MOJ
eISSN: 2374-6939


Case Report Volume 6 Issue 3
Department of Orthopaedics, Centro Hospitalar do Algarve, Portugal
Correspondence: Tania Pinto Freitas, Faro Hospital, R Leao Penedo, 8000-386 Faro, Portugal
Received: November 08, 2016 | Published: November 8, 2016
Citation: Freitas T, Couto A, Lopes M, Rosas J, Sacramento T, et al. (2016) Tuberculous Tenosynovitis of the Wrist and Hand- A Case report. MOJ Orthop Rheumatol 6(3): 00222. DOI: 10.15406/mojor.2016.06.00222
Tuberculous infection of the hand is a rare form of extra pulmonary tuberculosis that can cause serious joint and tendon damage.
We report the case of a 79-year-old female patient who presented with swelling over her left wrist for over 2 years and insidious flexor weakness of the fingers without any history of trauma. As comorbidities, she had hypothyroidism and a history of previous surgery of a giant cell tumour located volarly on her left wrist, which demanded tendon sheath excision. Ultrasonography showed a synovial cyst in the wrist. Plain X -rays revealed no abnormal findings in bone, joint, and soft tissue. Magnetic Resonance Imaging (MRI) was suggestive of flexor tendon sheath tenosynovitis, with a fluid collection in the tendon sheaths of the first to the fourth fingers and in the flexor compartment along the ulnar and radial sides of the wrist. Chest radiograph of this patient showed a small nodule on the right lung. An excisional biopsy was planned and intraoperatively, a yellow dense fluid was seen inside it. Histopathological examination showed fibrosis, epithelioid histiocytes, giant cells in the stroma as well as mononuclear inflammatory cell infiltration. Fluid’s microscopic analysis was positive for Mycobacterium tuberculosis, confirming the diagnosis of tuberculous tenosynovitis of the wrist and hand. We determined that she required treatment consisting of appropriate antituberculosis agents. The early suspicion and diagnosis of this extrapulmonary disease facilitates anti-tuberculous chemotherapy and help avoid wrong diagnosis and incorrect therapies.
Keywords: Wrist, Tuberculous, Tenosynovitis
Tenosynovitis, one of the common reasons of wrist pain, may has various aetiologies. One of the infectious causes of the wrist tenosynovitis is M. tuberculosis. Although antituberculosis drugs reduced the incidence of M. Tuberculosis infections, its prevalence is again increasing due to immune deficiency syndromes.1 It is mainly known as a pulmonary disease. Extrapulmonary tuberculosis involvement of the musculoskeletal system is uncommon, accounting for only 10% of tuberculosis cases. Involvement of the hand and wrist at presentation is extremely rare, and the diagnosis is often missed.2-4
To heighten awareness of this infection so that delays in diagnosis and treatment can be avoided, we present a case of tuberculous tenosynovitis.
A 79 years -old woman was admitted to the orthopedic department with symptoms of left volar wrist pain, swelling, flexor tendon weakness, which had started two years before. The swelling was soft in consistency, mobile, tender but without warmth or redness. She also complained about paraesthesia on the first to third fingers.
As comorbidities she had hypothyroidism and a history of a previous surgery performed on her left wrist, volarly, that consisted on the excision of a giant cell tumor of tendon sheath. She refers recurrence of the lump a month later. Laboratory tests were within normal range: C-reactive protein (CRP): 7 mg/L, erythrocyte sedimentation rate (ESR): 10 mm/h, and white blood cells (WBC): 6200 × 103 mm3.
Simple X-rays revealed no abnormal findings in bone, joint, and soft tissue. Magnetic resonance imaging (MRI) (Figure 1) was suggestive of flexor tendon sheath tenosynovitis. It revealed a fluid collection in the tendons sheath of the first to fourth fingers and in the flexor compartment along the ulnar and radial side of the wrist.
