MOJ
eISSN: 2374-6939


Research Article Volume 12 Issue 1
1Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Bangladesh
2Professor, FCPS, Bari-Ilizarov Orthopaedic Centre, Bangladesh
3Medical officer, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Mofakhkharul Bari, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Professor, Russian Ilizarov Scientific Centre, Kurgan, 1/1, Suvastu Shirazi Square, Lalmatia, Dhaka-1207, Bangladesh, Tel +88 01819 211595
Received: January 23, 2020 | Published: February 7, 2020
Citation: Bari M, Shahidul I, Bari AMSR. Trifocal bone transport by Ilizarov technique for large post-traumatic tibial bone defects: a single centre BARIILIZAROV experience of 46 cases. MOJ Orthop Rheumatol. 2020;12(1):12-14. DOI: 10.15406/mojor.2020.12.00507
Purpose: The Aim of this study was to evaluate the clinical and functional outcome of patients with large post-traumatic tibial bone defects managed by Trifocal bone transport using the Ilizarov technique.
Methods: We retrospectively reviewed 46 cases of 38.2 years (range, 15.0-68.0years). The bone defects averaged 10.5±3.5cm (range: 6.5cm–20.5cm) after radical debridement and it was managed by trifocal bone transport.
Results: The mean duration of follow up after Ilizarov frame removal was 28.5±1.5months (range 10.0-24.0months). All patients achieved complete union in both the regenerates. The mean bone transport time was 50.6±20.5days (range 30.0-130.0days). The mean Ilizarov fixator time was 1.2±0.4months/cm (range 0.8-2.2months/cm). The bone results were excellent in 40 patients and good in 6 patients. The functional results were excellent in 42 patients and good in 4 patients.
Conclusion: Trifocal bone transport is a safe, reliable and successful methods for large post-traumatic tibial bone defects in one stage surgery.
Keywords: bone defects, bone transport, Ilizarov technique, trifocal approach
Post-traumatic large bone tibial and soft tissue defects following high energy trauma presents a great challenge for Orthopaedic and Reconstructive surgeons. Bone transport by Ilizarov technique is the gold standard method for the treatment of large bone defects. Nonunion, deformity, persistent infection, bone defect and shortening can be addressed simultaneously using the academician Ilizarov principles and technique.1–3 The Ilizarov method is divided into 3 categories depending on the type of treatment.
The monofocal approach closes bone and soft tissue defects directly. Acute shortening >3cm may compromise the vasculature and lead to limb ishchaemia. The fibula must have a defect to match the tibial defect.4 Conventional single level bone transport bridged bone defects in the majority of cases, when the defect is >7cm, the complications of bone transport including prolonged fixation in the Ilizarov frame, hypoplastic bone formation in the regenerate tend to increase.4,5 Kurgan, Russia researches proposed that trifocal bone transport should be used to reduce those complications when bone defect is 7cm or greater.1,4,6 In this original paper we are presenting our experience in successful treatment of large post-traumatic tibial bone and soft tissue defects by trifocal bone transport using the Ilizarov technique in a series of 46 cases where conventional orthopaedic approaches are often inadequate and inappropriate.
We respectively reviewed a series of 46 patients who were managed with the Ilizarov technique of bone transport between January 2005 and January 2018 at our Bari-Ilizarov Orthopaedic Centre. The inclusion criteria’s were the following-
In this study included 36 males and 10 females with a mean age of 38.2 years (range, 15.0-68.0 years). The causes of injury included motor vehicle accidents in 30 patients, explosive injury in 5 patients, crush-related injury in 10 patients and fall from height in one patient. All were open fractures, including Gustilo II in 7, Gustilo IIIA in 15, Gustilo IIIB in 20, and Gustilo IIIC in 2 patients. The mean duration from time of injury to application of the Ilizarov frame was 15.5 months (range, 2.0-40.0months). Defects with infection were located in the proximal tibia in 16 patients, the middle tibia in 21 patients and the distal tibia in 10 patients.
