MOJ
eISSN: 2374-6939


Review Article Volume 11 Issue 1
Argentina
Correspondence: Rodolfo Horacio Alonso, Lobos 249, Wilde, Buenos Aires, Código Postal: 1875, Argentina
Received: July 15, 2017 | Published: January 31, 2019
Citation: Alonso RH. Posterior cruciate ligament. cortical tibial fixation. MOJ Orthop Rheumatol. 2019;11(1):35-40. DOI: 10.15406/mojor.2019.11.00466
The difficulties of the techniques of reconstruction of de Posterior Cruciate Ligament (PCL) are widely known.
Objectives: To present our technique of retrograde tibial fixing, and analyze retrospectively if we have improved the final result.
Material and Method: In a group of 110 surgical patients for PCL operated with different techniques we did a retrospective study in 96 with X-ray posterior drawer when they returned to work. 14 patients were excluded because they did not meet those conditions.
Results: The X-ray posterior drawer test had differences statistically significant between our technique and the previous ones, which were done with bone-patellar tendon- bone and quadrupled hamstrings fixed with screws.
Conclusion: Our technique has simplified the surgery; its duration was shortened and therefore allows us to do other simultaneous ligament reconstructions. It has improved the posterior drawer test objectively.
Keywords: PCL, Cortical Tibial Fixation
Level III. Retrospective comparative study.
PCL reconstruction is demanding, with different techniques available. First Bone-Tendon-Bone graft (BTB)1–7 was chosen, with important technical difficulties such as sometimes short graft length, because at the moment to turn and introduce one of the bone parts into the femoral tunnel from distal to proximal, the other bone part got out from the tibial tunnel and it was very difficult to get it reintroduced.. Another difficulty was to control the location of the screw at the end of the tibial tunnel. Then Quadrupled Hamstrings (QH) graft8–22 was used, fixed with screws, with which the technique was much easier, the length of the graft was enough (with the need even to place a screw in the depth of the tibial tunnel) and because of its flexibility there was not difficulty in introduction it into the femoral tunnel.
With these first two techniques after the surgery the knee had no clinical PDT, but when the immobilization with the splint was removed after 8 weeks a clinical PDT was evident, and then at the medical discharge the radiographic PDT was greater than 5 mm, exceeding the average in medical publications. There were two surgeries not included in this study, with Quadricipital graft,23–25 and because of its length it was necessary to fix the bone plug into the depth of the tibial tunnel (same problem as with BTB), and with a little thickness at the end of the graft to fix it inside the femoral tunnel with equal outcome at discharge, the presence of greater than 5 mm PDT (7.5 mm average).
At that point, it was thought that the final result was caused by fault in the tibial fixation, and then it was decided to use a device to hang in a stirrup the HG and attach it to the tibial cortical in the retrograde form (which in addition gave the benefit of not having to control the position of a tibial screw). Two devices were used, designed to suspend tendons in the femur to ACL reconstruction (as an Endobutton), first SAR Bone, rigid and long only up to 20 mm (Figure 1), and when its production was discontinued E-SOLID was used, which because it has a longer and articulated stirrup, is best directed along the tibial tunnel (Figure 2).

Figure 2 E-SOLID device: with stirrup to hang tendons and articulated bracket to lock at the cortical.
At that time also vision optics or instrumental via the posterior-inner passage was left aside for every surgery. Instead anterior approach was used. The aim is to present a new technique for PCL reconstruction. And to analyze retrospectively the result obtained with techniques previously employed and the technique which is showed, to lower the PDT after the patient discharge.
110 reconstructions were done from May 1996 to December 2014.
Inclusion criteria: patients presenting ruptures type III (more than 10 mm of PDT), or type II (between 5 and 10 mm in PDT with symptoms that prevented their return to work), isolated or combined, and were assessed at the time of registration for return to work using radiographic PDT measured in mm.
The PDT was measured in mm with natural size Rx superimposing the Rx of the operated knee and the contralateral (Figure 3&4).
Figure 3 PDT Rx of the operated knee at discharge. E Solid device. The correct location of the tibial tunnel without use of posterior internal approach can be seen..
Technique: 1) Knee in 90º. Vertical incision medial at the Anterior Tibial Tubercle (ATT) to take out the Hamstrings Graft. As assistant prepares the QH passing the Hamstrings through the device bracket and suturing them to themselves (Figure 5). The tourniquet is inflated.
2) Arthroscopy by anterior-lateral approach, meniscal surgery if required. Cleaning of remains of PCL in femur and tibia, seeing and touching the end of the posterior slope, (Usually it is necessary to temporarily exchange the optic to medial and the instruments to lateral).
3) The optic by anterior lateral approach better locates us in the knee than the posterior medial, since it is the way that the arthroscopy is usually performed, and gives more security since the posterior capsule is permanently seen, which is favored by tibial posterior translation because of the relaxed ACL. By anterior-medial approach on the edge of the posterior tibial slope a special guide for PCL with safety device which does not allow the pin to go beyond the tip of the Guide is set (Figure 6A&B), the guide is regulated to lay it in the tibial cortical most distal possible position to avoid interference with a possible tunnel of ACL reconstruction. The pin is inserted with puncher until it stops and soft hammer blows complete the passage through the cortex. A protector cap is placed over the pin, and tunnel is done with bit 1 mm grater that the graft diameter). The tunnel is compacted with device of equal diameter, and with adequate scraper the joint tunnel mouth is rounded to prevent ruptures of the graft in the angle.

