MOJ
eISSN: 2374-6939


Research Article Volume 12 Issue 4
1Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof, Russian Ilizarov Scientific Centre, Russia
2Professor, Bari-Ilizarov Orthopaedic Centre, Bangladesh
3Medical officer, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Mofakhkharul Bari, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Professor, Russian Ilizarov Scientific Centre, Kurgan, Bari-Ilizarov Orthopaedic Centre, 1/1, Block#E, Suvastu Shirazi Square, Lalmatia, Dhaka-1207, Bangladesh, Tel +88 01819 211595
Received: June 29, 2020 | Published: July 14, 2020
Citation: Bari MM, Shahidul I, Shayan BAMR. Tibialization of fibula for reconstruction of big tibial defects (post-traumatic, post-infective) by Ilizarov technique. MOJ Orthop Rheumatol. 2020;12(4):73-78. DOI: 10.15406/mojor.2020.12.00522
Purpose: The purpose of this study was to evaluate the functional results of Tibialization of fibula for reconstruction of big tibial defects.
Methods: Between January 2000 and January 2018, 28 patients (20 males and 8 females) with big defects following infection and post traumatic injury of the tibia were treated. The mean age of the patients at the time of surgery was 15.3 years (4-24 years). The fibula was mobilized medially to fill the defect and was fixed with Ilizarov fixator. The average size of the defects reconstructed was 7.35 cm (6-10cm). Patients were evaluated functionally using the ASAMI scoring system.
Results: The mean follow-up period was 29.03 months (range, 15-60). The average time for complete union was 6.8 months (range, 5-9 months). At final follow-up all patients had fully united. We found leg length discrepancy in 22 patients and that was corrected by re-lengthening of the solid new regenerate bone.
Conclusion: Ipsilateral fibular centralization or medialization is an excellent reconstruction for big tibial defects after wide debridement with very good acceptable functional outcome. Absolute stable osteosynthesis by biocompatible thin wires with Ilizarov fixation is the key to union and success.
Keywords: tibial defects, excision of the infected wound, reconstruction, Ilizarov, fibular medialization
Reconstruction of large defect of tibia following infection is considered as one of the most difficult problem facing the orthopaedic surgeon.1–4 Amputation with modern prosthetic fitting is a salvage procedure to treat big defects, which gives a functional result with unpredictable psychological impact.
The tibio-fibular synostosis in managing tibial short defect using the Ilizarov external fixator was applied in 28 patients aged from 4-24 years. 20 patients suffered from paediatric haematogenus osteomyelities and in 8 cases tibial defect developed after multiple sequestrectomies, necrectomies performed for chronic osteomyelitis of traumatological origin. Different modalities have been used to reconstruct the segmental defects following infection.5–10 Autogenous cortical bone graft is one of the commonly used methods for reconstruction where necrosis of the majority of osteocytes has occurred and required replacement of the dead bone by creeping substitution.5,11,12 Other methods of reconstruction include autoclaved autogenous bone graft13 and allograft14 commonly associated with nonunion and or infection.15 Vascularized fibular graft has been used with great success in the reconstruction of segmental tibial defects, but it is an extensive and time-consuming procedure.11,16
The use of fibular centralization (fibula pro tibia) was used as early as 1940 by Wilson17 to reconstruct a congenital tibial defect, and since that time it is used to reconstruct post-traumatic and post-infective tibial defects.12,18 This technique encourages many surgeons to reconstruct as a one-stage19,20 or two-stage21 procedure with a high success rate.
The purpose of this prospective study was to evaluate the results of ipsilateral fibular centralization as a single stage reconstructive procedure to reconstruct the skeletal defect following wide excision of tibia (post-traumatic and post infective).
Between Jan 2000 and Jan 2018, 28 patients (20 males & 8 females) with big defects following infection and post-traumatic defects of the tibia were treated by fibular medialization.1–4 Their medical records, imaging, and functional status were reviewed. All 28 patients had undergone preoperative assessment.
The primary goal of surgery was to preserve the limb. The defect was reconstructed by the use of ipsilateral fibular graft.
