MOJ
eISSN: 2374-6939


Case Report Volume 2 Issue 6
Pulvertaft Hand Centre, UK
Correspondence: Tommy R Lindau, Consultant Hand Surgeon, Past President European Wrist, Arthroscopy Society (EWAS), The Pulvertaft Hand Centre, Kings Treatment Centre, Royal Derby Hospital, Uttoxeter Road, DE22 3NE, Derby, UK, Tel 00441332783389
Received: June 16, 2015 | Published: June 22, 2015
Citation: Lindau T, Mathew P. Radial artery pseudoaneurysm in trapezio-meta-carpal arthroscopy: a case report, a cadaveric study and a systematic review of the literature regarding complications. MOJ Orthop Rheumatol. 2015;2(6):220-223. DOI: 10.15406/mojor.2015.02.00075
Arthroscopy of the trapezio-meta-carpal (TMC) or carpo-meta-carpal (CMC I) joint of the thumb is gaining popularity in the management algorithm for treatment of disorders related to the joint. We present an unusual and previously unreported complication of a pseudoaneurysm of the radial artery following this procedure. With a subsequent study on cadavers, we further discuss the portals and techniques to reduce the risk of this and other complications also based on a systematic review of the literature.
Keywords: Arthroscopy, Osteoarthritis, TMC
CMC, Carpo-Meta-Carpal; TMC, Trapezio-Meta-Carpal; OA, Osteoarthritis; USS, Ultrasound Scan; STT, Scapho-Trapezio-Trapezoid; DRL, Dorsoradial Ligament; UCL, Ulnar Collateral Ligament; POL, Posterior Oblique Ligament; AOL, Anterior Oblique Ligament; DCL, Dorsal Central Ligament; APL, Abductor Pollicis Longus; FCR, Flexor Carpi Radialis
A 68 year old retired personal assistant presented with pain over the base of her right thumb. Clinical examination and radiography confirmed Eaton Grade II osteoarthritis of the trapezio-meta-carpal (TMC) or the carpo-meta-carpal (CMC I) joint of the thumb (Figure 1). She was initially treated with splinting and two steroid injections to the joint under fluoroscopic control.
Due to lack of sustained pain relief she represented and was offered an arthroscopic evaluation of the TMC-joint. Under regional block anaesthesia and tourniquet the thumb was prepared for arthroscopy. Image intensifier was used to introduce needles into the joint as marked for the 1U and 1R1,2 (Figure 2). The 1U portal at the ulnar aspect of the EPB (Extensor Pollicis Brevis) and the 1R portal palmar to the APL (Abductor Pollicis Longus).1,2 The thumb was then positioned in a traction tower with counter weight. Mini incisions through the skin were made over the needles and artery clips were used for blunt access into the joint. The 1U port was used as the initial viewing portal and the 1R as the initial working portal. A 1.9 mm 30 degree arthroscope was used. A partial synovectomy was done with a 2mm full radius shaver through these portals with use of both portals as combined viewing and working portals. In addition to the partial synovectomy, two loose bodies were found and removed. Furthermore, the Grade 2 OA on x-ray was found on arthroscopic assessment with bare subchondral bone devoid of cartilage (Outer bride Grade IV) on the base of the first metacarpal though the trapezial surface looked more intact.3 At the end of the procedure, the wounds were opposed with steri-strips and the patient was discharged with a light bandage and advised to return in two weeks for a wound check.
At the two-week review, it was noted that there was a pulsatile swelling at the 1U portal. An ultrasound scan (USS) confirmed the clinical suspicion of a pseudoaneurysm (Figure 3). After due counselling she was admitted and had a successful coil embolisation of the radial artery just proximal to its termination by the interventional vascular radiologist (Figures 4 & 5). At further review, a repeat USS confirmed that the pseudoaneurysm had completely clotted off. However at clinical review three months later it was felt that though the swelling had reduced, the thumb base was still painful. After due discussion the patient was offered and accepted the option of trapeziectomy and APL interposition arthroplasty procedure combined with exploration of the pseudoaneurysm.
At surgery, the embolisation coils were visible and the pseudoaneurysm had resolved and flattened into a scarred vessel. This was carefully dissected and mobilised, but not excised, to allow the trapeziectomy to be done safely. In addition to the radiographic Grade 2 OA and arthroscopic findings of bare bone, there were signs of loss of cartilage over the scapho-trapezio-trapezoid (STT) articulation (Figure 6); hence a sliver of the proximal trapezoid was also excised.
