MOJ
eISSN: 2374-6939


Research Article Volume 13 Issue 1
Department of Orthopedic Surgery, University of Toledo Medical Center, United States
Correspondence:
Received: January 02, 2021 | Published: January 26, 2021
Citation: Liu J, Roebke LJ, Maten JWV, et al. Surgical treatments of patients with periprosthetic humeral fracture and comorbidities. MOJ Orthop Rheumatol. 2021;13(1):1-4. DOI: 10.15406/mojor.2021.13.00537
Background: Periprosthetic humeral fractures represent a complex and rare complication. Currently, there is no standardized procedure for management or classification of these fractures.
Questions/purposes: This unique case series purpose was to look at surgical outcomes and comorbidity profiles of 10 PHF patients. Subsequent analysis looked at whether these outcomes could add to the discussion of a proposed standard of care in a patient cohort with significant comorbidities.
Patients and methods: All patients with humeral fractures from 2008-2019 were analyzed for inclusion. A total of ten patients met the inclusion criteria; humeral fracture concurrent with a shoulder arthroplasty. Each patient was managed surgically using a locking plate with or without cerclage wiring. Outcome analysis was then performed for each patient. Humoral fractures managed conservatively were removed from the dataset along with periprosthetic fractures around an elbow arthroplasty, IM nail, or supracondylar fracture after shoulder arthroplasty.
Results: The average union time in all patients was 13.27±2.90 (9.86-17.29) weeks. There was no significant difference between patients treated with cerclage wiring or without. All patients had successful union except for a patient with Osteogenesis Imperfecta. There were two radial nerve palsies. The average Deyo-Charlson score and BMI was 7.1±.84 (4-13) and 29.89 respectively.
Conclusion: The treatment of PHFs using the technique of ORIF with locking plate with or without cerclage wiring provides satisfactory outcomes in a patient population that usually includes significant comorbidities.
Level of evidence: Therapeutic Study Level IV Retrospective Review.
Keywords: periprosthetic humeral fracture, comorbidities, deyo-charlson score, ORIF
Currently, there are very few papers analyzing periprosthetic humeral fractures (PHFs) in comparison to the widely researched topic of periprosthetic femoral fractures. PHFs are a rare complication that can happen either intraoperatively or postoperatively; the prevalence can range as a high as 3% to as low as 0.6%.1–5 Although these complications are rare, the volume that surgeons may see is on the rise. There is an increasing rate of shoulder and elbow arthroplasties performed in the United States. Between the years of 1993 to 2007 alone, the annual procedure rates jumped from 6% to 13%.6 As such, rates of periprosthetic humeral fractures will also continue to rise in the US.
Unlike the more well-defined treatment and classification protocol for femoral periprosthetic fractures, PHFs do not have an well-established consensus.4,5,7–9 Most current classification systems are constructed to reflect the location of the fracture compared to the tip of the prosthesis: proximal, adjacent, or distal. The Wright and Cofield classification system was applied to this case series due to the clarity of parameters: type A is proximal to tip of prosthesis, type B is adjacent to the tip of the prosthesis, and type C is distal to the tip of the prosthesis.5
In this study, an analysis of comorbidities was done using the Deyo-Charlson Index and patient BMI. BMI together with the Deyo-Charlson Index helps create a patient profile for the typical patient who may suffer a PHF. Singh et. al.10 is the only study to utilize the Deyo-Charlson Index in conjunction with PHFs with data collection of patients from 1976 to 2008. In the Singh et al study, the Deyo-Charlson index was associated with a significant increase in risk of postoperative PHF; however, it does not list the individual Deyo-Charlson index in addition to BMI for each patient case with the corresponding treatment in each patient. Additionally, corresponding union time after treatment of these complex patients and complications are not reported. Our study provides this information with the goal of enhancing the body of knowledge of what the standard of care PHFs should be. The purpose of this study is to investigate a level 1 trauma center’s experience on surgical management of PHFs while also analyzing patient comorbidities. This case series examines patient characteristics, previous arthroplasty, treatment, union time, and any complications that may have occurred.
