MOJ
eISSN: 2374-6939


Case Report Volume 15 Issue 3
1Pediatric Orthopedic and deformity correction Surgeon, Almoosa Hospital, Saudi Orthopedic Board Program Director, Almoosa Specialist Hospital, Saudi Arabia
2Orthopedic Resident, King Fahad Hospital of Hofuf, Kingdom of Saudi Arabia
Correspondence: Mohammed Alarbash, Orthopedic resident, King Fahad Hospital Hofuf, Saudi Arabia
Received: June 15, 2023 | Published: June 28, 2023
Citation: Bo-Eisa AN, Alarbash MS, Al Khars AF. Scurvy mimic acute Leukemia in a female child and review of literature. MOJ Orthop Rheumatol. 2023;15(3):123-128. DOI: 10.15406/mojor.2023.15.00631
Scurvy is a nondiscriminatory disease process resulting from a nutritional deficiency of ascorbic acid (vitamin C). Identifying scurvy can be demanding due to the perceived rarity of the condition, and it can become a tricky diagnostic question given to the variety of nonspecific symptoms, including skeletal and other systems affected. Diffuse musculoskeletal pain in children with no specific cause is usually fugue. Differential diagnoses include growing pain, joint hypermobility, psychogenic disorders, somatoform disorders, inflammatory diseases, and malignancies. Children with leukemia can be referred to the orthopedic when the diagnosis is still unknown; in fact, musculoskeletal pain or radiographic abnormalities can be very frequent at presentation and it could be the primary manifestation of leukemia and scurvy. We report one of rarest cases of patient present with feature of scurvy in developed area mimic Leukemia.
Keywords: scurvy, leukemia, inability to bear weight
Nutritional bone disease is an umbrella term that includes a broad spectrum of clinically different diseases that share the common finding of an unusual bone chemical environment leading to a defective skeleton abnormality.1 Usually characterized by a staged clinical presentation and manifestation that are commonly reversible once the underlying defect has been treated.1,2 Abnormalities of minerals include calcium, phosphorus, magnesium, or vitamin D and vitamin C. Scurvy is unfair disease process resulting from a nutritional deficiency of ascorbic acid (vitamin C).1,2 Scurvy was first noted in ancient Egypt. The disease's name was later derived from the Latin.1 There have been numerous scurvy epidemics in the past. When lacking in vitamin C, which is a necessary exogenous vitamin, people experience a variety of symptoms.2 In modern developed countries, this condition now extremely uncommon and may only occasionally be faced.3 Scurvy is considerably more uncommon among children, particularly in cases where there are no underlying medical conditions. Furthermore, the majority of physicians in developed countries had almost definitely never heard of childhood scurvy, which had long since been an outdated memory.4 Overlapping clinical manifestations and Imaging findings in scurvy could be suggestive of malignancy or other inflammatory disease.6,7 We present a case report of baby girl compline of long-standing lower limb pain and weakness, later on she was diagnosis with scurvy.
This is 2 years and 6 months old baby girl present with history of inability to bear weight and lower limb pain and weakness in the last 3 week. Pain was progressive over the last 3-weeks, pain not response to analgesia, it aggravated by bearing wight, relieved by rest. Associated with bilateral lower limb weakness and swelling. Baby was walking normally before. After a few weeks, the pain persisted, and the swelling was worsened. She tended no move her leg. She was also presented with general weakness.
Family give history that had multiply visit to other hospital no diagnosis was found. There was no recent history of fever, weight loss, trauma, bruising, no rashes, rhinorrhea, cough, sore throat or vomiting. She had received the recommended and compulsory vaccinations. The child was born full-term with an unremarkable neonatal history. She started walking at age of 12 months, and other neurodevelopmental milestones were normal. Baby not known to have any previous surgery and other chronic disease. On physical examination, baby was vitally stable, no dysmorphic feature, no neurological or cardiovascular abnormalities were noted. There was no hepatosplenomegaly or lymphadenopathy. No pallor, no petechial hemorrhages, no gum hypertrophy. Multiple skull swelling the largest 2cmX 2cm the other behind the ears (3 swelling) in the head hard with no warm or tenderness. Musculoskeletal examination showed bilateral wrist swelling, tenderness, mild hotness, decrease ROM of both wrists, distal neurovascular intact. Also, there was bilateral knee swelling, tenderness with hotness, decrease ROM, both knee joints had effusion and flexion contracture of 20◦ with further flexion possible only to 45◦ due to pain (Figure 1).
