MOJ
eISSN: 2374-6939


Case Report Volume 8 Issue 1
1Department of Orthopaedics, Hospital Tengku Ampuan Rahimah Klang, Selangor, Malaysia
2Chief Consultant, Bari-Ilizarov Orthpaedic Centre, Visiting and Honoured Professor Russian Scintific Centre, Russia
3Bari-Ilizarov Centre, Dhaka, Bangladesh
Correspondence: Premganesh Ganaisan, Department of Orthopaedics, Hospital Tengku Ampuan Rahimah Klang, Selangor, Malaysia
Received: April 18, 2017 | Published: April 20, 2017
Citation: Ganaisan P, Bari MM, Rahman M, Islam S (2017) Treatment of Osteopetrosis-related Subtrochanteric Fracture Using the Ilizarov Compression- Distraction Device: A Case Report. MOJ Orthop Rheumatol 8(1): 00300. DOI: 10.15406/mojor.2017.08.00300
Osteopetrosis is a rare inherited skeletal disorder characterized by bone fragility. Variable options of treatment modalities have been applied each with its relative intraoperative and post-operative complications. We present a case fixed using the Ilizarov Compression-Distraction device.
ICD, Ilizarov Compression-Distraction, ADO, Adult Dominant Osteopetrosis
Osteopetrosis is a rare hereditary bone disease characterized by increased bone density.1-4 There is a failure of bone remodeling due to disease of the osteoclasts.. It is clinically divided to 3 subtypes: infantile-malignant autosomal recessive; intermediate autosomal recessive and adult benign autosomal dominant (ADO). The ADO has two subtypes: Type 1 (ADO 1) which involves long bones, cranial vault and spine ; and type 2 (ADO 2) which displays end-plate thickening of the verterbrae “rugger-jersey spine” and the endobones “bone-within-bone” radiographic appearance of the pelvis. ADO 2 patients are usually asymptomatic and are diagnosed either incidentally or while presenting with a fracture as although the density increases, the mechanical strength is decreased.5 Literature has documented various treatment options-surgical and conservative, with their respective outcomes.3-7 The common feature noted is the difficulty faced intra-operatively due to the hard, dense bone resulting in equipment failure, prolonged surgery, suboptimal fixations and complications to the patient- blood loss, tissue and bone damage. We report a case of ADO 2 which was fixed using the ICD device with a good outcome
A 26 year lady, a known case of ADO 2, was referred to our center following a fall at home one month earlier. Her district hospital team had suggested a trial of conservative treatment, but due to the persistent pain and discomfort of immobilization she requested for surgical intervention. Despite sustaining the injury a month earlier, she was still suffering from substantial pain. Radiographs showed a subtrochanteric fracture of the left femur- Seinsheimer 2A without healing callus. After ruling out other injuries, skin traction was applied. The treatment options and all possible complications- intra, immediate and delayed post-operative were explained to her and the family. A collective decision was made to apply an ICD as we aimed to minimize operative time, reduce possible damage to tissue and bone, and limit surgical scarring. The necessary pre-operative investigations were done, and optimized where needed.
After spinal anesthesia was administered, she was placed on a traction table and under an image-intensifier a closed manual reduction was attempted to reduce the displacement as much as possible. But as expected, the proximal segment was significantly displaced upward- flexed and externally rotated. The decision was made to apply the ICD framework, and use the components to reduce the fracture- a benefit of the ICD system. 1.8 millimeter Russian made biocompatible olive wires and 5.0 millimeter tapered schanz pins were inserted based on the safe zones followed by the rings and arches. The initial deformity was well reduced in the coronal plane but was unsatisfactory in the sagittal plane. Taking into account the duration of the injury-specifically the contracted surrounding muscles, we applied a translation device for a gradual and controlled reduction. This also prevented the necessity of an open reduction, thus minimizing operative time, preventing blood loss, and the risk of fracture propagation if we had tried re-manipulation. Post-operatively the limb was clinically well-aligned (Figures 1 & 2).
