MOJ
eISSN: 2374-6939


Research Article Volume 6 Issue 2
University Hospital Wales, UK
Correspondence: Alun Yewlett, University Hospital Wales, 383 Western Avenue, Cardiff, CF5 2BD, UK, Tel 7815118525
Received: October 19, 2016 | Published: October 19, 2016
Citation: Yewlett AD, King AC, Brooks FM, Evans RO, Williams RW (2016) What is the Single Most Important Technical Aspect When Fixing a Proximal Humeral Fracture with A PHILOS Plate? MOJ Orthop Rheumatol 6(2): 00213. DOI: 10.15406/mojor.2016.06.00213
Introduction: This study aimed to identify technical factors contributing to hardware complications with PHILOS plates.
Methods: A five year retrospective radiological review of all PHILOS platings at our institution was performed. Pathological fractures and revision cases were excluded. (79 patients, 73 females, mean age 88 and range 15-108). AP (Antero-posterior) radiographs were used to assess infero-medial support (presence or absence of calcar screws), adequacy of reduction by measuring the neck-shaft angle, and loss of reduction. The first postoperative radiograph was compared with a follow up radiograph from more than 12 months after the index surgery and cases that required revision were identified. Six patients underwent further surgery for either screw perforation into the joint or plate failure. Cases were then divided into two groups, a revision group (R) and an unrevised group (U), and statistical analysis using Wilcoxon’s rank test for non-parametric data was performed looking at the differences between mean neck shaft angle, adequacy of reduction and loss of reduction in both groups.
Results: A clinically and statistically significant difference was found in the mean neck shaft angle between the unrevised and the revised groups. The mean neck shaft angle was 129° in patients who did NOT undergo any further procedures (N = 73). The mean neck shaft angle was 110° in patients who DID undergo revision (N = 10) P <0.03.
Conclusion: Restoration of an adequate neck-shaft angle was the most important determinant of successful PHILOS plate fixation. If this was not achieved, screw perforation or plate failure occurred.
Keywords, Proximal humerus, ORIF, Plating, Technique, Complications, Review
Proximal humeral fractures account for 5% of fractures and are the third commonest fracture in elderly patients after femoral neck and distal radial fractures.1,2 The majority can be treated conservatively.3 but there are certain fracture personalities that are believed to benefit from surgery.4 (Table 1).
|
1 |
2 part GT/LT #s 3 or 4 part #s where GT displaced by >1cm |
|
2 |
#s with a displaced fragment of the articular surface of the humeral head attached to a displaced tuberosity fragment |
|
3 |
Unstable 2 part surgical neck #s in which there is disengagement of the shaft from the humeral head, due to displacement or extensive metaphyseal comminution. |
|
4 |
2, 3 or 4 part #s in which there is varus or valgus deformity of the humeral head to the shaft by >300 from the normal head shaft inclination of 1300. |
|
5 |
3 or 4 part anterior #-dislocations caused by the propagation of posterior humeral head # (‘Hill-Sachs lesion’) and with retained soft-tissue attachments to the humeral head at surgery (‘Type 1’ anterior #-dislocation). |
|
6 |
3 or 4 part posterior #-dislocations caused by propagation of a # of the anterior humeral head (‘reverse Hill-Sachs’) and with retained soft-tissue attachments to the humeral head at surgery. |
Table 1 Relative indications for fracture fixation in proximal humeral fractures.
Stable fixation of proximal humeral fractures is challenging. Historically surgeons faced multifactorial problems including osteoporotic bone, angular instability and lack of availability of low-profile implants to avoid impingement. The PHILOS (Proximal Humerus Locked Plating System) has locking screws which provide angular stability and better hold in osteoporotic bone. It is also low profile, which minimises sub-acromial impingement. It is suitable for two-part, three-part and certain four-part fractures in the young and elderly.4
Although studies using PHILOS plates report good results overall.4,5 there are well recognised complications including avascular necrosis (AVN), screw cut-out, non-union and plate or shaft screw failure.5 Mal-reduction and loss of fixation are important reasons for poor outcomes after surgery. Studies have shown that loss of fixation occurs primarily in the presence of varus malreduction.6 and it has been shown that the placement of superiorly directed oblique locked screws (calcar screws) can prevent loss of reduction by providing inferomedial support.7,8 These concepts are supported by a biomechanical study by Lescheid.9 who demonstrated that anatomical reduction with medial cortical contact is the stiffest construct when forces are applied. They found that removal of cortical support had a drastic effect on axial, torsional and shear stiffness at 10° and 20° of varus angulation and failure occurred secondary to plate bending as the humeral head was pushed down medially and distally.
