MOJ
eISSN: 2374-6939


Case Report Volume 6 issue 4
1Orthopaedic Department of Centro Hospitalar do Algarve, Portugal
2Hospital particular do Algarve, Portugul
3Orthopaedic Department of Hospital Dona Estefania, Portugal
4Orthopaedic Department of Hospital Beatriz Angelo, Portugal
Correspondence: Tania Pinto Freitas, Faro Hospital, R. Leao Penedo, 800086 Faro, Portugal
Received: October 10, 2016 | Published: November 21, 2016
Citation: Freitas T, Couto A, Ovídio J, Vide J, Amaro F (2016) Spontaneous Bilateral Femoral Neck Fracture Rare Presentation of a Metabolic Bone Disease. MOJ Orthop Rheumatol 6(4): 00232. DOI: 10.15406/mojor.2016.06.00232
A 50 year old woman was observed at the emergency department after falling from her own height after sudden failure of the lower limbs, which led to bilateral femoral neck fracture.
She has had multiple repeated urinary tract infections, nephrolithiasis with several admissions in urology department and extracorporeal lithotripsy episodes with shock waves. She also had history of surgical removal of kidney stones.
The Laboratory tests revealed high calcemia (13.2 mg/dl) and alkaline phosphatase (445); normal phosphate and magnesium, normal Calcitonin; high parathyroid hormone(> 2500 pg / ml). Hyperparathyroidism caused by a parathyroid adenoma was diagnosed after ultrasound, biopsy and scintigraphy were performed. Radiographs revealed classic and severe bone findings in PHPT, features which were common in the past but are thought to be rare at this modern age.
Parathyroidectomy was performed at the same time as a bilateral cemented total hip arthroplasty. She developed the hungry-‐bone syndrome 5 days postoperatively, which resolved with administration of bisphosphonates, calcium and D vitamin.
Keywords: Hip, Fracture, Bilateral, Hyperparathyroidism, Parathyroid, Nephrolithiasis
Femoral neck simultaneous bilateral fractures are extremely rare and have been associated with high-‐energy trauma, and less frequently, low-‐energy trauma, seizures, electric shock, electroconvulsive therapy and metabolic bone diseases,including hyperparathyroidism.1,2
When they occur in a low-‐energy trauma context, this leads to the underlying pathology suspicion. Hyperparathyroidism is a common metabolic bone disease affecting 7/1000 people and 21/1000 women in post menopause period.3,4 The diagnosis is easily confirmed using clinical analysis.
Our goal is to report the maximum spectrum of severity, and the various manifestations of hyperparathyroidism in the rare cases of long evolution of the disease. We highlight the surgical treatment options and rare complications, which also occurred in the present case.
The authors present the case of a 50 years old woman that came to the emergency department afte falling from her own height, caused by sudden failure of the lower limbs.
Her past medical records consisted of repeated urinary tract infections (since 2009), nephrolithiasis with several admissions in the urology department and extracorporeal lithotripsy episodes with shock waves. She also hadhistory of surgical removal of kidney stones (Figure 1) She complained about bilateral knee pain, asthenia and progressive muscle atrophy.
The physical examination showed external rotation of both legs and pain with hip mobilization. On the X ray there was marked osteopenia and bilateralfemoral neck fracture Garden IV (Figure 2); lytic lesions of the skull; osteolysis of the distal phalanges; osteitis fibrosa cystica / brown tumour (Figure 3).
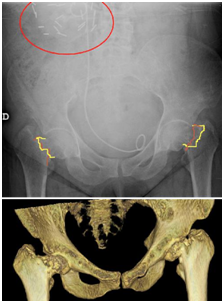
Figure 2 X ray showing bilateral femoral neck fracture and kidney surgical Staples; 3D reconstruction.

Figure 3 Lytic lesions of the skull; distal phalanges osteolysis; osteitis fibrosa cystica / brown tumour.
The Laboratory tests revealed:
Anaemia, erythrocyte sedimentation rate 81 U/L, normal electrophoresis, normal thyroid function. High calcemia (13.2 mg/dl) and alkaline phosphatase (445 mm/h); normal phosphate and magnesium, normal Calcitonin; high parathyroid hormone (> 2500 pg / ml).
Hyperparathyroidism originating in a parathyroid adenoma was the diagnosed and confirmed by ultrasound, biopsy and scintigraphy (Figure 4) .
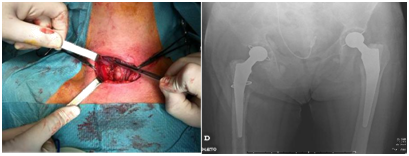
Figure 5 Partial parathyroidectomy and post operative X ray ofbilateral cemented total hip arthroplasty.
Postoperatively she spent two days in the intensive unit care (ICU) requiring transfusion of two red blood cells units. She also suffered from a Hungry bone syndrome that was controlled with bisphosphonates, calcium and vitamin D.
She was released from the hospital thirty days after surgery, walking with crutche, continuing her recovery with physical therapy program. At four months after surgery she walks with no need of external support.
Nephrolithiasis is a multifactorial disease. Hyperparathyroidism is a known risk factor for nephrolithiasis, which is observed with an estimated prevalence of 7–40%. Furthermore, among patients presenting with renal stones, the prevalence of concurrenthyperparathyroidism is around 2%-‐ 8%.3,5
Seeking for the aetiology in this case could have prevented the progression for severe disease.6 Cancer and multiple myeloma can cause high calcium levels, lytic lesions and fractures, but only hyperparathyroidism and familiar hypocalciuria occur with increased parathyroid hormone.7 Brown tumors are an extremely rare clinical phenomenon in developed countries as a result of earlier diagnosis and treatment of hyperparathyroidism. Such rare and multiple benign lesions constitute a real challenge for the clinician in the differential diagnosis of cancer.4,8
Hungry bone syndrome is rare but expected in the post operative period of the most severe cases. The advanced bone disease conditioned surgical technique regarding the need for cementing and the type of implant used.9-12
Hyperparathyroidism is a frequent cause of nephrolithiasis, and should therefore be excluded in these cases, avoiding the most severe forms of the disease. In here the consequences imply mobility limitation, reduced bone quality and the need for prosthetic revision in the future.
All the other colleagues helped to treat this patient and aided in writing this case report.
None.

©2016 Freitas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.