Operative technique
Operative intervention for filling in tibial defects using fibula includes the following:
For the sake of increasing the stability of the bone fragments during fixation period the system “apparatus-limb” is replaced depending on specific biological conditions to provide regeneration of tissues. The choice of an osteotomy type of fibula or synostosis is very important. The character of fibular osteotomy is determined depending on peculiarities of the pathology and variant of synostosis. Techniques of fibular osteotomies could be as follows:
Minimal traumatization of soft tissues is an e obligatory condition of surgical intervention. This can be achieved by:
A variety of operative interventions is osteoclasis which is performed in a close way. Osteoclasis serves for obtaining fiexion and torsion fracture of a bone or a fragment.
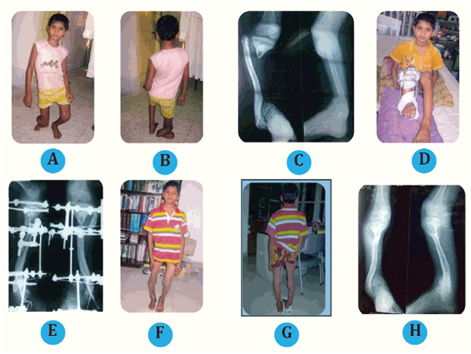
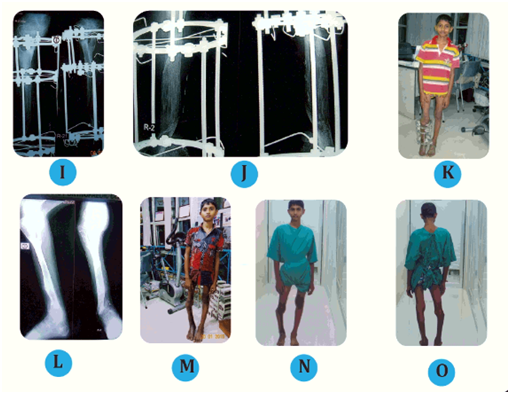
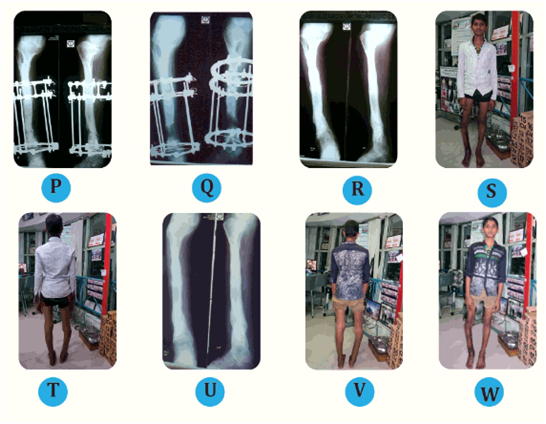
Figure 1
Post-operative care
The principally new mechanical and biological basis of the techniques developed for tibio-fibular synostosis makes a fine distinction of the proposed methods for treating tibial defects from conventional techniques of tibio-fibular synostosis. Post-operative course of the patients with tibial defects and application of tibial-fibular synostosis went on regularly without significant somatic changes. In the patients with fibular tibialization techniques applied (30%) body temperature within the first seven-ten days varied from 37.2°to 37.8° and got normalized within three-five days. Within first three-five days general body temperature did not exceed 38.0° and varied from 37.2° to 38.0°. The patients had no pronounced edema of distal parts of operated limb. Since post-op wounds were small and two to five silk sutures were applied to the wound these sutures had been removed on 5th-7th day.
Functional weight-bearing on the limb was permitted on the next day after osteosynthesis but with the loading within 50% for a period of fragment transport and fully for fragments fixation period. In fibular tibialization osteotomized fragments transport was started on the 5th day by 0,25mm three-four times a day up to the contact with tibial fragments. In all the cases of tibio-fibular synostosis during frame control period in the first place it is necessary to achieve the contact of osteotomized fibular fragments with the tibial ones and at the same time accompanying segment deformities as well as stable deformities or contractures of the adjacent joints are to be eliminated and only at the final stage anatomical tibial shortening is compensated using tibial lengthening. After above and tibial fragments transport the modules of rigidity as well as of firm bone stabilization have been assembled with the frame using additional wires and tension of uniting parts subject to constant compression contact (Table 1).