The patient was in supine position under spinal anesthesia. All implants were removed. Radical debridement of all inflammatory granulation tissues and infected devitalized bones were performed.7 Soft tissue and bone specimens were sent for culture. The mean area of soft tissue defect after debridement was 8.5cmx5.5cm (range: 5.5cmx2.5cm to 20.0cmx10.0cm), and the mean bone defects was 10.5±3.5cm (range: 5.5cm-20.5cm), which were measured intra-operatively. After the debridement Ilizarov frame was applied for every patient. For mid tibia defect, two rings were placed in the proximal and two rings in the distal tibia. Sometimes we put 3 rings in the distal tibia for more stability. Two corticotomies were performed: one in the proximal and other in the distal tibia between each of the rings. Converging transport was performed. All cases were followed by bone transport and resume limb length.
Bone transport started after a latent of 5 to 7 days. For converged bone transport, each fragment of both sides of the bone defect proceeded at a rate of 1mm/day, which was divided into 4 times of 0.25mm each. Thus, the distraction rate at each site of corticotomy should be 1mm/day, and the bone defect was shortened 2mm/day. The modes of trifocal approach (double level bone transport) are shown in the diagrams (Figure 1).
Radiographs were reviewed monthly to monitor the progress of bone transport and quality of the regenerate during transport. After docking, X-ray films were taken every two months to assess consolidation of the regenerate and healing of the docking site. Using the criteria of Fischgrund et al.8 when radiographs showed that three complete cortices had formed in the regenerate, and bone healing was achieved in the docking site, the Ilizarov frame was removed and plaster was applied.
Bone and functional results were evaluated according to the Association for the Study and Application of the Method of Ilizarov (ASAMI) criteria.4 Bone results were evaluated based on union, infection, deformity, and limb length discrepancy and classified as excellent, good, fair, and poor. The functional results were evaluated according to limp, range of motion and return to activity and classified as excellent good, fair, and poor.4
The mean follow-up duration after removal of Ilizarov ring was 28.5±1.5months (range, 10.0-24.0months). All patients achieved complete union in both the regenerates. The mean bone transport time was 50.6±20.5 days (range 30.0-130.0days). The mean soft tissue healing duration was 2.5±3.0months (range, 1.0-5.0months). The mean consolidation duration of the distraction gap was 10.8±3.0months/cm (range, 5.0-16.0months/cm). The mean Ilizarov fixator time was 12.0±0.4months/cm (range, 0.8-2.2months/cm). The bone results were excellent in 40 patients and good in 6 patients. The functional results were excellent in 42 patients and good in 4 patients. The typical case is illustrated in Figure 2.
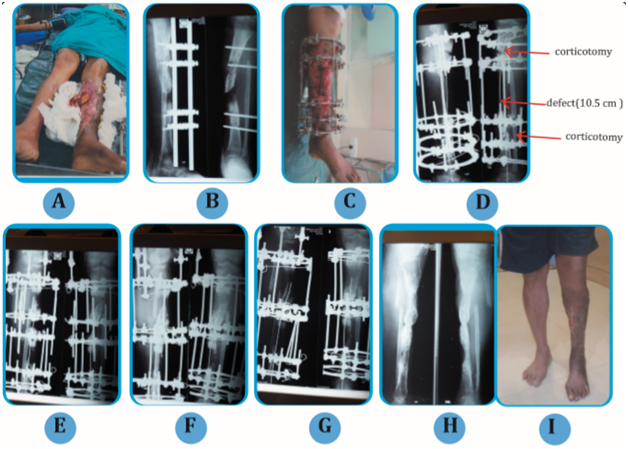
Figure 2 (A) Picture of 35 years old man with G lll B. (B) Radiograph of left tibia-fibula with uniaxial fixator in situ, done elsewhere. (C) Picture of left leg with Ilizarov in situ. (D) Radiograph of left tibia-fibula after debridement with proximal & distal corticotomy. (E) Radiograph of left tibia-fibula with Ilizarov in situ after 2 months. (F) Radiograph of left tibia-fibula after 3 months. (G) Radiograph of left tibia-fibula after 11 months. (H) Final radiograph of left tibia-fibula after 1 year and 6 months. (I) Clinical picture of the patient.
In all our cases no flap cover was needed and bone transport was achieved nicely. Bone grafting was not done in any case and that is the violation of the Ilizarov principles and rule. We achieved good contact in the docking site in all the cases. The soft tissue defects were closed gradually during bone transportation. We put guide wire in the whole tibia to maintain the axis and to prevent the deviation. One nonunion occurred at the docking site due to invaginated soft tissue, and refreshened the bone ends and achieved a good contact and excellent union.
