MOJ
eISSN: 2374-6939


Review Article Volume 5 Issue 4
1Senior resident orthopedics surgery, King Fahad hospital, Saudi Arabia
2Consultants orthopedics surgery and Oncology, King Fahd medical city, Saudi Arabia
3Medical students, King Fahad Medical City, Saudi Arabia
Correspondence: Munzir Izzeldin Abdelraouf Abbasher, king fahad mdical city, dhabab street, sulaimanya, po.box 59046, zip 11525 Riyadh, SaudiArabia, Tel 967000000000
Received: August 24, 2016 | Published: September 2, 2016
Citation: Abbasher MI, Al-Shaya O, Sawan H, Al-Kenani A, Al-Rumaih M, et al. (2016) Reconstruction of the Ankle after Wide Resection of Distal Fibula Tumours: Case Series and Review of the Literature. MOJ Orthop Rheumatol 5(4): 00189. DOI: 10.15406/mojor.2016.05.00189
The fibula is a rare anatomic location for both primary bone sarcomas and metastatic lesions. The proximal fibula is the most common area of the fibula involved by tumors. This followed by the fibular diaphysis and distal fibula. Resection of the distal fibula is used to treat malignant or benign locally aggressive tumors involving this region. Current reconstructive techniques are limited by undesirable functional deficits. We report 2 cases, all of them having Ewing's sarcoma in the distal fibula. We investigated them systemically and locally by doing X-ray, CT Scan, MRI and Bone scan. We did for them wide resection of tumor .The ruminant of tendons of the peroneus longus, peroneus brevis, and flexor halluces longus were cut and they were used to reconstruct for the lateral aspect of the right and left ankle using suture anchors. K-wires were used to do temporary arthrodesis.
Involvement of the distal part of the fibula by benign aggressive and malignant tumors remains to be a challenge for the treating surgeon. Such lesions require resection that consequently results in ankle instability.1 Due to rarity of the condition reconstruction techniques vary, with variable results. The fibula is affected in 2.4% of primary bone tumors,2 with the proximal third being more frequently involved than the distal segment.2,3 Malignancies of the distal third of the fibula carry a better prognosis than proximal lesions,2 although some authors have not observed such prognostic difference.4
The fibula is longer than the tibia and contributes partially to weight bearing. In 1971, lambert5 using cadaveric ankles reported one sixth of the static load of the leg was carried by the fibula. The embryological aspect of the ankle joint reflects a mild Varus alignment and becomes parallel to the knee joint after 12. In adults the fibula lateral malleolus is located 2cm posteroinferior to the medial malleolus tip, and is mobile up and down during stance phase. The distal projection of the lateral malleolus acts to limit the amount of eversion thus acting as a lateral buttress. The ankle joint is surrounded by fibrous capsule yet it is weak anteriorly and posteriorly. The medial and lateral sides are strengthened by well-defined ligamentous structures i.e. static stabilizers and muscular structures i.e. dynamic stabilizers. The lateral side off the ankle has three major ligamentous structures namely 1)anterior talofibular 2)posterior talofibular 3) calcaneofibular , resection of which during surgery might result in ankle collapse into valgus if not reconstructed.1,6
A girl, 11yearsold Saudi presented to us with progressive swelling of the left lower limb, localized above the left ankle with complaints of pain and limping gait. She had visited many clinics for her pain and swelling with no relief to her symptoms. The patient was examined clinically and there was a swelling in the lateral aspect of the distal leg tender firm too hard with intact skin over it, 4x3 cm, no other systemic clinical finding of note. X-ray of the left leg (Figure 1) showed aggressive lytic lesion of the distal fibula. Thence patient was investigated with basic lab works plus systemic and local staging for further diagnosis. She was admitted under us in pediatric surgical ward for open biopsy of the distal fibular lesion and CT of the lower limb (Figure 2) showed destructive bone lesion involving the distal end of the fibula associated with extensive destruction and aggressive periosteal reaction associated with large soft tissue mass 4.5 x 5 cm in maximum axial dimension. Also, MRI of the lower limb (Figure 3) showed there is a large destructive bone lesion involving the distal diaphysis of the left fibula. This lesion does not cross the growth plate. It is associated with aggressive periosteal reaction along with a large soft tissue mass that appears of high signal intensity in T2 and intermediate to low signal intensity in T1 sequences. This was followed by technetium-99m MDP scintigraphy (Figure 4), it showed an increased tracer uptake in the distal left fibula, extending to the left ankle and the left foot. Excisional biopsy was taken from the proximal and distal margin of the lesion in the left fibula which confirmed Ewing's Sarcoma. According to the histopathology department, they reported that there is no evidence of residual tumor i.e free resection margins. (Figure 5) The patient was referred from us to pediatric oncology clinic for further evaluation. She was electively admitted to the hospital for staging and central line insertion to start chemotherapy. She treated as per Ewing sarcoma protocol in our hospital. Patient was put on neoadjuvant chemotherapy which included vincristine, cyclophosphamide, doxorubicin and etoposide, and if osfamide 3 times weekly. After 6 months of chemotherapy, we recommend to her family to do a surgery. We did a wide surgical resection of the tumor in the left leg. Subcutaneous tissue was dissected and isolation of superficial peroneal nerve was done. Dissection of lateral compartment of the left leg up to 16cm proximal to the lateral malleolus and distally, until the distal physis (Figure 6). The tendons of the peroneus longus, peroneus brevis, and flexor halluces longus were sacrificed and the ruminants were used to reconstruct for the lateral aspect of the left ankle using suture anchors (Figure 7). K-wires were used to do temporary arthrodesis (Figure 8). The surgical wound was closed in layers. VAC dressing was also applied as standard care management in Oncology cases at KFMC and backs lab was applied (Figure 9). The last MRI done for the patient showed there is altered signal intensity of the soft tissue with post-contrast enhancement. However, the dimensions of this area of altered signal intensity are decreased as compared to previous MRI. There is no evidence of soft tissue mass lesion (Figure 10). According to the last patient's follow up after six months post-operation it shows no Valgus deviation, normal ankle motion, mobilizing full weight bearing with splint assistant during physical examination (Figure 11). Also, X-rays and MRI finding shows no residual mass lesion or local recurrence.