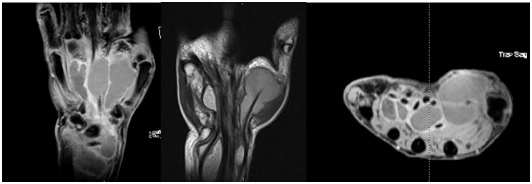
Figure 1 fluid collection in the tendons sheath of the first to fourth fingers and in the flexor compartment of the wrist.
A chest radiograph revealed a pulmonary calcified nodule, suspicious of an old tuberculous infection; however, no significant differences were found in patterns and sizes of these lesions when compared to the previous films. There was no past or family history of tuberculosis. She did not have any complaints of respiratory symptoms, including cough, sputum, or chest discomfort.
A follow up serologic test was negative for human immunodeficiency virus (HIV) antibody.
Left wrist excisional biopsy with synovitis resection and flexor retinaculum release was then performed. Flexor tendons were also widely debrided. A dense yellow granulated fluid was seen during the operation (Figure 2). Perioperative specimens were sent to pathology and microbiology. A tuberculosis culture was analysed in addition. Pathologic examination showed fibrous cyst with giant cells and the microbiologic examination revealed M. tuberculosis.
After thorough debridement, antibacillary chemotherapy administered over an 9-month period promoted full healing and positive results in this patient, including disappearance of the swelling after 2 months of treatment and a normal range of motion after 6 months without recurrence within 2 years (Figure 3).
Since 1950s, the incidence of tuberculous infection has gradually decreased due to anti-tuberculous chemotherapy. However, this trend has been reversing recently because of the increased number of patients infected with HIV, bacterial resistance to medications, and increased international travel and immigration. Thus, the incidence of extrapulmonary tuberculosis, including musculoskeletal tuberculosis, has also been rising.2
Tuberculous infection of the musculoskeletal system accounts for 10% of all extrapulmonary cases of tuberculosis. In musculoskeletal tuberculous infections, the involvement of tuberculosis in peripheral joints and tendons is rare. If left untreated, tuberculosis can cause serious joint and tendon damage as well as the spread of mycobacteria into the surrounding bursa, muscle, and other soft tissues. Concurrent active pulmonary tuberculosis is present in less than 50% of the patients.2,5
As in our case, the diagnosis of the tuberculous tenosynovitis may be either difficult or delayed due to its non specific symptoms as well as its insidious onset. The inflammatory tenosynovitis around the carpal tunnel may compress the median nerve, mimicking the symptoms of canal carpal syndrome due to a mechanical cause.6
The incidental finding may be supposed to be the most common presentation for tuberculous tenosynovitis. The infection of the tendon sheath may result from the hematogenous dissemination of the bacillus. However, direct inoculation of the tendon sheath by the Koch bacillus was also reported.6
The wrist x-ray may not show any abnormality, except chronic cases with sequel. The magnetic resonance imaging usually confirms the chronic tenosynovitis, but not the specific origin of the disease. It is essential for a complete examination of the whole tendon, exploring any tendon lesion or joint involvement.
The definitive diagnosis of the tuberculosis unavoidably depends on histopathological analysis of the tissue sampling showing epitheloid granulomas and giant cells with central caseous necrosis and also bacteriological cultures.7
The currently recommended 6-month course is often adequate with extensive curettage, lavage and synovectomy. Surgery is essential, but the extent of surgical debridement is still debatable.3,8
The possibility of tuberculous tenosynovitis should be considered for an insidious hand weakness that occurs in the absence of external injuries. Characteristic MRI findings and the anatomic correlation of flexor tendon sheath with wrist bursa are helpful in differentiating tuberculous tenosynovitis from other causes. The early diagnosis could have facilitated proper management in this case. We highlight the importance of histopathologic and microbiological analysis of the excised material.
If in the first surgery had been performed microbiological analysis, the diagnosis would have been made and the second surgery would have been programmed differently
All the other colleagues that helped to treat this patient.
None.

©2016 Freitas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.