MOJ
eISSN: 2374-6939


Case Report Volume 11 Issue 2
Centro Hospitalar Universitário do Algarve, Portugal
Correspondence: Filipe Medeiros, Centro Hospitalar Universitario do Algarve, Estrada do Poço Seco, 8500-338 Portimao, Portugal, Tel +351 282 450 300
Received: April 29, 2019 | Published: April 30, 2019
Citation: Medeiros F, Correia B, Sousa F, et al. Septic arthritis in ochronosis’ patient. MOJ Orthop Rheumatol. 2019;11(2):110-113. DOI: 10.15406/mojor.2019.11.00482
Alkaptonuria is a rare autosomal recessive metabolic disease caused by homogentisic acid oxidase enzyme deficiency. High homogentisic acid levels will eventually result in black deposits in skin, sclerae, connective tissues (ochronosis) and urine (alkaptonuria). It can lead to early degeneration of joints. The diagnosis is often delayed because of its low prevalence and non-specific early symptoms. We describe a clinical presentation of ochronotic arthropathy, on a complex patient, who developed a septic arthritis of the knee. The patient was under immunosuppressive therapy, due to a previous colon adenocarcinoma and received a knee corticosteroid infiltration, two weeks before the onset of pain. It was performed joint lavage and arthrolysis by arthrotomy. During the procedure, we found a dark pigmentation on bone. Urine tests were positive for alkaptonuria. The patient completed an antibiotic cycle and rehabilitation, with satisfying improvement in knee’s range of motion. At four years follow-up the patient can walk without crutches, presents minor knee pain. High level of suspicion and awareness is needed to diagnose ochronosis. The joint destruction in a complex patient must be carefully analysed. We’ve chosen a non-aggressive therapeutic management, but according to the literature, other therapeutic strategies could have also been chosen, like joint arthroplasty. We’ve declined this option because the patient is still doing antineoplastic treatment.
Keywords: alkaptonuria, ochronosis, septic arthritis, knee
Alkaptonuria is a rare autosomal recessive metabolic disease, with an incidence of 1:125,000 to 1:1 million worldwide. First description of Alkaptonuria was done by Garrod in 1908, that also recognized it to follow classic Mendelian recessive inheritance.1 The genetic defect is mapped to the HGD gene and more than 90 different mutations have been identified to date.2 Alkaptonuria is caused by homogentisic acid oxidase enzyme deficiency, that results in high homogentisic acid levels. It will eventually result in black deposits in skin, sclerae, connective tissues and urine. Ochronosis, dark pigmentation of connective tissues, is the musculoskeletal manifestation of this disease.3 It can lead to early degeneration of cartilage, leading to secondary osteoarthritis,4 by a mechanism that has not been understood.2 A worldwide review conducted in 2004 found that approximately 600 cases of ochronotic arthropathy have been reported since 1962.1 The diagnosis is often delayed because of its low prevalence and non-specific early symptoms.4 The diagnosis occasionally is discovered intraoperatively in patients undergoing joint replacement surgery through the observation of the characteristic bluish-black pigmentation of the tissue surrounding the joint.2 Ochronotic arthropathy manifests first in the spine. Subsequent degeneration is on the knee (most commonly affected, in 64% of cases), hip, and shoulder. Small joints of the hand and foot usually are not affected.2 Homogentisic acid and its oxidation products could accumulate also in the sclera, skin, heart valves, the cartilage of the nose and ears, tendons, ligaments, renal tubule epithelial cells, pancreas, and arteries.5–7 In this paper, it is described a clinical presentation of ochronotic arthropathy with septic arthritis in the knee, of a complex patient.
A 46-year-old man presents in our emergency with fever, severe left knee pain with inflammatory signs, within one week of evolution (Figure 1). He had sigmoid colon adenocarcinoma, submitted to left hemicolectomy (February 2013), retroperitoneal metastasectomy (January 2014), and chemotherapy. An intraarticular infiltration with steroids was performed two weeks before on that knee. An initial white blood cell count was slightly elevated at 11.3/mL with elevated C-reactive protein of 160.1 mg/L. A possible septic arthritis was diagnosed and it was performed evacuated arthrocentesis for microbiologic analysis and joint lavage with hematopurulent content output. He started empiric treatment with intravenous flucloxacillin 2g qds and gentamicin 240mg. No significant clinical improvements while awaiting results, underwent knee arthrotomy, joint lavage, extensive debridement and arthrolysis. During the surgery, it was found purulent content and dark pigmentation on bones and soft tissues (Figure 2). Postoperative microbiology samples reveal metecilin-sensible Staphilococcus aureus infection. It was made urine tests of alkaptonuria, that were positive. After maintaining the intravenous flucloxacillin for 2 weeks with good response, the treatment was shifted for oral with rifampicin, according to antibiogram. Besides antibiotic cycle, rehabilitation was also important for the treatment, and the patient improved his endurance with satisfying range of motion of the knee. After four years follow-up, the patient can walk 90 with crutches, with minor knee pain. He also presents complaints on both shoulders. In physical exam he has limitation on range of motion in knees (Figure 3) and shoulders. Radiologic findings show osteoarthrosis joints (Figure 4), but no additional treatments were done or proposed.
The diagnosis of alkaptonuria may be suspected by an accurate physical examination. Dark pigmentation on sclera and on ear cartilage are typically described,6 but not so easy to find in these patients. The classic clinical trial of alkaptonuria is homogentisic aciduria, ochronosis and ochronotic arthropathy.7
Overall, the incidence of ochronotic arthropathy in patients with alkaptonuria is low.2 Differential diagnosis must be done with ankylosing spondylitis and degenerative osteoarthosis.7 However, certain radiologic findings allow its differentiation, like unusual sites of joint involvement (severe glenohumeral joint disease in the absence of significant trauma, advanced changes in the sacroiliac joints and symphyseal joints), and joint-space loss with an unusual pattern (symmetrical joint-space narrowing in the hips and shoulders, and isolated lateral femorotibial loss of knee joint space) (Figure 4). Involvement of large peripheral joints usually occurs about 10 years after spinal changes.7 Darkening of the urine is a common diagnostic feature and should be considered in children even producing it unusually.2 Diagnosis can be confirmed using gas liquid chromatography, thin-layer chromatography, or enzymatic spectrophotometry to analyse the amount of homogentisic acid in the patient’s urine. Arthroscopy has been found to be an effective diagnostic tool in cases of suspected ochronosis.2