Failed surgical fixation due to hardware failure is a devastating complication for both the patient and the surgeon. If revision surgery is required, it may entail significant morbidity. If a technical cause for hardware complications can be identified then surgeons should be able to minimise these in the future. We therefore reviewed all PHILOS plate fixations at our institution to attempt to determine what surgical factors predicted hardware failure, particularly the role of calcar screws in providing inferomedial support.
All patients who underwent ORIF (Open Reduction and Internal Fixation) of a proximal humerus fracture using a PHILOS plate between January 2005 and November 2010 in our institution were identified retrospectively by searching our electronic theatre log. Patients who underwent the procedure for a pathological fracture or revision surgery were excluded. All operations were performed by or directly supervised by one of the two senior authors who are fellowship trained consultant orthopaedic shoulder surgeons. The surgical technique was the same in all cases with the patient in the beach chair position and a standard deltopectoral approach utilised and image intensification used as required.
Pre-operative radiographs were evaluated and fractures were classified according to Neer’s classification.10,11 The initial postoperative AP (anteroposterior) and most current radiographs of at least 12 months following index surgery were used to assess inferomedial support, adequacy of anatomical reduction and loss of reduction. Inferomedial support was considered present if one or more calcar screws were placed i.e. running tangentially to the medial curvature of the humeral neck (Figure 1). Adequacy of anatomical reduction was assessed by measuring the neck-shaft angle (Figure 2). Loss of reduction was assessed by measuring the height between the humeral head and the proximal end of the plate (Figure 1).
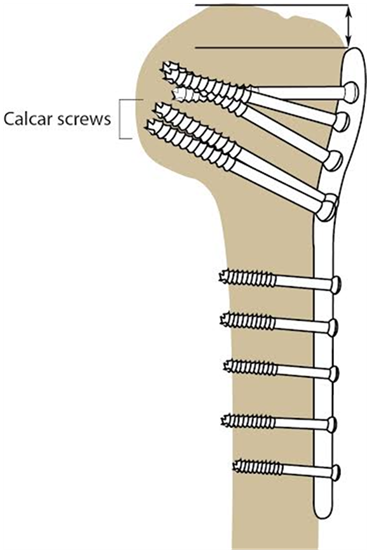
Figure 1 Calcar screws in the inferomedial humeral head and height between the humeral head and the proximal end of the plate used to assess for loss of reduction.
Complications (AVN, screw cut-out, non-union and plate or shaft screw failure) and further procedures were also evaluated on postoperative radiographs. AVN was defined radiographically as flattening or irregularity of the humeral head (Figure 3) and screw cut-out was defined as protruded screws into the glenohumeral joint (Figure 4). Implant failures were either broken plates or screws or pulled out screws (Figure 5). Cases were then divided into two groups, a revision group (R) and an unrevised group (U), and statistical analysis using Mann-Whitney U test for non-parametric data was performed looking at the differences between mean neck shaft angle, adequacy of reduction and loss of reduction in both groups.
Further subgroup analysis was performed looking at the number of parts in the fractures according to Neer’s classification. The mean change in the neck shaft angle from the preoperative images compared with the post-operative follow up films was reviewed as were the number of calcar screws used if any.
Statistical analysis was performed using IBM SPSS v20.0 (IBM, USA). The data was not all normally distributed, so a Mann-Whitney U test was used to look for differences between the means of neck shaft angle, plate height and between the revised and unrevised groups. Fisher’s exact test was used to test the relationship between the use of calcar screws and failure of fixation. Linear regression was used to examine the relationship between change in neck shaft angle, initial plate height and age. A similar analysis was performed for the relationship between change in height of the plate, initial neck shaft angle and age. A p value of <0.05 was considered statistically significant.