Patient underwent serial investigation include blood work up and radiological imaging. The laboratory data results were as follows: white blood cell count 2.98 lymphocyte count 60%, platelet 161, hemoglobin 7.2 g/dL. C-reactive protein level was <5. Sickle cell test and electrophoresis were negative. All virology and other blood work up were negative. Blood culture and urine culture were normal.
The radiographs bilateral ulnar symmetrical distal metaphyseal eccentric osteolytic lesions are seen with disruption of the medial cortex; however no periosteal reaction. Also, there is small osteolytic lesion within the distal radius (Figure 2). Both knees showed signs of osteopenia, the thick sclerotic metaphyseal line above a widened physis, and small beak-like excrescences at the metaphysis of both tibias (metaphyseal clefts). Ring of increased density surrounding epiphysis (Wimberger ring) (Figure 3). US guided aspiration of both knees show no signs of infection. MRI of wrist was done which show diffuse bilateral bone marrow oedema of the distal ulna and radius both sides. This is associated with evidence of diffuse periosteitis and soft tissue oedema however no apparent fluid collections. Subcutaneous oedema is also identified. No apparent acute fractures. No focal osseous lesions. Intact extensor and the flexor tendons bilaterally and bone: Generalized bone marrow oedema is seen more pronounced around the knee and wrist joints. (Figure 4).
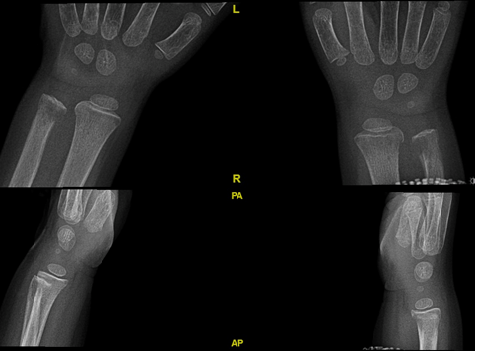
Figure 2 Bilateral wrist x ray AP and lateral view show ulnar symmetrical distal metaphyseal eccentric osteolytic lesions and disruption of the medial cortex with small osteolytic lesion of distal radius.

Figure 3 Bilateral knee x ray AP and lateral view show joint effusion with osteopenia, the thick sclerotic metaphyseal line above a widened physis, and small beak-like excrescences at the metaphysis of both tibias (metaphyseal clefts).
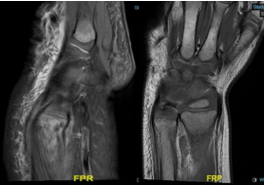
Figure 4 MRI of the wrist Diffuse bilateral bone marrow oedema of the distal ulna and radius both sides. This is associated with evidence of diffuse periosteitis and soft tissue oedema.
On the other hand, those features were giving a suspicious this case either chronic recurrent multifocal osteomyelitis or metabolic bone disease in form of scurvy or malignancy which is less likely Patient was on broad spectrum intervenes antibiotic for 2 weeks and no improvement. So, we began vitamin C therapy 100 mg per day 3 times for 2 weeks. The pain has significantly improved but not subsided, swelling on the leg and ankle was also decreased. She started to move knee and ankle joint, but still, she is not fully cooperative to walk. Patient underwent bone biopsy and culture. Histology show B-cell leukemia even she is positive for malignancy and had a feature of scurvy. Patient was improving on vitamin C supplement. After that patient start course session of chemotherapy. After complete chemotherapy patient have almost normal walking function.