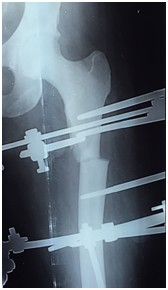
Figure 1 Immediate postoperative radiograph in the coronal view showing a mild coronal and roational displacement.
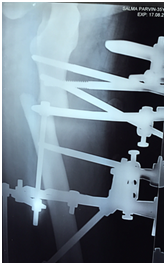
Figure 2 Immediate postoperative radiograph in the sagittal view showing a significant displacement.
The total surgical time was about 50 minutes. There was negligible blood loss as only stab incisions were made for the schanz pins entry. Post- operative pain was well managed with just opioids for a fixed duration of three days, and on a ‘prn’ basis subsequently. She was advised partial-weight bearing mobilization the day after surgery, and over the course of the translation period. The translation process was ceased after five days when radiographs showed good bony contact and alignment in both coronal and sagittal planes. Thereafter she was encouraged for full-weight bearing with a use of aid when required (Figure 3).
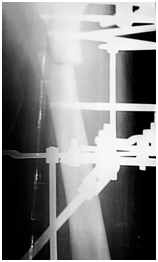
Figure 3 Radiograph in the sagittal view at day 5 of translation showing a well approximated fragment.
Follow-ups were scheduled initially at two and four weeks. She was also supplemented with calcitriol at 1200mg per day. The fracture united at 22 weeks following surgery with the patient ambulating well and pain free (Figures 4-6).
Osteopetrosis is a rare hereditary bone disease characterized by increased bone density.1-4 There is a failure of bone remodeling due to disease of the osteoclasts. Studies suggest three different genetic mutations which affect the osteoclasts ability to acidify bone during remodeling.5 The result is a dense but mechanically weak bone. The fracture callus shows no Haversian canals.5 This patient was an ADO type 2, first described by Albers-Schoenberg, who presented with the fracture following a trivial injury.3,5
Despite literature showing non-operative treatment as a feasible option.4,5 we opted against controlled-traction and casting. As the patient was young, we wanted her to start mobilizing early to prevent joint contractures and other complications associated with prolonged traction- pressure sores, orthostatic pneumonia. Besides running the risk of non-union, we also wanted to avoid malunion, which was anticipated as the fracture was already a month old and any attempts of reduction would be futile.
The choice of the surgical technique was based on many factors. We reviewed literature3-7 on the intraoperative and post-operative complications associated with the various surgical techniques, and the subsequent outcomes. Hardware failure and breakage- due to the dense bone are the main intraoperative complications, which in turn lead to prolonged operative time, excessive bleeding, periosteum and tissue damage. These issues either directly or indirectly lead to an array of post-operative complications such as delayed union, non-union, infection, osteomyelitis, hardware failure- breakage, cut-out; and also there complications experienced during removal of implant and revision surgery, if required.4-7
We attribute the success of this treatment due to the versatility of the ICD method- a stable and quick construct using wires and schanz pins.. This avoids the necessity for an open reduction and the associated complications- blood loss, tissue and periosteum damage, besides minimizing operative time. The versatility of the ICD system permitted us to apply a translation device to gradually correct the initial sagittal displacement, negating theneed for an open reduction of a month old fracture. The ‘multi-dimensional’ construct permits early weight bearing, which in-turn stimulates bone healing, prevents joint contractures in addition to a shorter period of immobilization.
The fracture united at 22 weeks, which is within the range documented in literature.4,5 A major contributing factor to the healing is the ICD‘tension-stress’ principle, which coupled with the micro-motion at bone-wire interface stimulates osteogenesis, angiogenesis and desmogenesis.8 An important component to the system is the specially designed Russian 1.8millimeter bio-compatible bayonet olive-wires we used. The sharp ‘cutting-tips’ of these wires permit a faster, and hence a more efficient bone penetration. This in-turn, optimizes operative time by preventing equipment failure, and most importantly minimizes periosteum and tissue damage- aiding to faster healing and union (Figure 7).
None.
None.

©2017 Ganaisan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.