The management of large post-traumatic tibial bone and soft tissue defects remains a challenge for Orthopaedic and Reconstructive surgeons. Conventional treatments have been proposed, including flap transfer with combined or autologous bone grafting, vascularized fibular grafts, Masquelet technique, and bone transport.1,4,5 Autologous bone graft is geared toward smaller defects typically because of its limited quantity; for larger defects, graft is harvested from more than one site, increasing the morbidity of the donor site (Table 1–3). Furthermore; even though vascularized fibular grafts have been successfully used to bridge massive bone defects, the operation demands high technical expertise and causes great trauma, and complications of stress fracture and nonunion have usually occurred.1–5 Masquelet technique can reconstruct large bone defect, but the procedure requires two steps to complete, including debridement, spacer insertion and wound closure, and bone graft is performed six to eight weeks later. For large bone defects, the source of bone graft is a big problem.5,9 Ilizarov bone transport has become a gold standard for the treatment of massive tibial bone defects, it could eradicate infection and solve bone and soft tissue defects at the same time.1 Traditional Ilizarov bone transport universally adopts single level transport to bridge massive bone defects. The drawbacks of the method are the lengthy Ilizarov frame time. Several studies of single level bone transport have shown that the Ilizarov fixation index ranges from 1.2 to 2.8months/cm with an average of 2.0months/cm.1,4,7,8,10 According to the calculation, if the size of bone defect is 10cm, Ilizarov fixation takes more than 20months. To decrease the fixation time, Borzunov et al.6 firstly proposed that one-stage double level or multilevel bone transport for massive bone defect to shorten distraction time and Ilizarov fixation time. Their clinical outcomes demonstrated that the duration of distraction could be reduced 2.5 times and fixation from 1.3 to 1.9times with the double level technique compared with the traditional single level technique. In our study, the average size of bone defect was 10.9±3.8cm. The mean compression/distractions 50.6±20.5days and the mean Ilizarov fixator time was 1.2±0.4months/cm.11,12
Case No. |
Age (Yr)/sex |
Fracture type: Gustilo |
Nonunion site |
No. of previous surgery |
Bone defect (cm) |
Soft tissue defect (cm*cm) |
Bone treatment surgery |
Infecting organism |
1 |
15,M |
IIIA |
distal tibia diaphysis |
3 |
6.5 |
7.0×3.5 |
Converging transport |
MRSA |
2 |
35,M |
IIIB |
middle tibia diaphysis |
4 |
12.0 |
4.5×3.0 |
shortening, lengthening |
MRSA |
3 |
48,F |
IIIA |
middle tibia diaphysis |
2 |
13.0 |
7.0×3.5 |
shortening, lengthening |
MRSA |
4 |
47,M |
IIIB |
middle tibia diaphysis |
4 |
9.0 |
6.8×3.5 |
Converging transport |
MRSA |
5 |
26,M |
IIIB |
proximal tibia diaphysis |
3 |
16.0 |
7.0×10.5 |
Converging transport |
MRSA |
6 |
38,M |
IIIB |
proximal tibia diaphysis |
4 |
8.0 |
8.0×3.5 |
Converging transport |
Pseudomonas aeniginosa |