Difficult in bearing wight and joint pain are common chief complaint in the pediatric emergency department, and it has a broad differential diagnosis. It can be a challenging symptom to elucidate in the pediatric patient, especially in nonverbal children or kids with sensory or behavioral developmental issues.9 In children, bone and joint pain and refusal to walk generally alerts the physician to possible osteomyelitis, septic arthritis, and malignancy.10 Scurvy may have features of pseudo-paralysis, simulating osteomyelitis or tumor as differential diagnosis.5
Scurvy is a diagnosis that could be missed easily. It is rare cause of bone and joint symptoms, and this rarity of occurrence as compared to other nutritional deficiencies frequently leads to delayed recognition of this disorder 11. The majority of individuals had a comorbidity that raised their risk of vitamin C insufficiency. These include hematological illnesses, severe food allergies, neurological disorders such autism, anorexia, cerebral palsy, and developmental delay, as well as other dietary restriction factors like fructose intolerance.3,5 An unusual aspect of the present case was the absence of any potential risk factors, which demonstrates that scurvy may still be occasionally encountered in the pediatric population, even in individuals with no predisposing disorders, living in families without unusual eating habits. Also, this case was having a feature of scurvy even with no risk factor and associated with leukemia.
Furthermost of characteristic disorders of vitamin C deficiency can overlie with rheumatological, infectious or hematological malignancy diseases, viewing a broad variety of musculoskeletal and mucocutaneous manifestations, consequently mimicking other pediatric conditions 5. The early signs include nonspecific features include irritability, loss of appetite, low grade fever, and later, petechiae, ecchymoses, hyperkeratosis, and corkscrew hairs.
In 80% of scurvy patients, there are musculoskeletal symptoms.7 In addition, like in our patient, bone disease occurs more frequently in children than in adults as a symptom of the disorder.12 The following are the radiographic signs of pediatric or infantile scurvy: a transverse metaphyseal line of increased density, a transverse metaphyseal line of decreased density (scurvy line), metaphyseal excrescences of the beaks, subepiphyseal infractions, increased density of periostitis and epiphyseal shell with a central lucency (Wimberger’s sign of scurvy). The radiographic findings including osteopenia, thick sclerotic metaphyseal line, metaphyseal excrescences of beaks, Wimberger ring were observed on the radiograph of our patient. However, those sings were found in our patient and associated with leukemia. The laboratory results showed an inflammatory illness, and we initially could not detect the possibility of scurvy due to the rarity and lack of understanding of the MRI findings of scurvy.9,11,12 A low vitamin C level in the plasma is specific for the diagnosis of scurvy; however, this is a not always a reliable indicator because plasma levels may be normal with recent intake of ascorbic acid.9,12 This is present in our patient which show low hemoglobin and MRI result give suspicious of infection. In addition to that patient was on iv antibiotic and there is no improvement. In our patient due to the unresponsiveness and further progression of the disease despite antibiotic therapy, we then suspected the possibility of scurvy or another hematological malignancy. Fortunately, our patient’s symptoms decrease after vitamin C supplementation.3 But our patient not completely return to normal function, we decide to proceed with bone biopsy which show picture of leukemia with B cell lymphocyte. So, our patient having both feature of scurvy as radiological sings and proccing of disease and involve in malignancy as patient not completely improve vitamin C. Our finding suggests that scurvy it could present with other malignancy, and it could the initial presentation of malignancy or it might hide the presentation of other tumors or metabolic bone disease. F. Miraj, A. Abdullah et all had presented a case with picture of fibrous tumor on histopathology however the clinical and radiological findings were not consistent with it. So, feature of malignancy it could be present but the diagnosis of scurvy mainly clinical with help of radiological sings. moreover, scurvy could superimposed by malignancy and the reverse is true.8
Though scurvy is a rare and ancient disease, it should not be left in the pages of a history book.5 Whenever not readily diagnosed, the outcome may be unfavorable; the consequences of scurvy may be relevant and include intensive and invasive investigations, hospital admission with prolonged hospital stays, physical disability and even severe complications such as severe infections and cerebral hemorrhage or hemopericardium, which may be fatal if also untreated in children.7 This case report emphasize that scurvy is not a disease of the days-of-old but is present in today’s society, including in developed countries. Also, always think that scurvy could associated with malignancy and might be the chief compline of malignancy. Therefore, a high level of suspicion should be kept in mind even in people with no identified risk factor.