ORIF using a PHILOS plate was performed in 105 patients who were eligible for inclusion. 25 patients were excluded, including one patient who died within three months of surgery and 24 without available post-operative radiographs because they were archived or moved out of our area. Radiological follow-up was possible in 79 patients, (mean age, 88 years, range 23-108) at a maximum of 4 years. There were 50 two part fractures, 25 three part fractures and 4 four part fractures. Fractures were treated after a median of 8 days.
Sixty-six patients had calcar screws in situ (20 with one calcar screw, 38 with two calcar screws). The mean loss of reduction was 2mm (3mm for no calcar screws, 1mm for 1 calcar screw and 3mm for 2 calcar screws) after a mean of 281 days.
Ten patients (median age 67 years, range 45-76) underwent further surgery for post-operative complications. One for AVN, two for screw cut out, one for plate failure, two for shaft screw failure and three for non-union. These were noted on radiographs after a mean follow up of 204 days.
The mean neck-shaft angle was 129o in patients who did not undergo a further procedure (no calcar screw 129°, 1 calcar screw 132°, 2 calcar screws 134°) compared with 110° in patients who underwent revision (no calcar screw 117°, 1 calcar screw 120° and 2 calcar screws 107°).
Statistical analysis showed a statistically significant difference (p=.004) between the initial neck shaft angle in the revision versus the unrevised group, but plate height and age were both non-significant (p=0.64 and p=0.53 respectively). There were no other statistically significant differences found, except that the use of calcar screws was significantly related to failure (p=0.048).
The change in neck-shaft angle was predictable the by initial neck shaft angle (p<0.01), but not age (p=0.68) or height of the plate (p=0.41). Similarly the change in height of the plate was predictable by the initial neck-shaft angle (p=0.013) and initial height of the plate (p<0.01) but not by the age of the patient (p=0.75).
The subgroup analysis of mean initial humeral neck shaft angle by Neer classification of parts is tabulated below along with a breakdown of the meaninitial neck shaft angle versus the number of calcar screws used (Table 2 & 3). These are graphically shown in figures 6 and 7. We also looked at the mean change in the neck shaft angle for both the types of fractures by Neer group and also the specific changes based on the number of calcar screws used. These changes along with their standard deviations are shown in Figure 6 & 7.
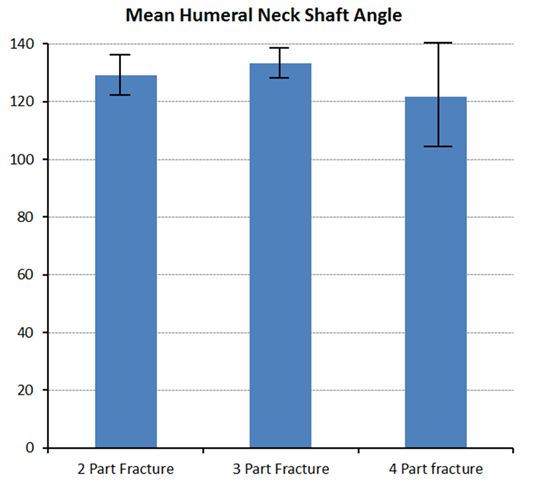
Figure 6 Bar Chart showing the mean humeral neck shaft angle with standard deviations for the three different fracture types.
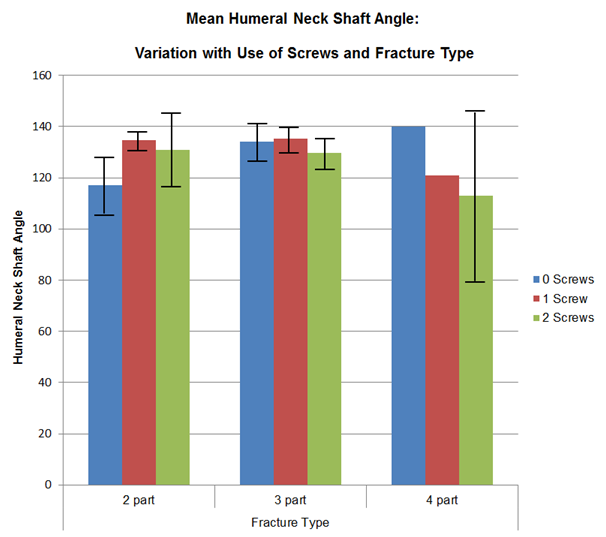
Figure 7 Bar chart showing means humeral neck shaft angle and standard deviations by fracture type and number of calcar screws used for fixation.
