MOJ
eISSN: 2374-6939


Research Article Volume 8 Issue 3
Department of Orthopedic and Traumatology, Al-Azhar University, Egypt
Correspondence: Nagy Abdulraheem Seleem, Lecturer of Orthopedic Surgery, Al-Azhar University, Faculty of Medicine, Cairo, Egypt, Tel 201000000000
Received: March 21, 2015 | Published: June 7, 2017
Citation: Alsebaey AA, Seleem NA (2017) Transforaminal Lumber Interbody Fusion in Management of Degenerative Lumber Disc Disease. Research Article 8(3): 00316. DOI: 10.15406/mojor.2017.08.00316
Study design: Prospective Cohort study.
Objectives of the study: To assess the clinical and radiological outcomes of TLIF in the management of degenerative lumbar disc diseases and to demonstrate the safety, surgical efficacy, and advantages of the transforaminal approach for lumbar interbody fusion.
Methods: Twenty patients with degenerative lumbar disc diseases were treated with TLIF and were followed up for 24 months. The clinical outcomes were assessed by Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) questionnaire. The radiographic fusion was assessed by Brantigan and Steffee criteria for radiographic fusion.
Results: Low back and leg pain completely resolved in 18 patients (90%).Solid fusion achieved in 18 patients (90%), whereas pseudo arthrosis documented in two patients. Complications reported post-operatively; Dural tear reported in 2 cases (10%), early post-operative wound infection reported in one case (5%), neurological deficit reported in one case (5%), Cage subsidence reported in one case (5%), Pseudo arthrosis reported in 2 cases (10%) and poor improvement of low back pain also reported in 2 cases (10%).
Conclusion: Transforaminal lumbar interbody fusion is a safe and effective method for achieving circumferential spinal fusion via a single stage procedure. Interbody cages in degenerative lumbar disc diseases are useful to increase neuroforaminal height and to improve the chances of achieving a successful 360˚ fusion.
Keywords: Degenerative lumbar disc diseases, Transforaminal approach, Interbody fusion
Approximately 70% to 85% of adults will be affected by low back pain (LBP) at some point during their lifetimes. Numerous anatomic sites can be responsible for the pain, and accurate diagnosis is often difficult. Degenerative disc disease (DDD), internal disc disruption, lumbar disc herniation, and facet joint arthritis, as well as intra-abdominal pathology, are all potential causes of LBP.1 Patients with DDD or discogenic back pain can present with a constellation of symptoms that range from benign LBP to excruciating back pain with lower extremity symptoms. Continued degeneration of the affected disc can lead to secondary problems such as degenerative spondylolisthesis, lumbar stenosis, and facet arthrosis.2 Methods of spinal arthrodesis continue to evolve in efforts to treat back pain. The latest techniques include approaching from anterior, posterior, lateral and posterolateral. Interbody fusion techniques have been developed to provide solid fixation of spinal segments while maintaining load bearing capacity and proper disc height.3 The ability to reconstruct the anterior column after disc removal is important because 80% of the compressive, torsion, and shear forces are transmitted through the anterior column.4
Reconstruction of the anterior column can be performed via the anterior approach, with direct transperitoneal or retroperitoneal access to the lumbar spine. Posterior fusion and instrumentation can be added to obtain a 360 degree fusion. This technique involves two surgical approaches, with increased operating time (compared to posterolateral fusion) as well as potential complications related to anterior approaches to the lumbar spine. An alternative method of reconstructing the anterior column is via posterior lumbar interbody fusion.5 The transforaminal lumbar interbody fusion (TLIF) developed by Harms is a modification of the posterior lumbar interbody fusion (PLIF).6 The TLIF has been shown to be valuable alternative to the traditional PLIF.7 Advantages of the TLIF over PLIF are fewer complications, avoidance of epidural scarring, less intraoperative bleeding, and avoidance of dural injury. Further, given its unilateral approach, better preservation of the lumbar spine musculoligamentous complex is obtained.6
Objective
Prospective study was conducted between 2012 and 2014 in Bab El Shaareya University Hospital, Al-Azhar University involving 20 patients with degenerative lumbar disc diseases were treated operatively by TLIF technique using a PEEK Cages with pedicular screws and rods. Before starting study the ethics committee in Al-Azhar University, faculty of medicine approved it and consent was taken from all patients. The inclusion criteria were: (1) Patients with degenerative disc disease with or without disc herniation; Exclusion criteria were lumbar spine infections or tumors. All cases tried conservative measures for at least three months. The patients were twelve males and eight females. The average age at surgery was 45 years (36-62). 16 patients had a one-level fusion, most commonly affected level L4-L5 (10 patients), followed by L5-S1 (4 patients) and L3-L4 (2 patient). 4 patients had two levels of involvement.