A retrospective review was conducted between January 01, 2008 and May 31, 2019, patients who had a surgically repaired humeral fracture were analyzed for potential periprosthetic humeral fractures. Of the 877 humeral procedures performed, 15 periprosthetic humeral fractures were identified. PHFs around an elbow arthroplasty, IM nail, or a supracondylar fracture after shoulder arthroplasty were all discarded from the data set. Patients with conservative management alone were also excluded. Following final inclusion criteria, radiological analysis and chart review were both completed. In total, nine PHFs and one stress riser were included for final analysis.
A thorough chart review was also performed to collect patient demographic and comorbidity data. The Deyo-Charlson score and BMI were then used to evaluate the patient profile of PHFs following shoulder arthroplasty. All data was collected in and analyzed using Microsoft Excel.
The patient population consisted of nine female patients and one male patient. The average age was 75.1±12.71 (55-92) years old. The average union time in all patients was 13.27±2.90 (9.86-17.29) weeks. In comparison, patients with cerclage wiring had union time average of 13.81±2.81 (9.86-17.29) weeks while patients without cerclage wiring had union time of 11.35±1.22 (10.14-12.57) weeks. A surgical approach was used in all patients. All fractures resulted in satisfactory union apart from the intrahumeral stress riser case which was complicated by osteogenesis imperfecta.
Fracture types consisted of five Type B, four Type C, and one intrahumeral stress riser according to the Wright and Cofield classification system. Three patients had a prior reverse total shoulder and within this group, two patients had a type C PHF and one patient had a type B PHF. Five patients had hemiarthroplasty and within this group, one patient had an intrahumeral stress riser, three patients had a type B, and one patient had a type C. The one patient with long stem hemiarthroplasty (Case 5) had a type C fracture. The patient with a total shoulder arthroplasty had a type B fracture. All fractures resulted from a fall from various heights.
The Deyo-Charlson score was on average 7.1±.84.4–13 A score of 7, 13, 4, 6, 8, 10, 5, 6, 6, and 6 were included for all ten cases of PHFs respectively. A large portion of the patient cohort had significant conditions that may have affected healing due to compromised bone quality. Rheumatologically, five patients had osteoporosis (case 6, 7, 8, 9, 10), two patients had rheumatoid arthritis (case 2 and 5), and four patients had osteoarthritis (case 1, 3, 6, 7). These surgically managed patients included seven patients treated with open reduction internal fixatin (ORIF) with locking plates and cerclage wiring, while three patients were treated with ORIF with locking with no use of cerclage wiring (Figure 1). Conservative treatment was attempted prior to surgical management in case 1, 2, and 3 but was unsuccessful. Bone grafts were used in cases 1, 2, 3, 7, 8, and 10.