Figure 1 AP view of plain X-ray of the left leg showed ill-defined lesion involved distal end of the fibula (diaphysis) with cortical destruction and soft tissues swelling.
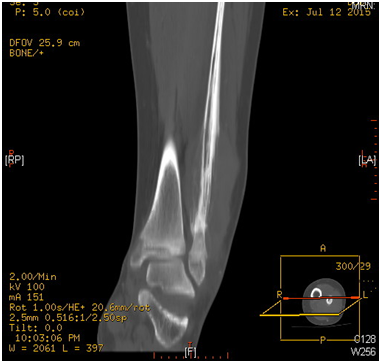
Figure 2 CT Scan of the lower limb showed destructive bone lesion involving the distal end of the fibula.

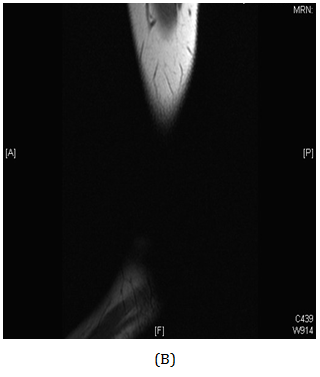
Figure 3 MRI of the lower limb showed aggressive bone lesion involving the distal diaphysis of the left fibula associated with huge soft tissue tumor.
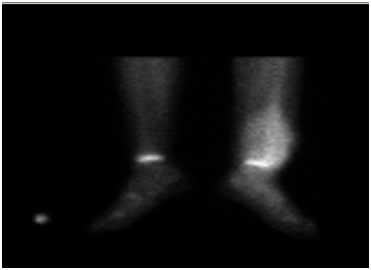
Figure 4 Bone scintigraphy demonstrates an increased tracer uptake in the distal left fibula, extending to the left ankle and the left foot.
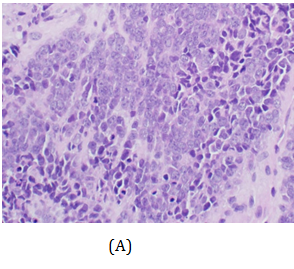
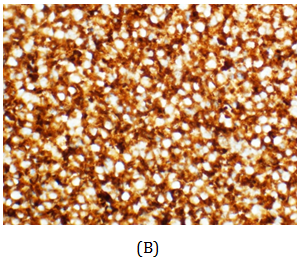
Figure 5 H&E stain and immunohistochemistry showed sheets of small round cells with scant clear cytoplasm , little mitotic figures and multiple fatty cells.
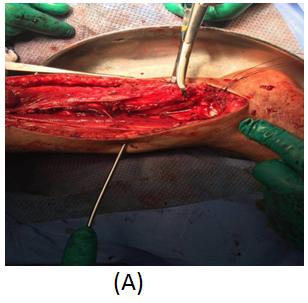