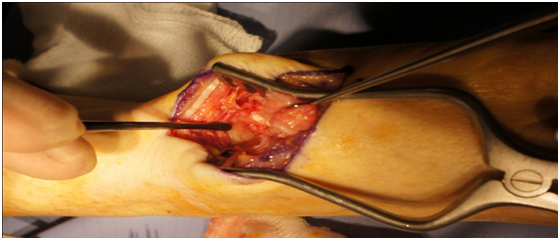
Figure 6 Intraoperative photograph demonstrating the Scapho-trapezoid joint with previously unknown arthritis (indicated with instrument on the left).
At the last follow-up, she is pain free and mobilising her thumb without discomfort. Our systematic review search (please see separate subheading) did not identify any reports of a pseudoaneurysm of the radial artery following arthroscopy of the TMC-joint of the thumb.
Vascular anatomy of the radial artery
The radial artery reaches the dorsum of the wrist from the volar aspect traversing beneath the APL and EPB tendons over the STT-joint. The branches at this level include the dorsal carpal branch, which arises beneath the extensor tendons of the thumb; crossing the carpus transversely toward the medial/ulnar border of the hand, the first dorsal metacarpal arises just before the radial artery passes between the two heads of the first dorsal interosseous muscle and divides almost immediately into two branches, which supply the adjacent sides of the thumb and index finger; the first branch being the arteria princeps pollicis and the second branch; arteria volaris indicis radialis (radialis indicis artery).
Cadaveric assessment of the radial artery
In order to further define a safe zone (with respect to the artery) for the ulnar portal, we dissected 5 fresh-frozen cadaveric hands and exposed the radial artery alongside the clinically identifiable landmarks at the level of the TMC-joint and measured the distance from the edge of the tendons to the artery. The handling of human remains adhered to ethical and practical protocols. In all five specimens (Table 1) the radial artery was consistently found to be at a distance of 10mm or more from the ulnar edge of the EPB-tendon.
|
Name |
Distance in mm |
|
Patient 1 |
|
|
Patient 1 EPB |
12 |
|
Patient 1 EPL |
4 |
|
Patient 2 |
|
|
Patient 2 EPB |
10 |
|
Patient 2 EPL |
4 |
|
Patient 3 |
|
|
Patient 3 EPB |
10 |
|
Patient 3 EPL |
3 |
|
Patient 4 |
|
|
Patient 4 EPB |
12 |
|
Patient 4 EPL |
3 |
|
Patient 5 |
|
|
Patient 5 EPB |
12 |
|
Patient 5 EPL |
0 |
Table 1 Summary of cadaveric study findings: The distance from the EPB and EPL respectively to the radial artery is shown in the table.
The position with respect to the EPL tendon was more variable ranging from 0mm (under the tendon) to 7mm radial to the radial edge of the tendon. The superficial branch of the radial nerve course was variable in each of the specimens and did not directly cross the portals. Our cadaveric findings adhere to the common understanding that the radial artery crosses deep to the extensor tendons and is located about 4 to 17 mm (average 11mm) ulnar to the EPB tendon and about 2-8 mm radial to the EPL tendon at the level of the TMC-joint.4
Systematic review of the literature
We searched the following databases:
The following search terms were used without setting any limits
exp *RADIAL ARTERY/ exp ANEURYSM, FALSE/ exp CARPOMETACARPAL JOINTS/ OR exp THUMB/ exp TRAPEZIUM BONE/ exp ARTHROSCOPY/ "radial artery".ti,ab/ ("pseudoaneurysm" OR "false aneurysm").ti,ab/ (trapezioemetacarpal OR carpometacarpal OR CMC OR thumbTitle/Abstract)/ radial artery Title/Abstract
The systematic review did not reveal any previous reports regarding the post-operative development of a pseudo-aneurysm, even if arterial injuries with haematoma formation were described.2,5 The review identified numerous complications associated with arthroscopy to the CMC I joint; ranging from superficial and deep infections to injury to the branches of the superficial radial nerve, and persistent post-operative pain.2,5 There is however paucity in the literature as demonstrated in our review regarding the true incidence of the complications and on specific advise regarding how to avoid them.
