MOJ
eISSN: 2374-6939


Case Report Volume 12 Issue 5
1Orthopedics Service, Hospital José Joaquim Fernandes, Portugal
2Orthopedics Service, Hospital Garcia de Orta, Portugal
Correspondence: Filipa Gonçalves Pereira, Unidade Local de Saúde do Baixo Alentejo, Rua do Outeiral nº 40, 4715-142 Braga, Portugal, Tel 00351919010045
Received: October 06, 2020 | Published: October 30, 2020
Citation: Pereira FG, Brito F, Osório T, et al. Staple arthroscopic fixation of tibial ACL avulsion with concomitant lobenhoffer approach for a posterolateral tibial plateau fracture. MOJ Orthop Rheumatol. 2020;12(5):104-107. DOI: 10.15406/mojor.2020.12.00529
Tibial eminence avulsion fracture or anterior cruciate ligament avulsion fractures are extremely uncommon, especially in adults. The objective of the treatment is to provide knee stability, allow early rehabilitation and reduce complications rate. Several methods for fracture fixation have been described in the literature. We report a case of a 39 year old male who presented with a severe tibial plateau fracture and an avulsed ACL which was arthroscopically fixated with a staple. This is a unique, simple and affordable technique with excellent clinical and functional results.
Keywords: ACL avulsion, staple fixation
ACL, anterior cruciate ligament
Tibial spine avulsion fracture is a rare injury, especially in skeletally mature patients. In literature this type of injury is mostly reported in pediatric population.1,2 The classical injury mechanism is due to hyperextension associated with a valgus or rotational force, usually secondary to a fall from a bicycle, a motor vehicle accident or associated with sports involving pivoting and axial load like ski or football. This leads to the avulsion of the tibial attachment of the ACL also known as tibial spine intercondylar fracture.3 High energy trauma is necessary to overcome the tensile bone strength at ACL attachment, therefore a higher incidence of associated injuries such as tibial plateau fractures and other ligaments tears is identified.2,4,5
The modified Meyers and McKeevers classification is the most commonly used (Figure 1). Type I nondisplaced fractures do not require surgical treatment, whereas Type III and IV are managed surgically. There is some debate about type II, but it is acknowledged that that a fragment displacement <5mm can be treated with close reduction and immobilization for 4 to 6 weeks.6
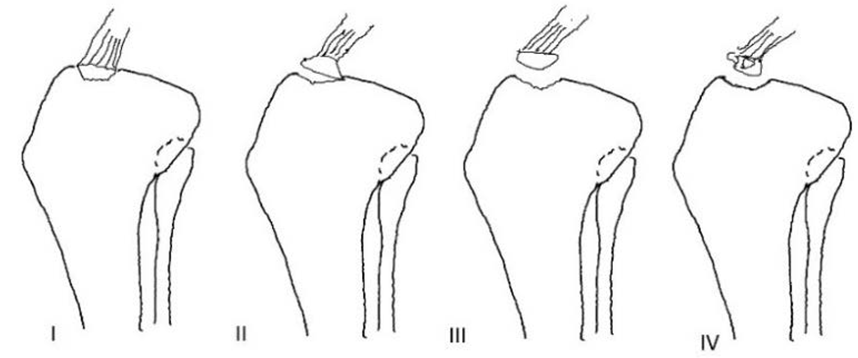
Figure 1 Modified Meyers and McKeever classification of tibial eminence fractures. Modified Meyers and McKeever classification. Figure (a) is a Type I and is non-displaced; (b) is a Type II which has a displaced anterior margin and hinged posterior cortex; (c) is a Type III and there is absence of any bony contact; (d) is a Type IV and is comminuted. Taken from Lubowitz JH, Elson WS, and Guttmann D, Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fractures Arthroscopy, 2005. 21(1): p. 86e92.
Several methods have been described for surgical treatment of tibial spine fractures. The most frequent techniques described in the literature are screw fixation with or without washer, suture fixation, wires and suture anchors but a gold standard treatment is yet to be determined.7–9
The Goal of surgery is to achieve an adequate fracture reduction and fixation that restores ACL length, enables proper healing and early rehabilitation.10 The authors present a valid, affordable and easy accessed arthroscopic method of fixation for these type of fractures using a staple, with excellent functional and clinical results.
A 39 year old male presented after a motorcycle accident with swelling and impairment and disability of the left knee. Physical examination revealed a large knee effusion with intolerance to passive range of motion. Neurovascular injuries and compartment syndrome were excluded.
A preliminary orthogonal radiograph revealed a postero-lateral tibial plateau fracture and raised the suspicion of a displaced medial tibial spine anterior fracture (Figure 2). The patient underwent a CT-scan to further evaluate the fracture pattern (Figure 3) and was immediately immobilized with a long leg posterior cast with the knee in extension.