|
Case No |
Age (Years) |
Sex |
Diagnosis |
Recection length(cm) |
Follow-up (months) |
Hardware |
Complication |
Union (months) |
Functional scoring |
|
1 |
20 |
M |
Post-traumatic |
6 |
17 |
Ilizarov Application |
LLD |
6 |
Good |
|
2 |
5 |
M |
Post-osteomylitic |
8 |
55 |
Ilizarov Application |
LLD |
9 |
Excellent |
|
3 |
16 |
M |
Post-infective |
9 |
15 |
Ilizarov Application |
LLD |
7 |
Excellent |
|
4 |
10 |
F |
Post-traumatic |
6 |
19 |
Ilizarov Application |
LLD |
6 |
Excellent |
|
5 |
7 |
M |
Post-osteomylitic |
8 |
12 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
6 |
24 |
M |
Post-infective |
7 |
14 |
Ilizarov Application |
LLD |
5 |
Good |
|
7 |
23 |
F |
Post-traumatic |
7 |
52 |
Ilizarov Application |
LLD |
9 |
Excellent |
|
8 |
14 |
F |
Post-osteomylitic |
5 |
45 |
Ilizarov Application |
LLD |
9 |
Excellent |
|
9 |
18 |
M |
Post-traumatic |
6 |
33 |
Ilizarov Application |
5 |
Excellent |
|
|
10 |
23 |
M |
Post-infective |
9 |
26 |
Ilizarov Application |
LLD |
5 |
Excellent |
|
11 |
19 |
M |
Post-traumatic |
8 |
17 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
12 |
24 |
M |
Post-osteomylitic |
8 |
38 |
Ilizarov Application |
LLD |
6 |
Good |
|
13 |
15 |
F |
Post-infective |
9 |
35 |
Ilizarov Application |
6 |
Excellent |
|
|
14 |
12 |
M |
Post-traumatic |
7 |
43 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
15 |
10 |
F |
Post-osteomylitic |
6 |
46 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
16 |
6 |
M |
Post-traumatic |
9 |
22 |
Ilizarov Application |
LLD |
7 |
Excellent |
|
17 |
18 |
M |
Post-osteomylitic |
8 |
38 |
Ilizarov Application |
5 |
Excellent |
|
|
18 |
16 |
M |
Post-infective |
5 |
25 |
Ilizarov Application |
LLD |
6 |
Good |
|
19 |
17 |
F |
Post-traumatic |
7 |
28 |
Ilizarov Application |
9 |
Good |
|
|
20 |
19 |
F |
Post-infective |
9 |
26 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
21 |
11 |
M |
Past-traumatic |
6 |
16 |
Ilizarov Application |
LLD |
7 |
Excellent |
|
22 |
22 |
M |
Post-osteomylitic |
8 |
18 |
Ilizarov Application |
5 |
Excellent |
|
|
23 |
20 |
M |
Post-infective |
9 |
19 |
Ilizarov Application |
LLD |
6 |
Excellent |
|
24 |
19 |
F |
Post-traumatic |
9 |
24 |
Ilizarov Application |
LLD |
9 |
Excellent |
|
25 |
15 |
M |
Post-osteomylitic |
5 |
21 |
Ilizarov Application |
LLD |
8 |
Excellent |
|
26 |
6 |
F |
Post-infective |
6 |
32 |
Ilizarov Application |
8 |
Excellent |
|
|
27 |
19 |
M |
Post-osteomylitic |
7 |
54 |
Ilizarov Application |
LLD |
5 |
Excellent |
|
28 |
12 |
M |
Post-infective |
9 |
23 |
Ilizarov Application |
LLD |
7 |
Excellent |
Table 1 Patients demographics
LLD: limb length discrepancy
The rates of fragments transport as well as tibial distraction during lengthening are to be delayed or to be temporarily (for two-three days) stopped if clinical and subjective manifestations of nerve vascular bundle irritation or peroneal neuritis are observed. Radio-graphic dynamics of regenerate formation after synostosis was examined in all patient. Fibular tibialization with cylindrical fragment in all 28 patients with tibial defect took place in different time depending on the condition of skin scars subjected to tension. The fragment was transported from fibula with moderate tenderness. In four patients of this group in post-op fragment transport the signs of peroneal neuritis were observed but they disappeared during fragments fixation. In two weeks after initiation of fibular transport in the X-rays light cloudy shadows of the regenerate getting dense and oriented to the traction direction were observed from the side of osteotomized ends. Post-operative period in six patients after closed osteosynthesis for tibialization with proximal fibular end went on smoothly without marked increase of the body temperature. As a rule, distraction started from the third day after surgery. The rate was individual and depended on the intensity of tibial pains appearing in fibular transport. Commonly it was 0,25 mm twice or three times a day. Fibular transport up to the level of proximal tibial fragment was performed daily with simultaneous rotation of distal tibia by one degree per day in medial rotation position.