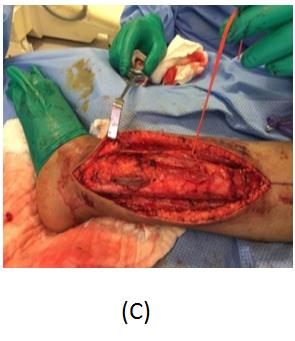

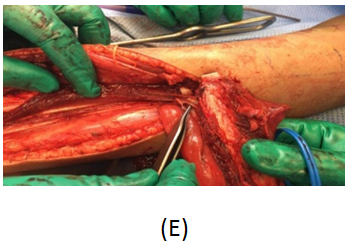
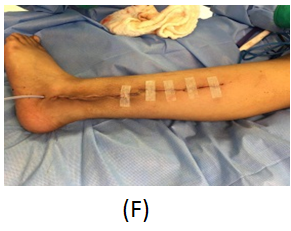

Figure 6 Interoperation images. Tumor in the distal end (A). Remnant of Prenous Longus Tendone (B). Isolation of the Superficial Peroneal Nerve (C). Resection of distal Fibula Tumor (D) Tumor resected with reservation of neurovascular pedicle (E). VAC dressing (F). AP view of plain X-ray of the left leg showed dissection of lateral compartment of the left leg during resection of the tumor (G).


Figure 7 Anteroposterior ( A ) and lateral views ( B ) of plain X-ray of the left leg showed the tendons of the peroneus longus, peroneus brevis ,and flexor hallucis longus were cut and they were used to reconstruct for the lateral aspect of the left ankle using suture anchors.


Figure 9 Anteroposterior (A) and lateral views (B) of Plain X-ray of the left leg after applying a backslab.
A Saudi girl, 10 years old presented to OPD with progressive swelling of the right ankle for 3 months, localized on the lateral aspect, and increasing with pain and swelling within last two months. During physical examination, proximal area of the skin over the swelling was dark black as what was noted. The patient was investigated primarily in a hospital outside of Riyadh according to a biopsy was taken with osteomyelitis of distal fibula and treatment was start taken but with no response. X-ray of the right leg (Figure 12) and CT of the lower limb (Figure 13). An expansile, lytic and destructive bone lesion is seen involving the distal third of the right fibula. (Figure 14) on MRI showed there is a large destructive bone lesion involving the distal third of the right fibula with sparing of the distal fibular epiphysis. No definite involvement of the right tibia and talus. Trace of fluid is seen in the right tibiotalar joint most likely reactive. The neurovascular structures appear intact. This was followed by technetium-99m MDP scintigraphy (Figure 15), what it showed a solitary focal lesion distal end of right fibula compatible with suspected Ewing's sarcoma. No additional lesions were noted to suggest skip lesions or metastasis. She treated as per Ewing sarcoma protocol in our hospital. Patient was put on neoadjuvant chemotherapy. Later, We did a wide surgical resection of the tumor was preformed upto12 cm from the distal fibula malleolus during which ,the superficial peroneal nerve and peroneus longus and brevis tendon were sacrificed the ruminant of the peroneus longus and calcaneo fibular ligament were sutured and using anchors were attached to the distal tibia in the right leg free pedicle latissmuss dorsi flap was anastomosed to the peroneal artery locally to cover the soft tissue defect by the plastic surgery team. The last MRI done for the patient (Figure 16) showed there is interval reduction in the size of the previously noted heterogeneous enhancing mass at the distal metaphysis of the right fibula. On the bone scan (Figure 17), there is interval reduction in the size of the previously noted heterogeneous enhancing mass at the distal metaphysis of the right fibula. There is no sign of skip metastases to other limb. Bilaterally bone marrow signal changes are most likely related to chemotherapy. The patient will follow up with us regularly.

