MOJ
eISSN: 2374-6939


Research Article Volume 3 Issue 1
1Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Russia
2Bari-llizarov Orthoapedic Centre, Russia
3National Institute of Traumatology and Orthopaedic Rehabilitation, Bangladesh
Correspondence: Mofakhkharul Bari, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Professor, Russian Ilizarov Scientific Centre, Kurgan, Tel +88 01819 211595
Received: April 23, 2015 | Published: June 29, 2015
Citation: Bari MM, Islam S, Shetu NH, et al. The management of bone loss of diaphyseal tibial long bones. MOJ Orthop Rheumatol. 2015;3(1):244-246. DOI: 10.15406/mojor.2015.03.00080
The management of segmental defects within the diaphysis of long bones is one of the most challenging problems that the surgeon confronts in his practice. The procedures traditionally used to bridge bone gaps include autogenous bone grafting,1 posterolateral bone grafting,2 transplantation of allograft bone & tibialization of fibula procedures.3,4 All the above traditional methods of management of bone defects sometimes require multiple surgical interventions. The treatment period is long & weight bearing may not be possible while the functional results are often less than satisfactory. Recent studies showed that the G.A. llizarov Technique is a more popular than vascularised bone grafts especially for big bone defects.5
The ilizarov technique
The llizarov circular external fixator was designed in early 1950s.6 It is a modular device allowing controlled mechanical forces (compression & distraction) to be applies at a pathological bone site. The system uses biocompatible thin wires that are placed in different planes & are secured to modular rings under tension. These thin wires act as a small spring within a more rigid system of rings & concerning rods. In this way the system provides stability against angular, rotational & translational displacements, while it is relatively flexible in axial direction, allowing controlled axial loads to be applied at the zone of osteogenesis.7 McCoy MT et al.8 have compared the mechanical properties of four different external devices. They demonstrated that the llizarov external fixator had the lowest overall stiffness but high resistance to bending & rotation strains. It provides a dynamic osteosynthesis system, which prevents harmful (bending, translational & rotational) forces & allows only the useful (axial) forces to act at the osteogenesis site. This probably stimulates bone regeneration. In addition, llizarov apparatus allows multiplanar & multidirectional correction of deformities". G.A. llizarov using his apparatus, developed new methods for salvage & reconstruction of a variety of a serious congenital & acquired orthopaedic problems such as clubfoot, radial clubhand, hand & leg length discrepancies, infected & non-infected non-unions, mal-unions, segmental bone defects, chronic osteomyelitis & joint contractures.
Biology of osteogenesis by ilizarov technique
The llizarov methods basically consist of application of mechanical forces to induce new bone formation. This can be accomplished by two separate biological processes: distraction osteogenesis & osteogenesis by changing the mechanical environment at a pathological bony site. Distraction osteogenesis is the method of lengthening a long bone without grafting. After a diaphyseal corticotomy, the early mesenchymal in growth (early callus), is elongated by gradual, progressive distraction using a dynamic external fixator.9 Corticotomy is a low energy osteotomy in which only the cortex is being cut. In this way the endosteum within the medullary canal, along with the medullary vessels are preserved. Gradual distraction of the corticotomy site organizes the early callus into a cylinder of parallel fibers of collagen. The fibers are generally oriented longitudinally parallel to the tensile force, joining the distracted corticotomy surfaces & filling the gap created by distraction. Gradually as the distraction proceeds these fibers begin to ossify. As long as distraction is continuing a central region (the interzone), consisting histologically of undifferentiated cells, does not undergo ossification, allowing for the lengthening to continue.
Ossification is carried out from both corticotomy surfaces towards the central interzone & extends through the entire cross section of the newly formed tissue. When the desire lengthening is obtained the distraction is stopped & the interzone ossifies. Later, under the compression forces, applied by muscle contraction & weight loading the newly formed cylinder of solid bone remodels into cortex & medullary canal. The remodelling process may require years to produce mature, lamellar cortical bone. Osteogenesis may be achieved by changing the mechanical environment to stimulate a pathologic bony interface (e.g. non-union) & restore bony continuity. By this technique variations of compressions & distraction forces across a non-union or a pseudoarthrotic site are applied to induce osteogenesis. The sequence of compression-distraction depends on the rigidity and compression of the pathologic bony interface. There are many critical factors related to osteogenesis. The local blood supply and the integrity of the periosteum are of great importance. llizarov emphasized the importance of careful corticotomy to prevent damage to the periosteum & to the medullary vessels. Recent experimental as well as clinical studies however, have demonstrated that dissection of the nutrient vessels during the corticotomy, plays no significant role because the local vascularity is rapidly restored. The intregrity of the periosteum is the most important factor for new bone formation.
Another factor promoting the bone formation is the stable fixation of the bone fragments, so that the forces applied at the osteogenic zone are controlled both in their magnitude & their orientation. Another critical mechanical factor is the rate & the rhythm of distraction. Llizarov found experimentally, that distraction at a rate of 0.25 mm every 6 hours (1mm/day) is ideal. Distraction at a faster rate causes local ischaemia & subsequently retardation of osteogenesis of poor quality of the newly formed bone.9–12 Distraction at a slower rate will cause premature consolidation of the interzone, preventing further distraction. The last important factor is the level of the corticotomy.10 It seems that the ideal place for the corticotomy is at the metaphyseal region. Metaphyseal corticotomy must be preferred whenever possible. Weight bearing is considered to be essential both for bone regeneration & consolidation. We used the above biological processes of distraction in our practice.
For the last 23years (1990-2013) in different hospitals, 126 cases of tibial diaphyseal defects were operated on by the llizarov method. Male predominated with an average age of 35 years (Table 1). The age of the patients ranged between 12-58years (average 35). The main aetiology was open fractures as presented on Table 2 patients had active infections with drainage & seven were previously infected. The majority of the patients had undergone several previous operations including compression plating, external fixation, bone grafting & plastic operations. Many patients had shortening & angular or rotational deformity. The average duration of the bone defects was 10 months. After resection of the infected & necrotic bone the intercalate defect was 4.8cm in average (range 3.5-8.5cm).
|
Male (87.30 %) |
110 |
|
Female (13.70 %) |
16 |
Table 1 Tibial diaphyseal defects operated by the llizarov method
|
Aetiology |
|
|
Open Fractures |
86 cases |
|
Complications of Surgically Treated Fractures |
15 cases |
|
Osteomyelitis |
12 cases |
|
Gun Shots |
10 cases |
|
Congenital Pseudoarthrosis |
03 cases |
|
Total |
126 cases |
Table 2 Aetiology of open fractures
A proximal corticotomy & gradual transportation of a bony fragment towards the fragment opposite to the segmental defect (the target zone) was performed. Using the llizarov device the bone fragments, proximal & distal to the intercalate defect, were fixed in good alignment. A bone fragment of adequate length was then created after the corticotomy. 5 to 7 days after corticotomy, the bony fragment was gradually transported axially across the defect. The transportation was achieved by the use of olive wires & inclined rods, or by transporting central ring connected to the bone fragment with two or more wires. As the bone segment was transported, a new gap was created behind it, while the length of the original gap was gradually reduced & finally when the leading edge of the transported bone reached the bone surface opposite the segmental defect, it was closed. The new gap, created behind the transported bone, was regenerated by distraction osteogenesis. At the target zone variations of compression-distraction forces were applied to induce osteogenesis. When the local circumstances allowed, two bone fragments, one proximally & one distally to the defect, were transported towards the centre. By this bifocal transportation the filling of the gap was accelerated.
Regeneration of the distraction gap was achieved in all 126 patients. Union at the target zone was achieved in 120 patients out of 126 cases & union was not related to the length of the bony defect. In six patients there was a failure of union at the target zone. This was due to incomplete removal of the eburnated & atrophic bones. Healing of the infection occured in all patients without a second operation. Residual varus deformity remained in two patients with 10 & 12 degrees deformity respectively (Figure 1 & 2).
Case 1: Figure 1.
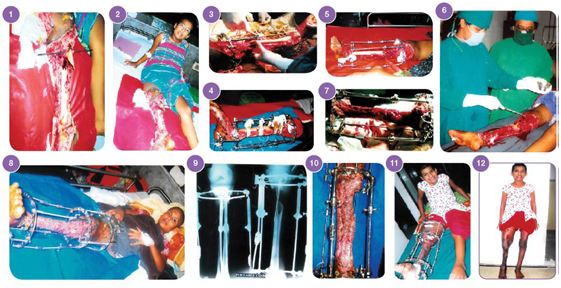
Figure 1: Case 1.
1.Open degloving injury of left leg with bone loss of left tibia GIIIB.
2. Radiograph of left tibia fibula with bone loss in the lower tibia.
3. Close up view of the left leg with llizarov in situ.
4. Ilizarov in the left leg after 1 month follow up.
5. Close up view of the left leg with llizarov in situ. 6. Skin grafting was done.
7. After 2 month follow up.
8. Radiograph of right tibia fibula with distraction osteogenesis.
9. After 3 months follow up.
10. Radiograph of left tibia fibula with good regenerate in the upper tibia.
11. After 4 months follow up, patient is in standing position.
12. After 4 1/2 months follow up. Front view.
13. After 4 1/2 months follow up. Back view.
14, 15. After 6 months follow up.
16. In OR Table before removal of llizarov apparatus.
17. Radiographic final result after 7 months.
18. Clinical appearance of the patient with smiling face.
Case 2: Figure 2.