Clinical and radiologic evaluations
All patients in this study were carefully assessed clinically in the form of detailed clinical history and thorough general and local examinations. For radiographic examination, standing anterior-posterior and lateral radiographs of the lumbar spine were performed. Flexion-extension lateral radiographs taken in the standing position were also done to discover whether hyper mobility exists at the spondylolisthetic level. Magnetic Resonance Imaging (MRI) was done for all patients preoperatively to demonstrate any impingement of the central spinal canal from disc herniation, degenerative spondylosis, or other conditions.
Surgical technique
All patients received general anaesthesia with endotracheal intubation; Foley's catheter was also applied to all patients for fluid balance during operation. Patients were operated in conventional operating room. One dose (1 gm.) of antibiotic was given intravenously for every patient at the induction of anesthesia. The patient was placed in prone position. The patient was positioned over cushions or pillows placed transversely under the chest and pelvis. The latter method avoided the metal of the frame being an obstacle in the field of C-arm beam. After sterilization and draping, a midline longitudinal incision was made at the affected vertebral level identified on lateral fluoroscopy. The fascia was incised in line with the skin incision, the paraspinous muscles were elevated, exposing the spine. Pedicle screws are placed in the vertebra above and below the disc to be fused. Slight distraction is performed opposite the intended decompression side. The exposure for the TLIF is achieved by removing the facet joint, hemi-lamina, and pars interarticularis region on one side of the spine using an osteotome or high-speed drill and Kerrisonrongeur. Foraminal blood vessels that lie in the inferior portion of the neuroforamen cauterized and divided using a bipolar unit before proceeding. The exiting nerve root identified, but vigorous exposure or retraction of the ganglion avoided. A nerve root retractor placed medially to protect the thecal sac. The disc space is incised between the thecal sac and exiting nerve root and a generous window was removed from the posterolateral annulus. Provisional discectomy was performed using curettes. The disc space was expanded with an interbody distractor or sequential disc space dilators to restore disc height and achieve indirect decompression of the foraminal zone. Distraction of the disc space using disc space dilators facilitated visualization within the disc space and allowed a complete discectomy to be performed. Vigorous distraction of the pedicle screws to achieve the disc space expansion was avoided because this practice may lead to loss of screw purchase. Once the disc space expansion has been achieved using interbody distraction, the pedicle screws on the side opposite the interbody approach were tightened over a temporary rod to maintain the distracted position. With the disc space adequately expanded, all disc material and cartilaginous endplate were thoroughly removed, leaving the bony endplates intact. Autogenous cancellous bone graft harvested from the iliac crest or taken from the posterior spinal elements during decompression, was then packed into the anterior and contralateral portions of the disc space to promote interbody fusion. The cage was packed with autogenous cancellous bone graft. The interbody space was then reconstructed by selecting an appropriately sized interbody cage. Trial implants were useful for ensuring optimal sizing of the interbody cage. The interbody cage was then impacted into the disc space. Additional cancellous graft materials were packed around the cage, filling any residual voids within the interbody space. Any distraction that has been temporarily used to hold opens the interbody space was released after placement of the interbody cage. Rods were attached to the pedicle screws, and gentle compression was applied to the construct. Before wound closure, a probe was used to confirm adequate space around the neural structures and ensure that no graft material has migrated into the foraminal region. In the recovery room; the patient was observed by a nurse and pulse oximeter was used to record the pulse and the oxygen saturation. The blood pressure was also checked and patient controlled analgesia was started. All patients received intravenous antibiotics for 5 days postoperatively, followed by oral antibiotics till discharge from the hospital. Patient controlled analgesia was continued for the first 36-48 hours. Hemoglobin level was checked in the first postoperative day. Fluids were also given through the intravenous line. Drains were removed on the 2nd postoperative day. Wound condition was followed during the first 2 weeks, which is the time by the end of which the wound is supposed to be healed and the stitches were removed. The patients were allowed out of bed on day one. Lumbosacral support was worn according to the bone quality during the operation. Isometric exercises of the abdominal and back muscles were started on day two.