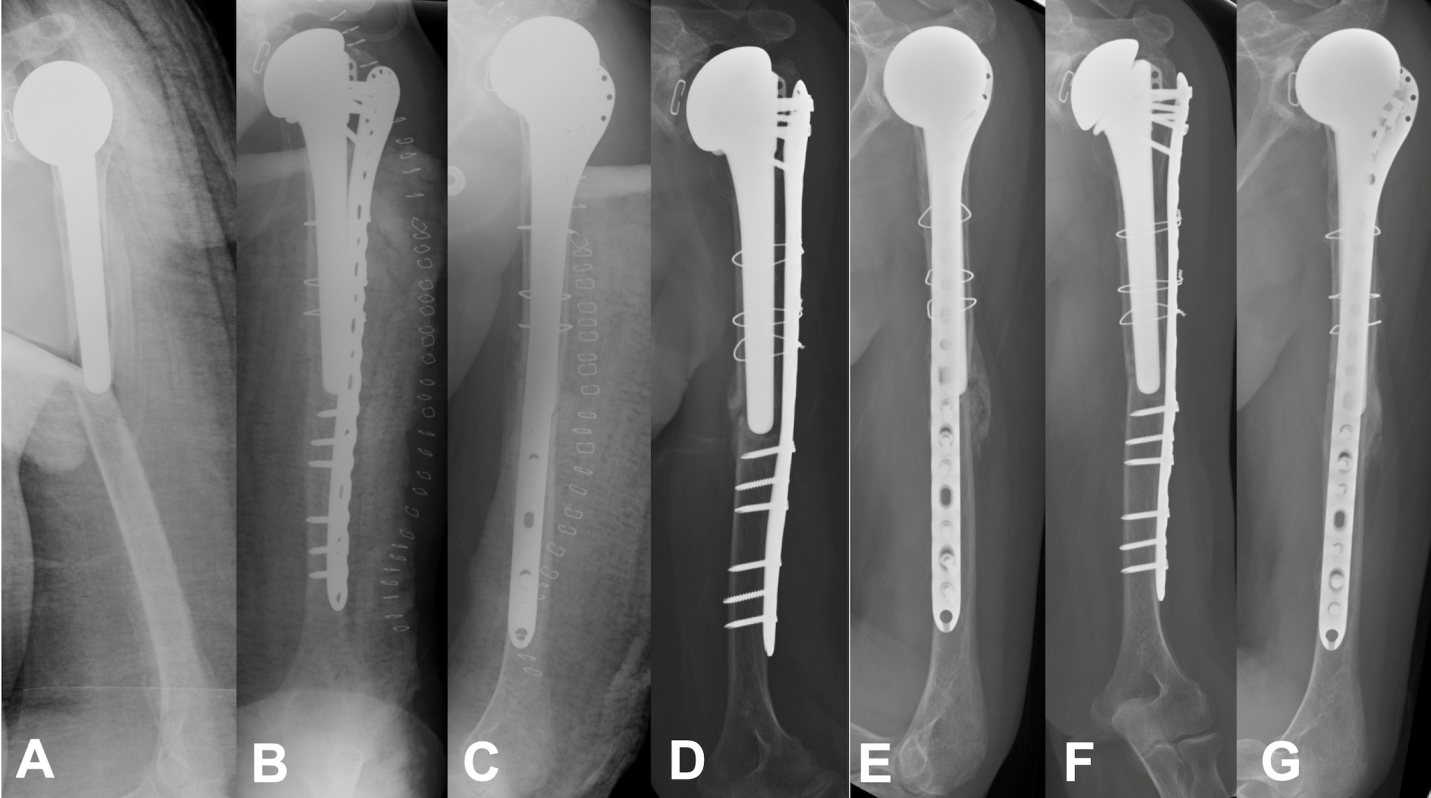
Figure 1 Seventy-one-year-old female with a previous left shoulder hemiarthroplasty previously and a periprosthetic humeral fracture after falling to the ground.
A: Preoperative lateral view; B: Postoperative AP view; C: Postoperative lateral view; D: Postoperative 2.5 months AP view; E: Postoperative 2.5 months lateral view; F: Postoperative 6 months AP view; G: Postoperative 6 months lateral view.
The range of motion was provided in two patients. Fifteen days post-operation, case 9 had active forward motion of 70 degrees and 50 degrees for abduction. Thirteen days post-operation, case 10 had active forward motion of 60 degrees and 60 degrees for abduction.
The time from the original arthroplasty to the occurrence of the PHF was, on average, 111.76 (10.43-312.86) weeks. Cases 5, 9, and 10’s time from original arthroplasty to occurrence of PHF were unavailable. Apart from case 3, the time from PHF to the surgery was quick; with an overall average of 15.90 (1-133) days. There were two radial nerve palsies that were related to the initial post fall PHF (case 2 and 8). Preoperatively in case 2, the patient was noted to have radial nerve palsy with functional deficits. The nerve was identified intraoperatively and protected for eventual conservative management. The nerve was not severed but stretching upon identification. In Case 8, the nerve was found to be in the fracture site but it was not cut so it was freed. They were both managed with cock up splints with PT/OT rehab. Case 2 had sensation intact but the active motion deficiency did not resolve despite management. Case 8 had partial radial nerve resolution. Cases 1 and 5 both had post-operation infections that resolved with antibiotics and debridement if needed.