7 |
32,M |
IIIA |
distal tibia diaphysis |
2 |
7.0 |
7.0×3.5 |
Retrograde transport |
MRSA |
8 |
65,M |
IIIB |
middle tibia diaphysis |
2 |
10.3 |
12.5×3.5 |
Retrograde transport |
Acinetobacter bawnannii |
9 |
46,F |
IIIB |
proximal tibia diaphysis |
3 |
9.5 |
10.0×3.5 |
Antegrade transport |
MRSA |
10 |
15,F |
II |
middle tibia diaphysis |
3 |
8.0 |
9.0×3.0 |
Converging transport |
MRSA |
11 |
49,M |
IIIA |
proximal tibia diaphysis |
4 |
11.8 |
6.0×2.5 |
Converging transport |
MRSA |
12 |
48,M |
IIIA |
distal tibia diaphysis |
5 |
13.5 |
12.0×3.5 |
Acute shortening |
MRSA |
13 |
34,M |
IIIB |
proximal tibia diaphysis |
3 |
12.5 |
7.0×3.5 |
Retrograde transport |
MRSA |
14 |
30,M |
IIIA |
middle tibia diaphysis |
5 |
4.5 |
4.5×3.0 |
Converging transport |
MRSA |
15 |
50,F |
IIIB |
middle tibia diaphysis |
4 |
7.0 |
7.0×3.5 |
Converging transport |
MRSA |
16 |
27,M |
IIIC |
distal tibia diaphysis |
2 |
5.5 |
6.8×3.5 |
shortening, lengthening |
MRSA |
17 |
32,F |
IIIA |
distal tibia diaphysis |
6 |
6.5 |
7.0×10.5 |
shortening, lengthening |
MRSA |
18 |
38,M |
IIIA |
middle tibia diaphysis |
3 |
12.0 |
8.0×3.5 |
Converging transport |
MRSA |
19 |
32,M |
IIIA |
middle tibia diaphysis |
2 |
13.0 |
7.0×3.5 |
Converging transport |
MRSA |
20 |
68,M |
IIIB |
middle tibia diaphysis |
6 |
9.0 |
4.6×3.5 |
Converging transport |
MRSA |
21 |
46,F |
IIIA |
proximal tibia diaphysis |
3 |
16.0 |
3.50×3.5 |
Retrograde transport |
MRSA |
22 |
47,M |
IIIB |
proximal tibia diaphysis |
4 |
8.0 |
5.50×3.5 |
Retrograde transport |
MRSA |
23 |
46,M |
IIIA |
distal tibia diaphysis |
7 |
7.2 |
9.0×3.5 |
Converging transport |
MRSA |
24 |
49,F |
II |
middle tibia diaphysis |
3 |
9 |
7.0×10.5 |
time in frame (months) |
MRSA |
25 |
48,M |
IIIA |
middle tibia diaphysis |
4 |
16 |
8.0×3.5 |
Converging transport |
MRSA |
26 |
34,M |
IIIA |
distal tibia diaphysis |
1 |
8 |
7.0×10.5 |
Converging transport |
MRSA |
27 |
30,M |
IIIB |
proximal tibia diaphysis |
2 |
7.2 |
12.0×3.5 |
Acute shortening |
MRSA |
28 |
30,F |
IIIA |
middle tibia diaphysis |
3 |
10.3 |
10.0×3.5 |
Retrograde transport |
MRSA |
29 |
27,M |
IIIB |
middle tibia diaphysis |
3 |
9.5 |
9.0×3.0 |
Converging transport |
MRSA |
30 |
32,M |
IIIC |
proximal tibia diaphysis |
4 |
8 |
6.0×2.5 |
Converging transport |
MRSA |
31 |
67,M |
IIIA |
distal tibia diaphysis |
5 |
11.8 |
12.0×3.5 |
shortening, lengthening |
PMRSA |
32 |
46,M |
IIIB |
proximal tibia diaphysis |
3 |
13.5 |
7.0×3.5 |
shortening, lengthening |
MRSA |
33 |
16,M |
IIIA |
middle tibia diaphysis |
5 |
12.5 |
7.0×10.5 |
Converging transport |
MRSA |
34 |
49,F |
IIIB |
4 |
4.5 |
8.0×3.5 |
Converging transport |
MRSA |
Table 1 Demographic data of patients
Case No. |
Age (Yr/sex) |
Fracture type: Gustilo |
Nonunion site |
No. of previous surgery |
Bone defect (cm) |
Soft tissue defect (cm*cm) |
Bone treatment surgery |
Infecting organism |
34 |
27,M |
A |
proximal tibia diaphysis |
3.0 |
3.7 |
12.0×3.5 |
Converging transport |
MRSA |
35 |
32,M |
IIIA |
middle tibia diaphysis |
5.0 |
7.0 |
7.0×3.5 |
Converging transport |
MRSA |
36 |
65,M |
IIIB |
