earlier, the Federal Health Resources and Services Administration projects a deficit of 55,000-150,000 physicians by the year 2020.10 The IIPCP will generate exactly 150,000 new primary physicians over the next 10years. In regards to the three consumer expectations of quality, cost and access, the IIPCP provides solutions to all three sides of the triangle. It increases quality by providing more efficient and effective communication between physicians which leads to better patient outcomes. The cost of healthcare will be reduced due to more PCPs available and a reduced need to seek specialty care; emergency room utilization costs will decrease due to better access. Finally, the IIPCP, in conjunction with the ACA will improve access due to the greater number of PCPs.
Cons: Consumers may not react well to seeing a primary care physician versus a specialist in certain situations, especially when they are accustomed to receiving certain care from specialists. They may not have trust in their primary care physicians because they do not view them as experts in medicine; the disparity in PCP versus specialist pay and power in the US is partially to blame for this frame of thought. Ultimately, this could result in certain patient populations seeking treatment at non-teaching institutions.
Pros/cons for the physician
Pros: Because of the ACA implementation and the increasing need for more primary care physicians, both specialists and PCPs will benefit from the increase in number of primary care physicians created by the IIPCP. Since many health plans are requiring patients to seek care from a primary care physician before visiting a specialist, many specialists will rely heavily on referrals from their primary care counterparts; thus, specialists are also affected by long scheduling delays from a shortage of PCPs. Patients may not be able to seek immediate care from specialists as readily as in the past; thus, if they are waiting to get an appointment with a PCP, the specialists are also indirectly waiting. When patients have direct access to specialty care, many patients do not properly diagnose themselves and end up seeking care with the wrong specialty. The increase in PCPs will lessen the burden of specialists having to perform PCP functions and then retroactively sending the patient to the appropriate specialists.
Primary care physicians, especially residents desiring to practice primary care, will benefit from the increase demand for AAMC hospital to fulfill their PCP residency requirements. Medical students focusing on PCP specialties are also more likely to “match” to a specific training program and will be less fearful on becoming a “non-matched” medical student in who has to reapply again at a later time. Not only will PCP residents be in high demand, but practicing PCPs and PCP faculty will also be in high demand in order to teach and train these new residents. As the increase in demand for PCP residents, faculty and staff rises, the PCPs will also realize a shift in power. The power will shift from the select high revenue-earning specialists to the PCPs. Because PCPs are not niched in one particular specialty, this will potentially result in a more organized and efficient coordination of care.
Cons: There are many ways AAMC teaching hospitals can diligently try to control risks to physician staff; however some risk is unavoidable. One risk is the reaction to changes from faculty, current residents, new residents, hospital staff and patients. There will have to be shifts in power, salary and space and along with these shifts come disgruntled staff.
In order to achieve large-scale success in implementing the IIPCP initiative, there needs to be a fundamental power shift-from the hospital executives and specialty physicians/faculty to the primary care physicians/faculty. There also needs to be a shift in power from the primary care physicians and faculty to members of their team.18 These shifts in power are necessary to have the most effective and efficient workforce to meet the demands of patient care and to effectively train the new influx of patients and PCP medical residents. Nobody likes giving up power voluntarily and it is certain that this will come with some conflict. Some of the consequences of this type of conflict could include the resignation of key faculty members; certain specialists and faculty members boycotting teaching hospitals; and hospitals losing their trauma rating, (i.e. Level 1 Trauma) as a result of bureaucratic conflict between departments resulting in a boycott. The IIPCP would affect physician faculty in several ways. Because there would be an increase in PCP residency positions, there would be an increase in demand for new faculty members; however, the increase would only be for PCP faculty members. The non-PCP (specialty) faculty members may be opposed to the IIPCP because they would most likely have to share their resources with the new PCP faculty members and PCP residents. Some of these resources may include salary, office space, resident education budgets and building space.
Finally, medical residents could find several disadvantages to the IIPCP. The residents in specialty services may be opposed to this initiative for similar reason to faculty members concentrating in specialty services. They would have to share resources such as pay, space and may even have to share many of the types of patients they typically treat. There would also be a decrease in demand for the these residency training programs as these teaching hospitals become dis incentivized to house specialty residency training positions. Residents and medical students focusing on PCP training programs will be more likely to support this initiative since the demand for these positions are likely to rise due to hospitals needing to fulfill their quotas in the number of PCP residency positions for funding eligibility.
Pros/cons for medicare
Pros: The creation and implementation of the ACA is an attempt to increase patient access while reducing cost. Drastic cuts in Medicare GME support are a short-term solution that could be financially devastating in the long run. If Medicare eliminates IME spending without addressing the PCP physician shortage, access will be an even larger problem. In regards to the ACA, the threat is not access in terms of health coverage; it is access in terms of PCP availability. In order to increase the output of PCPs to support the ACA, teaching hospitals will need to be given a reasonable means of training these PCPs. AAMC teaching hospitals are already utilizing clinical revenues to supplement the costs of their residency programs and will not be able to support these programs if the $6billion annual IME dollars are cut. The IIPCP will be a measure that the Federal government can use to prevent are more catastrophic and ultimately even more costly outcome if these funds are eliminated. The IIPCP will also allow the Federal government to redistribute the number of PCPs to areas that are significantly lacking PCP care. As outlined in the proposal of changes, teaching hospitals have the option to “opt-out” of the IIPCP program. It will then be at Medicare’s discretion as to which participating hospitals receive the extra funding to further increase their PCP residency positions.