|
Fracture Parts |
2 |
3 |
4 |
|
Number |
50 |
25 |
4 |
|
Average |
129 |
133.3 |
121.75 |
|
SD |
16.24 |
13.22 |
38.89 |
Table 2 Mean initial humeral neck shaft angle by fracture type.
|
Fracture Type |
2 Part |
3 Part |
4 Part |
||||||
|
Screws |
0 |
1 |
2 |
0 |
1 |
2 |
0 |
1 |
2 |
|
Patients |
5 |
17 |
28 |
6 |
7 |
12 |
1 |
1 |
2 |
|
Mean Angle Change |
-3.6 |
-3.8 |
-1.3 |
-5.2 |
-2.6 |
-7.4 |
-12 |
-3 |
-2 |
|
SD |
9.59 |
14.63 |
9.15 |
4.36 |
8.92 |
8.32 |
n/a |
n/a |
16.97 |
Table 3 Sub-group analysis by fracture type.
Previous studies have shown that the presence of medial support has a significant effect on the magnitude of subsequent reduction loss, independent of age and fracture type. In this case series, restoration of an adequate neck-shaft angle was the most important determinant in fixation. If this was not achieved, despite adequate infero-medial support, screw perforation or plate failure occurred.
When performing ORIF of proximal humeral fractures with PHILOS plating the surgeon should consider complications and how to prevent them. Our overall revision rate was 12%, which was slightly higher than that reported in other studies, but because of the small number of cases it is difficult to draw conclusions about the rate of individual complications. When non-unions and AVN were excluded our revision rate for hardware complications was 6%. However, when we looked at our complication rate after the first 12 months it dropped to 3%, which is lower than all other reported studies to the best of our knowledge. We ascribe this to the surgical learning curve, both in terms of technical execution and also patient selection over the time course of this study. We recognise that there are limitations to our study, particularly as it only involved radiological assessment of fixation. For example, AVN was assumed to be iatrogenic but patient factors could have predisposed to a negative outcome. However, information in the literature about the influence of patient’s comorbidities, smoking and steroid therapy and the results after ORIF of proximal humeral fractures is lacking.
Looking at the subgroups in more detail, we found that apart from a single outlier in the 4 part fractures that lost 12 ° from its initial neck shaft angle, the maximal mean angle change across all fractures occurred in our three part fractures that were fixed with 2 calcar screws. In this group of 12 patients the varus angulation increased by 7 ° even though two calcar screws were used. In the other two groups namely the 2 part and 4 part fractures when two calcar screws were used on average a 2° or less change in neck shaft angulation occurred. We noticed that there was always some loss of neck shaft angle over time, although we believe that a change of less than 1-2 degrees may be explained by simple measurement variability and was not in our view clinically significant.
How do we account for the increased loss in reduction with two calcar screws in the three part fracture group? We believe that those fractures that were the most technically difficult to reduce, such as those with calcar comminution or significant displacement were more likely to end up having a more varus reduction accepted than for simpler fractures. When faced with such a situation the operating surgeon may have felt that two calcar screws would provide the best support to prevent further displacement and to maintain the best achievable reduction based on our original understanding of their role. However, what our series has shown is that an excellent reduction is critical and if this cannot be achieved then calcar screws will not salvage the situation. We would therefore advocate surgeons involved in treating these difficult factures take great care to achieve an anatomical reduction. What our data has shown is that achieving a mean neck shaft angle of 110° or less after ORIF will predict failure. What is not yet known is the minimum neck shaft angle needed to prevent this, but from our series achieving a reduction of 129° or greater appears to be satisfactory.
This study shows that the restoration of an adequate neck-shaft angle is the most important determinant of successful PHILOS plate fixation. If this was not achieved, despite adequate infero-medial support, screw perforation or plate failure occurred. We recommend that a neck shaft angle of greater than 129o be achieved to avoid failure of fixation for these patients.
The authors would like to thank Jan Sharp for her help in preparing the figures and also Dr David Newman for help with preparing the graphs.
None.

©2016 Yewlett, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.