Six days after initial presentation, the patient underwent arthroscopic and open surgery
First step- A Lobenhoffer approach was performed to reduce and fixate the postero-lateral tibial plateau fragment with two 6.5mm cannulated screws with washer and an anti-gliding 3.5mm plate. This approach was selected due to the fracture pattern and also to the fact that reduction is achieved with hiper-extension.
Second step- Arthroscopy was performed for tibial plateau reduction, evaluation and fixation of tibial spine avulsion fracture. A large osseous fragment was found attached to ACL (Figure 4), with no comminution. No meniscal or intermeniscal ligament tissue was found in the fracture bed. There were no meniscal nor PCL injuries. Maintaining the knee in 90º of flexion, the medial tibial spine was temporarily stabilized with K wires percutaneously and fixated with a 10mm staple trough the antero-medial portal that was created in more superior position to provide a greater angle for the introduction of the staple handle (Figure 5).
Postoperative radiograph confirmed satisfactory anatomic fracture reduction (Figure 6)
The Patient was immobilized with long leg cast for 4 weeks. At the time of removal, he was showing signs of knee stiffness (-5º of extension and 60º of flexion) and thigh muscle atrophy. An intensive rehabilitation program was started with isometric and closed chain exercises, with partial weight bearing in the first 2 weeks after cast removal.
Radiological union was achieved 8 weeks following surgery (Figure 7).
One year after surgery the patient had no limitations in his daily activities, no pain or subjective instability and had returned to his previous activity level. He recovered full range of motion and had a Lysholm score of 91 (Figure 8 &9).
Tibial spine fractures typically occur at the distal insertion of the ACL (antero-laterally to the medial tibial spine). Radiographs and CT scan can be useful for the diagnosis but due to its location, frequent surrounding tissues in the fracture bed, and high frequency of associated injuries in adults, MRI can be a major advantage in this type of injuries.11
The authors consider the use of MRI of extreme value. Unfortunately, in this case de MRI could not be performed at in useful time.Despite lack of consensus regarding the treatment of tibial spine avulsion fractures, an arthroscopic approach has some known advantages compared to an arthrotomy because it is less invasive and has a lower stiffness risk. Additionally, arthroscopy allows a more accurate approach of the fracture, direct reduction control, evaluation and treatment of associated injuries, early mobilization, reduced hospitalization time and reduced morbidity.12
Direct visualization is of utmost importance, since the reduction can be blocked by the interposition of the inter-meniscal ligament or the anterior horn of medial meniscus.In addition, fixation methods can be controversial. Mechanical studies have shown that suture fixation and suture anchor have a higher load to failure and survival rate during cyclic loading compared to screw fixation.13
In this case the authors describe the use of a staple, placed arthroscopically to fixate the avulsed LCA. The medial tibial spine fracture line identified extended anteriorly up to tibial border. Therefore, the staple placed in the anterior part of fragment could not interfere with femur extension. This technique can be performed without specific arthroscopic instruments and is also an affordable option compared to the others with similar clinical and functional scores.14
Disadvantages of the use of staple fixation include the risk of iatrogenic fracture while hammering, articular surface damage during its placement, increased pull out failure compared with suture fixation and increased rate of hardware removal.In the presence of small or several fragments a secure fixation may be compromised with the use of a single staple, so careful assessment of preoperative images is required.
The most common complication is ACL laxity either if the patient is treated surgically or nonsurgically, with positive Lachman test in 20-60% of patients and positive Pivot Shift test in 8-40%. An association with the laxity postoperatively and the severity of the injury has been documented.8,15
Even though subjective and functional instability are not often observed, since residual laxity is well tolerated, nearly 20% of patients will need an ACL reconstruction.16,17 Another common complication is arthrofibrosis with an incidence rate of 10-29%, primarily related to immobilization, concomitant ACL rupture and surgery time exceeding 2hours.12,18,19 No correlation was found between the type of fixation and knee stiffness in literature.1,8 Risk Factors for postoperative stiffness include long immobilization period, complete fracture displacement, malunion, hardware protrusion, more than one surgical intervention,20 and increasing age.21,22
In the presented case, the patient was immobilized for 4 weeks, as recommended in several rehabilitation protocols. In the authors’ opinion, immobilization time could have been reduced, since the fracture fixation was strong and earlier mobilization might have prevented the initial stiffness. In this particular case weight bearing could not be started earlier because of the tibial plateau fracture.6,10
Tibial spine fractures are uncommon injuries and usually associated with secondary injuries, especially in skeletally mature patients.The approach of these fractures is still controversial, as well as the fixation method used. Gold standard treatment is yet to be determined but the goal is to have an adequate reduction, ACL tension and secure fixation in order to start early and aggressive postoperative rehabilitation and reduce complications. In the authors’ opinion, arthroscopic staple fixation is a simple and effective option with favorable clinical and functional results.
Dr. André Lopes Vasques, Catarina Amorim
The authors declare no conflict of interest regarding the publication of this article.
None.

©2020 Pereira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.