Assessment was mainly subjective using the Visual Analogue Scale (VAS) for pain assessment pre-operative and at 6 weeks, 6 months, 12 months and 18 months and also using the Oswestry Disability Index (ODI) for disability and quality of life assessment pre-operative and at 6 weeks, 6 months, 12 months,18 months and 24 months. Plain X-rays were obtained at 3, 12, 18 and24 months to assess bony fusion.8,9
Fairbank and his colleagues interpreted "percentage of disability" scores in this manner:
Radiographic fusion
The post-operative Antero-posterior, lateral radiographs and dynamic views were used to assess the fusion mass at each level. The plain radiographs were obtained at 3 months, 6 months, 12 months, 18 months and 24 months to assess fusion status. Solid arthrodesis of the interbody space was confirmed by the presence of continuous bridging bone observed on the lateral radiographs, absence of lucencies around the cages, no cage migration or collapse and absence of halo around the screws. By Using this criteria, solid fusion was achieved in 18 patients (90%), whereas pseudarthrosis was documented in two patients. Low back and leg pain were completely resolved in 18 patients (90%) according to VAS (Table 1). All patients were rated minimal disability according to ODI (Table 2). The radiological outcome (Figure 1) showed solid fusion was achieved in 18 patients (90%), whereas pseudarthrosis was documented in two patients.
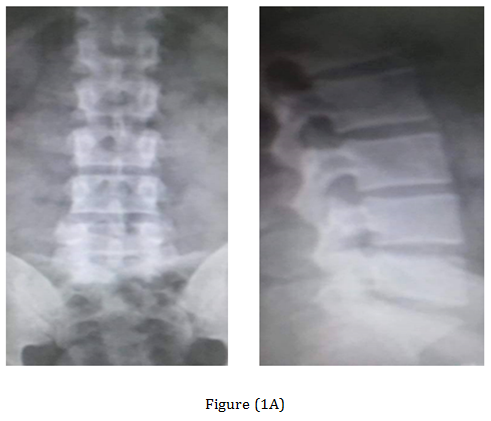
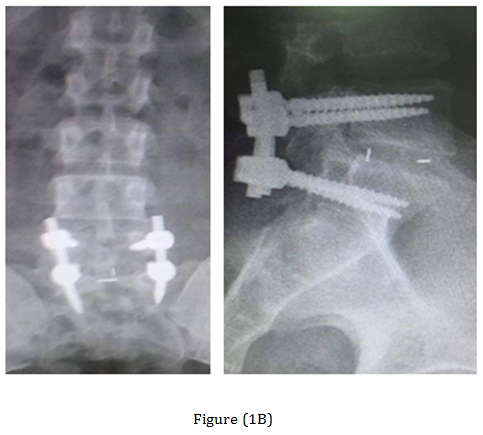

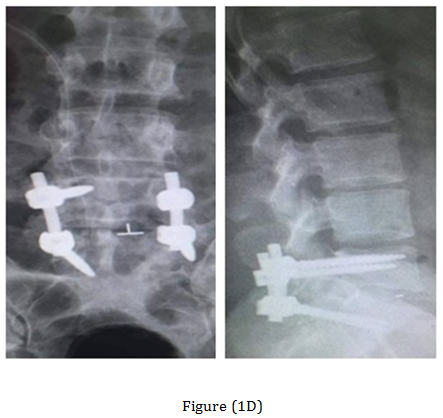
Figure 1 Case 3 with L.D.P L5-S1. (A) Preoperative radiograph anteroposterior and lateral views. (B) Preoperative MRI. (C) Post-operative radiographs anteroposterior and lateral views. (D) At the 18-months follow up anteroposterior and lateral views radiograph.