This is the review of all literature started from 1999 to 2023(include this case). We exclude adult patient we focus on only pediatric patients. Almost all patient express musculoskeletal symptoms and sings, some of patient report gingiva symptoms. On average almost all patient report chronic compline of lower limb pain and no immediate diagnosis were found. From all review cases had been have risk factor except our patient. Risk factors include developmental delayed seizure, food allergies. The most lab found is anemia, some institution report low level of vitamin C as diagnostic value. Most patient report classical finding of x ray for scurvy, some MRI give an idea that this picture of malignancy or chronic osteomyelitis, some patient underwent histopathology and bone biopsy which result on chronic inflammation with sub periosteal collection, other biopsy show picture of suspicious malignancy. All patient received treatment with vitamin C and there was significant improvement after treatment. Below table summary all review studies (Table 1).
|
Reference |
Age |
Symptoms/Signs |
Risk factor |
labs |
Radiology |
Pathology |
Treatment |
|
Bo-Eisa et al. (2023) This is study |
1 Y |
inability to bear weight and lower limb pain and weakness |
Normal |
Lowe hemoglobin
|
Feature of scurvy |
Bone biopsy B cell leukemia |
Yes |
|
Gicchino MF et al.6 (2021) |
4 Y |
lower limbs pain and refusal to walk |
Developmental delayed, eat disorder |
low iron and vitamin D level, low levels serum vitamin C |
generalized osteopenia including a ground glass appearanc Pelkan spur |
no |
yes |
|
Christopher Luckow et al.9 2020 |
5 Y |
progressive abnormal gait and difficulty bearing weight |
nonverbal autism |
vitamin C level low |
MRI: multifocal osseous marrow signal abnormalities, |
no |
yes |
|
Gallizzi et al. 3 2020 |
3 Y |
diffuse lower-extremity musculo- skeletal pain, and refusal to walk |
developmental delay, neurologic disorders, |
Lowe hemoglobin |
Feature of scurvy |
non |
yes |
|
Faisal Miraj et al.8 2020 |
3 Y |
pain and swelling on his left lower limb |
diet insufficiencies |
Lowe hemoglobin |
osteopenia, sclerotic metaphyseal widened physis, and small beak-like excrescences at the metaphysis of both tibias. |
histopathology suggested fibro-osseous tumors |
yes |
|
Hahn et al.13 2019 |
5 Y |
rash , knee pain swelling, |
diet insufficiencies |
vitamin C level low |
non |
non |
yes |
|
Lund et al.2 2019 |
3 Y |
persistent limp |
diet insufficiencies |
microcytic anemia vitamin C level Lowe |
non |
non |
yes |
|
Priyanshi Ritwik et al.14 2019 |
7 Y |
crying, difficulty in eating, and night-time mouth pain. |
autism spec- trum disorde |
microcytic anemia Lowe vitamin C |
non |
non |
yes |
|
Harknett et al.17 (2013) |
9 Y |
Non-weight- bearing, gingivitis, musculoskeletal pain, and swelling |
Autism |
anemia , vitamin D Iron deficiency |
X-ray: normal MRI: multifocal metaphyseal marrow edema and periosteal fluid collection |
Bone biopsy: hemosiderin laden macrophages |
yes |
|
Shahryar Noordin et al.17 (2012) |
4 Y |
pain and swelling of joints for and inability to walk |
Guillian Barre’ Syndrome , diet insufficiencies
|
Low hemoglobin |
X-rays of the knees showed ground glass osteoporosi, (Ring sign) |
noo |
yes |
|
Cole et al.17 (2011) |
10 Y |
Musculoskeletal pain and swelling, gingivitis, non- weight-bearing, rash |
Autism, developmental delay |
anemia |
X-ray: mild diffuse osteoporosis |
Punch biopsy skin: perifollicular hemorrhage
|
yes |
|
Solanki et al.17 (2011) |
10 Y |
Musculoskeletal pain, non-weight- bearing, gingivitis, pallor, hair changes |
Mental retarded developmental delayed, seizure disorder |