Figure 12 AP view of plain X-ray of the right leg showed ill-defined lesion involved distal end of the fibula (diaphysis) with cortical destruction and soft tissues swelling.

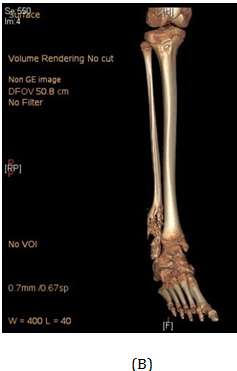
Figure 13 CT Scan of the distal third of the right fibula showed an expansile, lytic and destructive bone lesion.


Figure 14 MRI of the lower limb showed aggressive bone lesion involving the distal diaphysis of the Right fibula associated with huge soft tissue tumor.
Indeed only single case reports or small case series have been published in the subject reflecting the rarity of the condition.
Although some authors had good results without osseous reconstruction and believed that ankle stability was achieved by cicatricle fibrous tissue.7,8
In classic textbooks, reconstruction of the ankle after fibulectomy was done by transportation of the fibula in the same leg where the head of the fibula was used as a lateral malleolus. Classically described by Carell et al.9 technique has been used by Degauzy10 and Herring,11 yet has several shortcomings such as risk off peroneal nerve injury and lateral knee instability and inappropriate articulation with the talus distally12 and risk of arthritis.12 In his two case series one had normal ankle function at 2 years but information regarding knee and ankle function was not reported for one patient.
Dieckman et al.13 in his review, of 11 patients with distal fibula tumors either metastases or sarcomas, has achieved stability after reconstruction by arthrodesis either using a hind foot nail or tibiotalar arthrodesis with screws. The pros of the technique lie within the immediate stability and no need for cast immobilization (if hind foot nail is used), and acts as a salvage if part of the tibia was found to be involved with disease intra operatively. The cons on the other hand lie within the loss of ankle motion and the possibility of contamination and seeding of tumor cells through reaming in his review 2 complications in 2 patients one was super infection ended up with amputation and the other was non-union of the arthrodesis.
Monson et al.,14 in his case series of three patients, he advocated and performed a non-anatomical soft tissue reconstruction off the lateral ankle for stabilization. The technique utilized the peroneus brevis tendon and tenodesing it to the distal part of the tibia, and suturing part of it to the remnants of the calcaneofibular and talofibular ligaments. An average follow up of 4.8yrs revealed no episodes of instability, normal ankle motion and no arthosis. One of the patients had fracture in the base of the 5th metatarsal fracture and another underwent further fibula shortening due to bursa.
Jamshidi et al.15 proposed a way to reconstruct the ankle joint using osteoarticular allograft. In this review of 4 patients distal fibula allografts from the bone bank were used after appropriate standard tissue banking procedures.affter margin free resection adequate length of allograft was utilized and internally fixed using semitubular plate and screws .interestingly union was achieved in al 4 cases yet it is widely known that there is 30% risk of non-union, ankle stability was granted in all patients. As a late complication one patient had ankle valgus and another had syndesmotic screw breakage.
Recently leibner et al.,12 reported a case where they constructed the ankle mortise with the distal fibular remnant -the epiphysis-lateral malleolus to which a bone graft was attached. Stability was granted by arthrodesing distal margin of the fibula to the tibia and stabilized by plate and screws. At 5 years patient was pain free and physically active with no limitations and no instability.
Cappana et al.16 of the Rizzoli Orthopedics Institute in 1986 had a comprehensive review of 11 patients with various types of reconstruction after distal fibular resection; the overall results were satisfactory in this case review.
Overall, the rarity of the condition makes it difficult to choose which technique to be advantageous over the other. A step wise approach would limit and narrow your options and a decision based on several factors should be addressed such as type and nature of the tumor, site ,age of patient, involvement of growth plate, invasion of surrounding soft tissues (e.g. peroneus tendons), and the need for post-operative radiotherapy and chemotherapy should be considered.
Based on these options of treatment could be discussed as follows:
In the recent review by Leibener et al.,12 7 key points should be addresses when indulging into distal fibula reconstruction after resection:
None.
None.

©2016 Abbasher, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.