|
VAS |
Paired t-Test |
|||
|
Range |
Mean ± SD |
T |
p-value |
|
|
Preoperative |
4.0 - 9.0 |
6.9 ± 1.831 |
13.530 |
0.000 |
|
After 24 months |
0.0 - 1.0 |
0.08 ± 0.288 |
||
Table 1 Comparison between VAS preoperative and after 24 months postoperative.
|
|
ODI |
Paired t-Test |
||
|
Range |
Mean ± SD |
T |
p-value |
|
|
Preoperative |
22 - 38 |
32.9 ± 4.981 |
18.651 |
0.000 |
|
After 24 months |
1 - 5 |
2.33 ± 1.302 |
||
Table 2 Comparison between ODI preoperative and after 24 months postoperative.
Degenerative lumbar spine disordersare the commonest causes of low back pain. Lumbar arthrodesis contributed in solving this issue. TLIF is one of the modern techniques of lumbar arthrodesis which showed effective role in treating of lumbar pain caused by degenerative lumbar disc disorders.10 Clinical presentations in our study were mechanical back pain in 100% of cases and leg pain in 90% of cases. Female to male ratio was 1:4. Indications of TLIF includes low grade spondylolisthesis, degenerative disc diseases, spinal stenosis, unilateral and recurrent disc herniation especially if lumbar fusion is needed in addition to posterior decompression.11 Humphreys made a comparative study of 34 PLIF with 40 TLIF cases.12 Of the 34 PLIF procedures, 13 were single level, 20 were double level and 1 was triple level. Of the 40 TLIF, 17 were single and 23 were double level. There were no complications with the TLIF patients. However, with the PLIF, there were 4 cases of radiculitis, 1 case of broken hardware, 1 case of screw loosening, 2 cases of screw removal, 1 nonunion requiring additional fusion, and 1 superficial wound infection. The authors concluded that the TLIF showed to be a good alternative to PLIF with relatively less risk of complications, less operating time and hospitalization, as well as significant reduction in blood loss during operation. We quite agree with this as regard our results only but we did not have any comparison with PLIF to guarantee the final conclusion described by Humphry et al.12 TLIF approach lessens the potential for nerve root injury, therefore resolving probably the most important limitation of the PLIF procedure. For this reason, and the case specific advantages of TLIF over a combined anterior and posterior single-level fusion, we favor TLIF over PLIF as the choice surgical procedure for the posterior operative management of symptomatic degenerative lumbar disc disease. Lowe and Tahermia reported in their study which was done on 40 patients underwent TLIF surgery that fusion rate radiologically was 95% of cases and good to excellent clinical outcome was achieved in 88% of cases.13 In our study fusion rate was 90% and improvement in clinical symptoms was 90% of cases.
Deng-Lu Yan et al.11 mentioned that in his study lumbar pain improved in 83.5% of patients compared to 90% lumbar pain improvement in our.11 Complications in our study occurred in the form of dural tear in 2 cases (10%) that were repaired intra-operatively, early post-operative wound infection reported in one case (5%) and resolved completely after 2 weeks of medical treatment, neurological deficit reported in one case (5%) in the form of weak dorsiflexion of right ankle with hypoesthesia on the lateral aspect of the same foot and were resolved completely after medical treatment and physiotherapy, cage subsidence reported in one case (5%) due to extensive resection of the end plate although the patient clinically didn't complain, Pseudo arthrosis reported in 2 cases (10%) and poor improvement of low back pain also reported in 2 cases (10%).
In conclusion, it is our opinion that TLIF is a technique which offers a simple, safe and effective treatment for degenerative lumbar disc diseases with great improvement of life quality of cases with surgery satisfaction.
None.
None.

©2017 Alsebaey, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.