Follow-ups were done using the established standard of care of a 2 week follow up for wound check and removal of stitches or staples with subsequent visits for radiological and clinical analysis at 6 weeks, 2 months and 3 months. Patients were sent on standard protocol for PT/OT rehab following surgery. Average follow up for patients was 5.85 (3.4-12.8) months.
Periprosthetic humeral fractures remain a rare and complex complication. Management of these fractures is highly variable, but union can be achieved by surgical management as demonstrated by this study. Surgical management was the preferred method of treatment at this level 1 trauma center. With an average union of time of 13.27±2.90 (9.86-17.29) weeks, surgical management should be considered a valid treatment modality for PHFs. These patients have significant comorbidities with a Deyo-Charlson score of 7.1 on average but management with ORIF with locking plate with or without cerclage will still provide satisfactory results. Conservative treatment was attempted in three cases of the surgical cases; however, failure of adequate union resulted in each patient. We found the most common complication was radial nerve palsy. Based on anatomical location, this nerve is highly likely to be damage in a type B PHFs. When treating a type B fracture, special attention should be paid to the quality of the nerve based on anatomical proximity of the nerve to the fracture.
PHFs have a multitude of classification systems and recommendations of treatment based on each different classification. Worland et al.4 has a recommendation for each of the fracture types within his model of classifications. However, within some of these categories there is no preference between surgery or conservative treatment. Further, there is no distinction between different surgery techniques that are being used. Currently, there is no widespread consensus on recommendations or classification system. There is one consistency in terms of management; when there is a loose stem there is a wide-spread belief that there is a need for a revision. Most often it comes in the form of a long stem prosthesis.3–5,8,10–17
In a study done with Kurowicki et al.12 they identified 5 periprosthetic fractures that were treated with ORIF using a locking plate with “skive screws” to help achieve adequate fixation around the stem of the implant. The average union time in this study was 19 weeks. Another study using ORIF with plates for treatment of periprosthetic humeral fractures was done by Schoch et al.16 they used 4.5mm large fragment plate and a 3.5mm attachment plate to fix the fracture around the implant. The average union time in their five patients was 3.7 months. This study agrees with previous studies that ORIF with plates can achieve satisfactory union times as demonstrated by the similar union times. This study also demonstrates that this management can be done in patients with high comorbidity profiles.
PHFs can result from a multitude of surgeries including IM nail, elbow arthroplasty, and a shoulder arthroplasty. Intrahumeral stress risers insert an added complication of having a fracture between two prostheses. These complications require skilled management, especially when comorbidities are present. Comorbidities and the female gender require special attention in assessing the risk of complication. These factors have been linked to an increase in risk for complications especially intraoperatively humeral shaft fracture.18 Only one other study mentions patients’ BMI and Deyo-Charlson score with PHFs. Singh et al. analyzed patients from 1976 to 2008. Singh et al. analyzed risk of patients getting PHFs but not treatment outcomes in PHF patients’ comorbidity profiles. Comorbidities continually change over time. This requires and update in the literature for patient profile getting PHFs fractures and challenges that may ensue from these comorbidities that are common amongst this cohort of patients.
A limitation of this study was that the sample size was small given the rarity of the complication. Another limitation is a shorter follow-up that ended shortly after union times were achieved in patients.
Based on this level 1 trauma center’s experience, this case series is presented to add to the body of knowledge of a potential standard of care in PHF management. Currently, no randomized control studies exist on this topic and the majority of data used for management is based on case reports or a case series. Management of PHFs remains in its infancy while shoulder arthroplasty incidence continues to increase. In conclusion, the treatment of periprosthetic humeral fractures using ORIF with locking plate with or without cerclage wiring provides satisfactory outcomes in a patient population that usually includes significant comorbidities.
None.
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
None.

©2021 Liu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.