The mean total operative time was 1 and ½ hours and the mean blood loss was 200mL (range, 200-300mL). The mean duration of follow-up was 25.5 months (range, 15-48 months). All cases were assessed as regard clinical evaluation, radiological union, functional outcome. We achieved union in all cases. The average time for complete union was 5.5months (range, 5-8). Early callus formation was seen at 6 weeks post-operatively between the transposed fibula and remaining part of the fibula due to intact periosteal sleeve, which strengthens the reconstruction. All patients walked independently without a brace and without pain but with a little limp, which was evident in most of the cases. Hypertrophy of the graft was seen and increased with time.
Functional outcome was assessed by the ASAMI criteria, which assesses six parameters: pain, functional activity, emotional acceptance, use of external supports, walking distance and gait. The score was better in cases with intercalary reconstruction where joint mobility was preserved compared with knee or ankle fusion. Three had superficial wound infection and were treated by repeated dressing and parenteral antibiotics. 22 cases had LLD (Limb Length Discrepancy): 20 of them had LLD (Limb Length Discrepancy) of less than 5 cm and two patients had a discrepancy of more than 9cm. These occurred in skeletally immature patients and they were scheduled for limb lengthening by llizarov technique and we did that in all cases.
Reconstruction of large defects after trauma or infection is a challenging problem for orthopaedic and reconstructive surgeon. Reconstruction of a tibial defect can be done by different methods including large segmental allograft, vascularized and non-vascularized autograft, bone transport and mega prosthesis.7–10,20
Reconstruction by Strut allograft depends on their availability and amount of bone resection with potential nonunion and infection. The use of bone transport by distraction osteogenesis requires a lengthy procedure which limits its use in reconstruction of defects with big gap.21 Use of endoprosthesis for reconstruction of a proximal tibial defect gives an excellent functional result,5 with time it deteriorates due to loosening and there is a high rate of deep infection.8,22,23
Non vascularized autogenous fibular graft can be used to reconstruct post-traumatic tibial defect a 92% union rate by Ilizarov technique and hypertrophy of the graft is increased with time. Introducing the microvascular techniques, vascularized fibular graft can be used to reconstruct the tibial defect11,16 but it is an extensive and time-consuming procedure, which requires harvesting a fibular graft from a contralateral side and required special skills, but it is significantly stronger than a conventional neovascularized graft. We have done fibular osteotomy as described by Prof. Ilizarov. He described subperiosteal fibular osteotomy with maintenance of the lateral part of the periosteum as a continuous sheet above and below the osteotomy; he believed that this leads to a better union between the transposed fibula and the remaining part of the fibula, with a better strength of the reconstructed part. This technique is different from that done by Puri et al.20
Nonunion is a major issue if no or even minimal internal fixation is used according to Hatori et al.21 This why Ilizarov recommends fixation by biocompatible thin olive and smooth wires which is better than internal fixations. We feel that in order to achieve union, stable fixation of the transposed fibular graft should be achieved, which is not an easy.10,13 We achieved union in all cases, with average time for complete union of 5.5 months.
We allowed full weight bearing after the application of Ilizarov apparatus and we can see hypertrophy of the graft later on, which indicates that the graft achieved its biological potential. No stress fracture is seen in our series due to Ilizarov technique. LLD (Limb Length Discrepancy) was an inevitable complication, especially in skeletally immature patients with resection of the proximal or distal epiphyseal plate and limited mobilization of the fibular graft either proximally or distally in proximal or distal defects respectively. The infection rate in our study was 2%, which is significantly lower than that of the prosthetic replacement, which may reach up to 50%.22,23 We overcome all the disadvantages.
We had knee and ankle modality and shortening that caused limping; however, the Ilizarov technique had great advantages of preserving the patient's limb, with better psychological aspect, and it is a rapid, inexpensive procedure with high rate of union and graft hypertrophy without the need for microvascular skills.
In conclusion, reconstruction of a large tibial defect following (post traumatic, post infective) by transferred fibular graft and fixation by Ilizarov technique is an excellent option with an acceptable functional outcome; stable Ilizarov fixation is the key for union and success.
None.
The authors declare that they have no conflict of interest. All authors clearly stated that no benefits had received for this study.
There is no funding source.

©2020 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.