Cons: As part of a national attempt by the Obama administration to lower the national debt by $3.2trillion dollars over the next ten years, approximately 9% of the proposed budget cuts come from Medicare and Medicaid programs.19 Because the IIPCP proposes that current IME financial support remain the same in dollar amount, it does not help lower the national debt directly. In order for the IIPCP policy to take effect, it will be necessary to overcome this political obstacle.
Even if the IIPCP policy is passed, there will still be several financial and institutional barriers to address. Many of the teaching hospitals are already financially strained from “rising operational costs, lower insurance reimbursements and in some states, reduced Medicaid funding”.19 With Medicare IME contributions remaining constant, the IIPCP will require teaching hospitals to increase the number of primary care residencies while many institutions are already using some of their clinical revenues to help fund their residency training programs. Because clinical revenues at hospitals are also declining, these hospitals will have to find other ways to make the necessary institutional budget cuts to manage the new influx of training positions. They will have to hire more faculty members, pay residents’ salaries and also invest in more capital to be able to take on this commitment.
The proposal of the IIPCP policy presents a fair compromise to the financial risk of losing Medicare IME support. The AAMC understands that without an added benefit to the US healthcare system, such as the proposed increase in 15,000 PCP residency slots, it would be much more difficult to convince key legislators to be in favor of continuing to support IME funding. This policy will help decrease the output of the number of specialists trained by teaching hospitals. Decreasing the number of residency slots for specialists will be attractive to the Obama administration when lobbying for this policy change because it will help encourage medical students to seek their medical doctorate in primary care using supply-side rationing to control the output. Although the AAMC teaching hospital would most likely incur financial losses in the early stage of implementation, it is less risky than the alternative of inertia, which ultimately could result in a drastic loss in federal GME support.
Key benefits: The benefits outlined in this proposal stakeholder support will play an integral role in the adoption and continuation of the IIPCP policy.
AAMC teaching hospitals will continue receiving the $6billion annual dollars for GME support that they have relied heavily on in past years. These hospitals, although initially having to invest in capital would eventually be able to reduce per patient costs, increase profit margins and ultimately increase revenues by seeing more patients. The per patient cost reductions would be an indirect result of increasing the number of patients treated because they will have more PCPs involved in the less complicated patients.
From the physician perspective, communications between PCPs and specialists would be improved with integration of better EMR technology resulting in better efficiency and efficacy between departments. There will be increasing demand for new PCP faculty and residency positions in order to effectively train the new PCP residents and there will be a shift in power from specialists to the PCPs within hospital networks.
The American public seeking healthcare will see benefits in terms of better care and better outcomes. This will be achieved through fewer duplicate tests, shorter wait times and a greater number of PCPs available to treat them. This will address the consumer’s concern in healthcare quality stemming from the ACA’s intention to increase access and control costs. Addressing quality will rebalance the changes to the iron triangle of healthcare. One of the most important benefits of the adoption of the IIPCP policy is that the government will have a solution to the growing need for more PCPs as the ACA is implemented. As 15,000 new PCP residencies generate 150,000 new primary care physicians over the next decade, Medicare will be out of the “hot seat” in addressing the growing shortage in PCP care. Because of this increase, the HHS will be able to tie the $6billion of GME support to a tangible result rather than using the funding to support indirect medical expenses.20
In summary, the IIPCP will provide 15,000 new PCP residencies each year resulting in an aggregate 150,000 new PCP over the next decade. This policy would not only address the growing shortage in PCPs exacerbated by the ACA, but also help redistribute PCPs to geographic areas that lack the most PCP care. Also, the IIPCP will allow AAMC hospitals to utilize supply-side rationing to decrease the number of specialty residencies ultimately address the disjointed ratio of PCP to specialty physicians. As healthcare in the US trends to a more centralized system of patient care, the IIPCP will allow PCPs to regain control within these networks. Because PCPs are better qualified to coordinate care than their specialist counterparts, this will lead to more effective and efficient treatment and better patient outcomes. Finally, Medicare will not have to change the amount that they are currently spending on GME support, but they have a more tangible, measurable return on their investment.
In conclusion, the IIPCP policy would provide a compromise between stakeholders of the AAMC teaching hospitals and the key legislators within the Obama administration. Even though all parties would have to contribute large amounts of investment and incur risk, it is a way for both AAMC stakeholders and government leaders to work together in achieving better healthcare while minimizing unnecessary spending. The AAMC should be in favor of supporting this initiative as a way to proactively address growing concerns of the US healthcare system and impending cuts to GME support. Although this policy is uncharted territory, it will provide a means for AAMC teaching hospitals to continue to train our nation’s doctors today, which will in turn provide the healthcare of tomorrow.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.