Figure 2: Case 2.
Pain at the site of the wires was a frequent problem during transportation of the intercalated segment. The most common complication was pin track infection & it was treated by local care & in 2 cases it was necessary to replace the wires. There was no incidence of pin track osteomyelitis. Oedema of the leg & foot was always present during bone transportation. Joint stiffness of the knee & ankle occured very often during bone transportation, but after the removal of the fixator the rehabilitation of these joints resulted to the full recovery of joint motion. There was no incidence of neurovascular complications. Psycological intolerence was seen in four young patients. They required moral support until the end of the treatment.
llizarov method for the treatment of pseudoarthrosis & segmental bone defects has many advantages.12,13 But several technical problems may arise if the details of the technique are not followed precisely. Very important thing is to excise all the infected & necrotic tissues. The inexperienced surgeons usually fail to carry out a sufficient radical debridement with the current experimental & clinical experience, it is evident that regeneration of bone at the site of distraction can be obtained safely. It was evident in our cases that wide debridement accelerated healing & helped to control infection. For successful bone transportation, it is also important to maintain the bone ends in good & stable position. In order to provide firm stability & to avoid axial deviation during distraction, the assembly of fixator in our cases usually required one or two rings proximally, 1 in the intercalate segment & 1 or 2 distally. Another important factor is to achieve good contact of the bones, when the transported fragment contacts the bone surface at the target zone (opposite the segmental defect). A partial contact in 6 of our cases was the cause of non-union. The importance of controlling precisely the movements of the transporting bone fragment has been emphasised by many authors.5-7,10,13
The llizarov techniques for the treatment of segmental defects of diaphyseal long bones are effective & offer many advantages. One of the greater advantages of this technique is that it allows for the simultaneous treatment of bone loss, infection, non-union, deformity & problems of the soft tissues at the same time. In our all cases complications were not severe & did not affect the results.
None.
The authors declare there is no conflict of interest.

©2015 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.