Our case illustrates the problem with establishing portals safely; one of the key features with arthroscopy in any joint. We have previously not experienced any problems with the 1R and 1U portals used in this case.1,2 However, the proximity of the 1U portal to the radial artery increases the risk of damaging the artery, either completely or as in our case with a tangential damage and development of a pseudoaneurysm. Adhering to the described safe zones and following a regimented sequence of surgical techniques may help prevent avoidable complications. We have therefore suggested some pearls and pitfalls (Table 2). A false or pseudo- aneurysm6 is a fibrous containment of arterial contents after the arterial wall has been disrupted. In other parts of the body it may be a deadly complication, whereas it is less likely to cause any severe problems at this part of the hand and wrist.
|
|
Pearls |
Pitfalls |
|
1 |
Insert 2 blue needles in the 1R and 1U portals to the TMC-joint under fluoroscopic guidance. Exsanguinate prior to this to prevent displacement of needles. |
Failure to safely identify the portals may cause unnecessary soft-tissue injuries. |
|
2 |
Keep the 1U portal within 10 mm of the ulnar border of EPB. Mark this tendon prior to anaesthetic block. |
Further ulnar placement of the needle risks injury to the radial artery |
Table 2
A combination of color Doppler ultrasonography and X-ray angiography has been conventionally used with a sensitivity of 94% and specificity of 97% reported for the former modality (Figure 3). The classic appearance seen on color ultrasonographic imaging reveals a ‘‘Pyongyang’’ sign of swirling blood within the false aneurysm. X-ray angiography reveals a saccular aneurysm with a narrow ostium connecting the arterial lumen with the sac.
Treatment options involve surgical exploration and ligation or direct repair with or without grafting, ultrasound guided external compression of the neck of the false aneurysm, endovascular procedures like occlusion by coils, exclusion by stent-grafts and trans arterial or percutaneous injection of thrombin (bovine/human) to occlude the false aneurysm.
Our case with a complication with a pseudo-aneurysm occurred due to a very minimal but too ulnar placement of the 1U portal. Fortunately, it was successfully managed by the interventional radiologist with occlusion by coils (Figure 5). The patient did, however require further operative treatment due to persistent pain at the base of the thumb, independent on the arthroscopic iatrogenic complication. Interestingly, there was previously unknown OA at the STT-joint found at open surgery, possibly being the main cause of remaining pain after two steroid injections and arthroscopy and debridement to the more distal TMC-joint. So, perhaps in hindsight, CMC I arthroscopy ought to be combined with STT arthroscopy due to the risk of a pan-arthrosis presentation in spite of a seemingly normal preoperative x-ray.
Arthroscopic evaluation and treatment of the trapezio-meta-carpal (TMC) or carpo-meta-carpal (CMC) joint of the thumb is indicated in patients with early stages of osteoarthritis (OA) who have failed non-operative management. This includes synovectomy, debridement, removal of loose bodies, but may also involve thermal shrinkage and partial trapeziectomy with or without interposition. We have routinely used the portals as described by Badia A & Berger RA1,2 with the 1-U (ulnar) portal being made just ulnar to the EPB-tendon and the 1-R (radial) portal, volar/radial to the APL tendon. This case was of course the same, yet with a previously not reported complication.
The plane of the 1-R portal passes through the non-ligamentous capsule just lateral to the anterior oblique ligament (AOL) and is the preferred portal from which to view the dorsoradial ligament (DRL), posterior oblique ligament (POL), and ulnar collateral ligament (UCL), though the DRL may not always be clearly visualized as it is directly ulnar to the portal.7 The plane of the 1-U portal passes between the dorsal central ligament (DCL) and POL7 and is the preferred portal from which to view the AOL and UCL. Arthroscopic debridement and tendon interposition was described nearly 17 years ago.8 Two portals were described to permit adequate visualization and triangulation for debridement and tendon passage, one radial to the abductor pollicis longus (APL) tendon (volar), and one ulnar (dorsal) to the APL tendon along the line of the joint. The distance between each portal and insertion of APL is about 1 cm.
An accessory dorsal-distal portal (D-2) was developed to improve the visualization of the ulnar aspect of the trapezium if an arthroscopic trapeziectomy is contemplated.9 This portal is ulnar to the EPL-tendon and 1 cm distal to the V-shaped cleft at the juncture of the index and thumb metacarpal bases. A separate thenar portal, just distal to the oblique ridge of the trapezium following a line referencing the radial edge of the flexor carpi radialis (FCR) tendon has also been introduced.9 The multitude of portals make it difficult to understand which one is the best as they are all described and used by experts in a safe way, however, we suspect that there is an under-reported issue with portals and subsequent complications.
A thorough knowledge of the anatomy is essential to avoiding iatrogenic complications when embarking on arthroscopy in any joint of the body. Though rare, our reported complication with a pseudo-aneurysm of the radial artery, as well as other complications, are true learning points and should be reported to increase awareness among surgeons who perform these procedures be it routinely or occasionally. We sincerely hope this case report with the additional cadaveric assessment and systematic review of the literature will help not only novices in the field, but also aid experts in order to further excel in CMC I arthroscopy.
None.
None.

©2015 Lindau, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.