middle tibia diaphysis |
4.0 |
5.5 |
4.0.0×3.0 |
shortening lengthening |
MRSA |
37 |
38,M |
IIIA |
proximal tibia diaphysis |
8.0 |
6.5 |
7.0×3.5 |
Converging transport |
MRSA |
38 |
32,M |
IIIB |
distal tibia diaphysis |
6.0 |
12.0 |
6.8.5×3.5 |
Converging transport |
MRSA |
39 |
65,M |
IIIC |
middle tibia diaphysis |
7.0 |
13.0 |
7.0×10.5 |
Converging transport |
MRSA |
40 |
46,F |
IIIA |
middle tibia diaphysis |
2.0 |
9.0 |
8.0×3.5 |
Retrograde transport |
MRSA |
41 |
47,M |
IIIA |
proximal tibia diaphysis |
6.0 |
16.0 |
7.0×3.5 |
Converging transport |
MRSA |
42 |
46,M |
IIIA |
proximal tibia diaphysis |
3.0 |
8.0 |
12.0×3.5 |
Time in frame (months) |
MRSA |
43 |
49,M |
IIIB |
proximal tibia diaphysis |
4.0 |
7.2 |
4.6.0×3.5 |
Converging transport |
MRSA |
44 |
48,M |
IIIA |
distal tibia diaphysis |
7.0 |
9.0 |
3.50×3.5 |
Converging transport |
MRSA |
45 |
34,M |
IIIB |
middle tibia diaphysis |
3.0 |
16.0 |
5.50×3.5 |
Acute shortening |
PMRSA |
46 |
30,F |
IIIA |
middle tibia diaphysis |
4.0 |
8.0 |
9.0×3.5 |
Retrograde transport |
MRSA |
Case No. |
Bone transport time(days) |
Surgical docking site procedure |
Wound treatment strategy |
Soft tissue union time (months) |
Consolidation of the distraction gap (months) |
Union time of the docking site time (months) |
Time in frame (months) |
Ilizarov fixation index (months/cm) |
1 |
27,M |
directly docking |
heal itself |
3.5 |
12.0 |
6.5 |
9.0 |
1.1 |
2 |
32,M |
open bone graft |
heal itself |
5.5 |
8.0 |
8.0 |
5.0 |
2.1 |
3 |
65,M |
directly docking |
heal itself |
4.6 |
7.0 |
5.0 |
11.0 |
2.0 |
4 |
38,M |
directly docking |
skin grafting |
2.5 |
13.0 |
6.0 |
13.0 |
0.9 |
5 |
32,M |
directly docking |
heal itself |
6.0 |
8.0 |
9.0 |
605 |
1.4 |
6 |
65,M |
nonunion bone graft |
cross leg flap |
3.5 |
5.0 |
11.0 |
9.0 |
0.8 |
7 |
46,F |
open bone graft |
heal itself |
2.3 |
6.0 |
7.0 |
18.0 |
1.5 |
8 |
47,M |
directly docking |
heal itself |
6.0 |
9.0 |
10.0 |
14.0 |
2.0 |
9 |
46,F |
open bone graft |
heal itself |
3.7 |
11.0 |
6.0 |
12.0 |
0.9 |
10 |
49,F |
directly docking |
skin grafting |
4.5 |
5.0 |
9.0 |
15.0 |
1.6 |
11 |
48,M |
directly docking |
heal itself |
2.8 |
7.0 |
11.5 |
7.5 |
1.0 |
12 |
34,M |
directly docking |
cross leg flap |
6.2 |
10.0 |
3.5 |
8.0 |
0.8 |
13 |
30,F |
open bone graft |
closed directly |
4.4 |
4.0 |
9.0 |
11.5 |
1.2 |
Table 2 Demographic data of patients
Case No |
Bone transport time(days) |
Surgical docking site procedure |
Wound treatment strategy |
Soft tissue union time(months) |
Consolidation of the distraction gap(months) |
union time of the docking site time(months) |
Time in frame(months) |
Ilizarov fixation index(months/cm) |
14 |
40 |
directly docking |
Heal itself |
4.6 |
6.5 |
14.0 |
0.9 |
|
15 |
45 |
directly docking |
Heal itself |
2.5 |
8.0 |
8.0 |
12.0 |
1.4 |
16 |
30 |
directly docking |
Heal itself |
6.0 |
5.0 |
5.0 |
15.0 |
0.8 |
17 |
65 |
directly docking |
Heal itself |
3.5 |
6.0 |
6.0 |
7.5 |
1.5 |
18 |
80 |
directly docking |
Heal itself |
2.3 |
9.0 |
9.0 |
8.0 |
2.0 |
19 |
35 |
directly docking |
Skin grafting |
6.0 |
11.0 |
11.0 |