Figure 2 Findings intraoperatively: a) joint and cartilage surface destruction; b) dark pigmentation of a tissue.
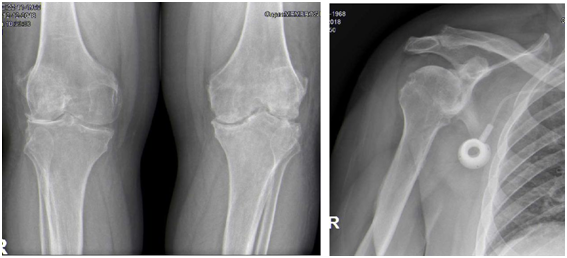
Figure 4 Radiologic findings showing osteoarthrosis joints: A. Bilateral Knee anteroposterior x-ray; B. Right Shoulder x-ray.
For septic arthritis, it is strongly recommended immediate antibiotic therapy and evacuation of purulent material as often as necessary. However, few published data are available that addresses the most effective methods of evacuating this purulent material. Gächter et al. defends that the degree of debridement required according to the intraoperative stage of the joint.8 Our open approach was based on bad clinical stage of the high-risk patient and radiographic osteolysis, classifying in stage IV. In these cases, open arthrotomy is recommended to effectively eradicate the infection in one-time surgery, with debridement, removal of loose fragments and curettage the cysts. When patients’ symptoms lasting four to ten days, Kirchhoff et al. treated them by open surgery or were converted from arthroscopy to open debridement due to advanced stages (Gächter III).9 Arthroscopic treatment is also indicated with septic arthritis on native knees with low reinfection rate and good functional outcomes.10 Although, Aim et al. showed that 25% required more than one arthroscopic lavage, and factors significantly associated with arthroscopic treatment failure were Gächter stage III or IV and positive drainage-fluid cultures after 24 h.11 It’s consensual that all incisions must be closed completely (no drains) and a aggressive early range of motion postoperatively must be routinely emphasized. Another controverse theme is the empiric antibiotic regims. Current antibiotic choices should be made based on the likely etiological organisms (geographic variation and resistance patterns) and subsequently modified in light of culture and sensitivity results. Our choice is justified by UK guidelines on initial antibiotic choice.12 Fusidic acid may also be considered as an adjunct because of apparently good penetration into bone.12 Although it should be noted that MRSA is gradually emerging and has been recently reported a prevalence of up to 17%.9 With regard to the choice of antibiotic, a multidisciplinary approach with microbiologists is essential.
Currently, there is no proven therapy or prophylactic treatment for alkaptonuric patients.2,4 Treatment options are administration of nonsteroidal anti-inflammatory drugs, intake of preparations containing glucosamine and chondroitin sulphate, intra-articular injection of hyaluronic acid and steroids, arthroscopic debridement of the affected joint, and arthroplasty. Treatment is generally supportive and aimed at preventing or minimizing the effects of ochronotic arthropathy, like others arthritis. More specific, the antioxidant properties of vitamin C have been shown to help slow the conversion of homogentisic acid to its pathologic polymeric intermediate.2,6 Dietary restrictions of foods containing phenylalanine and tyrosine have been shown to be effective in limiting symptoms of ochronotic arthritis because this reduces the production of homogentisic acid. Vitamin E and N-acetyl cysteine are potential therapies because of their scavenging of free radicals and consequent limitation of oxidative damage to joint tissue.2 The drug nitisinone is being researched as the first potential treatment for alkaptonuria; in previous research it was shown to reduce the levels of HGA by up to 95%.6
In our patient, we focus the challenge to decide which tissue were infected or simply with dark pigmentation. Sometimes it was difficult to know until where we should do the debridement. This is the second case described in literature with infection and ochronosis, but there not seems to have any relationship between them.4 The immunocompromised system and infiltration on the knee must have acted as risk factors for septic arthritis in this case. The joint destruction in these complex patient (with adenocarcinoma, ochronosis arthropathy and septic arthritis) was analysed carefully and it was chosen a non-aggressive management. Other therapeutic strategies could also have been considered according to the literature. Arthroplasty performed in patients with ochronotic arthropathy suggests that the procedure is effective in the alleviation of joint pain and the improvement of mobility,2 even in shoulders.3 However, it was declined this option because he is still doing antineoplastic treatments, and there is no benefit in some surgery or even infiltration.
About prognosis, patients with alkaptonuria can expect a normal life. Nevertheless, the complications of debilitating arthritis, chronic kidney disease, and ochronotic skin alterations will occur.6
Alkaptonuria is a rare autosomal recessive metabolic disease, that could be presented by ochronotic arthropathy. A high level of suspicion and awareness is needed to diagnose ochronosis. It is often only found during arthroplasty procedures. There is no definitive cure, and the treatment is aimed at controlling and ameliorating symptoms, similarly to a normal arthropathy. Surgical treatment may be necessary in some cases. Nevertheless, perioperative management may require careful considerations relative to common associated comorbidities in this disorder and should be discussed with the patient.

©2019 Medeiros, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.