Macrocytic anemia |
X-ray: Wimberger ring, Frankel line |
non |
yes |
|
Bacci et al.17 (2010) |
2 Y |
Gingivitis, musculoskeletal pain and swelling |
Extremely permissive parenting style |
Microcytic anemia |
X-ray: normal |
Bone marrow biopsy: normal
|
yes |
|
Besbes et al.17 2010 |
28-month 5 years |
musculoskeletal pain, irritability, fever, and pallor. pain and swelling of the left lower limb, intense pallor, |
psychomotor developmental delay and a seizure disorder poor oral intake |
iron deficiency microcytic hypochromic aregenerative anemia
|
oste- openia; thickened white line at metaphysis osteopenia, an irregular thickened white line at the meta- physis of femur |
non |
yes |
|
Popovich et al.17 (2009) |
1.6 years (plus review of 7 patients aged 1.5-9 years) |
Musculoskeletal pain, gingivitis, rash, non-weight- bearing, pica, pallor, irritability |
Severe food allergies, inadequate finances |
anemia Elevated ESR Low prealbumin Low vitamin C |
X-ray: edema of knee Bone scan: increased uptake at distal femur |
non |
yes |
|
Burk and Molodow17 (2007) |
2 Y |
Irritability, non- weight-bearing, gingivitis, petechiae, bruising |
Boiled milk, barley, and corn syrup diet |
Low vitamin C anemia |
X-ray: scurvy lines, osteopenia, corner sign |
no |
yes |
|
Duggan et al.17 (2007) |
9 Y |
Irritability, non- weight-bearing, gingivitis, rash |
Autism |
Microcytic anemia |
X-ray knee: osteoporosis, periosteal elevations, Frankel sign, scurvy lin |
Bone biopsy: extravasated red cells, edema, early fibrosis Skin biopsy: perifollicular hemorrhage |
yes |
|
Larralde et al.17 (2007) |
8 M |
Gingivitis, hair changes, pseudoparalysis |
Dilute cow’s milk diet |
Anemia |
X-ray: osteopenia, scorbutic rosary, corner sign |
no |
yes |
|
Seung Woo Choi17 2007 |
5 |
swelling of the left thigh, general weakness, poor oral intake, and a mild fever |
cerebral palsy, developmental delay, seizures, poor oral diet |
High WBC vitamin C level was low |
osteopenia, a widened physis, and small beak-l |
pathologic findings revealed an osteonecrosis and inflammation |
yes |
|
Bingham et al.17 (2003) |
16 Y |
Gingivitis, bruising, musculoskeletal pain, and swelling |
Abdominal pain and diarrhea relieved by dietary changes |
Anemia |
X-rays: normal MRI: calf hematoma |
Bone marrow biopsy: normal Skin biopsy: perivascular inflammation and hemorrhage |
yes |
|
Riepe et al.17 (2001) |
1 Y |
Gingival bleeding, pseudoparalysis, musculoskeletal pain and swelling, scorbutic rosary |
Cow milk and oatmeal diet |
Anemia |
CXR: scorbutic rosary, corner sign X-ray knee: osteoporosis, corner sign, Wimberger ring |
no |
yes |
|
MichaelWeinstein17 2001 |
9 Y |
muscu- loskeletal pain, inflammatory gingival disease, and hypertension. |
developmental delay, mild facial dysmorphism, and a seizure disorder |
hypochromic, microcytic anemia |
osteopenia, and a bone scan initially showed increased uptake around the left knee. |
no |
yes |
|
Mimasaka et al.17 (1999) |
6 Y |
Cardiopulmonary arrest, gingivitis, musculoskeletal swelling, stunted growth |
Neglect |
Low vitamin C
|
X-ray: calcified periosteum of epiphysis |
Autopsy: subperiosteal hemorrhage, dislocated epiphyseal plate, foam in airways |
no |
Table 1 Review of all literature started from 1999 to 2023
The present study showed the pharmacological potential of the ethanolic extract of Neem bark. Our findings demonstrated that the F-EtOAc, obtained after saponification of EtCNeem, showed to be rich in phenolic and flavonoid compounds with antioxidant potential, as well as a nontoxic.
None.
The authors declare no conflicts of interest.

©2023 Bo-Eisa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.