11.5 |
0.9 |
20 |
45 |
directly docking |
Heal itself |
3.7 |
5.0 |
7.0 |
9.0 |
1.6 |
21 |
55 |
directly docking |
Heal itself |
4.5 |
7.0 |
10 |
5.0 |
1.0 |
22 |
70 |
directly docking |
Heal itself |
2.8 |
10.0 |
6.0 |
11.0 |
0.8 |
23 |
50 |
directly docking |
Heal itself |
6.2 |
12.0 |
9.0 |
13.0 |
1.2 |
24 |
65 |
directly docking |
Heal itself |
4.4 |
8.0 |
11.5 |
605 |
1.4 |
25 |
40 |
directly docking |
Heal itself |
3.5 |
70.0 |
3.5 |
9.0 |
0.8 |
26 |
90 |
directly docking |
Heal itself |
5.5 |
13.0 |
9.0 |
18.0 |
1.5 |
27 |
80 |
directly docking |
Heal itself |
4.6 |
8.0 |
5.0 |
14.0 |
2.0 |
28 |
60 |
directly docking |
Skin grafting |
2.5 |
5.0 |
6.0 |
12.0 |
0.9 |
29 |
30 |
directly docking |
Heal itself |
6.0 |
6.0 |
9.0 |
15.0 |
1.6 |
30 |
45 |
directly docking |
Heal itself |
3.5 |
9.0 |
11.0 |
7.5 |
1.0 |
31 |
75 |
directly docking |
Heal itself |
2.3 |
11.0 |
7.0 |
8.0 |
0.8 |
32 |
70 |
directly docking |
Heal itself |
6.0 |
5.0 |
10.0 |
11.5 |
1.2 |
33 |
60 |
directly docking |
Heal itself |
3.7 |
7.0 |
6.0 |
7.5 |
1.1 |
34 |
30 |
directly docking |
Skin grafting |
4.5 |
10.0 |
9.0 |
8.0 |
2.1 |
35 |
95 |
directly docking |
Heal itself |
2.8 |
4.0 |
11.5 |
11.5 |
2.0 |
36 |
48 |
directly docking |
Heal itself |
6.2 |
7.0 |
6.0 |
9.0 |
0.9 |
37 |
85 |
directly docking |
Heal itself |
4.4 |
10.0 |
9.0 |
5.0 |
1.4 |
38 |
65 |
directly docking |
Heal itself |
4.4 |
12.0 |
11.5 |
11.0 |
0.8 |
39 |
35 |
directly docking |
Heal itself |
3.5 |
8.0 |
3.5 |
13.0 |
1.5 |
40 |
39 |
directly docking |
Skin grafting |
5.5 |
70.0 |
9.0 |
605 |
2.0 |
41 |
42 |
directly docking |
Heal itself |
4.6 |
13.0 |
5.0 |
9.0 |
0.9 |
42 |
45 |
directly docking |
Heal itself |
2.5 |
8.0 |
6.0 |
18.0 |
1.6 |
43 |
68 |
directly docking |
Closed directly |
6.0 |
5.0 |
9.0 |
14.0 |
1.0 |
44 |
70 |
directly docking |
Heal itself |
3.5 |
6.0 |
10.0 |
7.5 |
0.8 |
45 |
90 |
directly docking |
Heal itself |
2.3 |
9.0 |
6.0 |
8.0 |
1.2 |
46 |
84 |
directly docking |
Heal itself |
3.5 |
8.0 |
9.0 |
11.5 |
0.7 |
Table 3 Demographic data of patients
Borzunov et al.5 believed that hypoplastic bone formation could happen during defect filling when a single-level distraction regenerate was grown to >5cm or to the length that exceeded 40% of the original segment. All bone defects of our patients are >7.0cm and averaged at 1cm. According to our observations and experiences, we consider using double level transport if the defect is ≥7.0cm. This could facilitate earlier docking at the bone defect site. We encountered one delayed union or non-union of the docking site as a result of soft tissue interposition, poor blood supply, and poor contact from mismatch of coapting surface.
In conclusion, the Ilizarov technique of trifocal bone transport is a safe, reliable and successful methods for large post-traumatic tibial bone defects in one stage surgery. It could significantly shorten frame time, decrease bone transport time, and reduce total treatment time.
None.
All authors declare no conflict of interest.
None.

©2020 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.