Figure 6(A) Special PCL tibial Guide. It has a stop that regardless of the length of the tunnel prevents the pin from passing the tip of the Guide avoiding nerve and vascular injuries.
4) With the same guide a pin is placed in the femoral condyle in an out in way, so that it gets out intra-articular 5 mm from the osseous-cartilaginous limit in the original insertion of the anterior-lateral fasciculus at time 1.30 for the right knee and 10.30 for the left (Figure 7). A protector cup is again placed so that the bit will not damage structures, and a tunnel outside inside, according to graft diameter is done. A compactor is passed, and the intra-articular mouth is scrapped. (If the ACL is also broken, at this time the proper tunnels are done with appropriate guidelines).

Figure 6(B) Vision of the tip of the tibial guide behind the rear slope with optics via anterior lateral.

Figure 7 Location of the pin for the femoral tunnel passed outside inside with the same tibial Guide.
5) A double wire is passed in tibia outside inside, it is led with the tracer until the intra-articular hole of the femoral tunnel where it is fished with a hook outside (Figure 8 A&B). Another double wire on the outside of the knee is engaged, and is carried distally (femoral tunnel - intra-articular - tibial tunnel), the loop remaining out of the tibial hole.
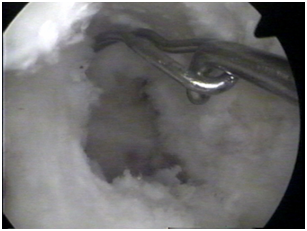
Figure 8(A) Passage of the first wire by the tibial tunnel outside inside, driven by the tracer to be presented against the femoral tunnel.
6) Through the wire loop tractor threads are passed, the graft is raised distal to proximal to the outside of the inner condyle (Figure 9 A&B), until the tibial device gets locked in the cortical.

Figure 8(B) In the intra-articular mouth of the femoral tunnel the first wire is engaged with a hook and carried out to have it passed along the path of the PCL with the loop outside of the femur.
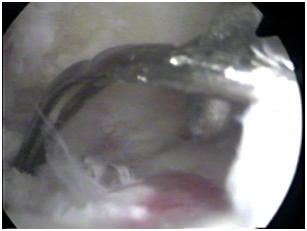
Figure 9(A) Once the second wire is hooked to the first, out of the femoral tunnel, it is carried to distal so it rests with its loop on the outside of the tibial tunnel.

Figure 9(B) By the second wire bending graft threads are passed to subsequently raise it through tibial and femoral tunnels.
7) Maneuver of tightening is done: while assistant pulls the graft strongly, the surgeon with one forearm behind the leg performs anterior drawers, and with the other hand on the ankle carries out knee flexion-extensions several times (Figure 10), so that the graft further progresses within the tunnels.
8) Screw guide is passed into femoral tunnel so that that it does not penetrate the graft and is left between it and the wall of the tunnel in order not to block the screw. Knee in 70ª and under maximum stress (anterior drawer with forearm behind the leg), the assistant places tendon osseous interference screw of the diameter of the tunnel outside inside, leaving the system as shown in Figure 11 and radiographic controls Figure 12. The stability is checked in flexion and extension. In case of rupture of both Cruciates, after passing the PCL graft, the BTB graft is introduced and fixed in ACL femur tunnel, then in 70 degrees of flexion and reduction of step off, the PCL graft is fixed in femur with a screw out in, and so is the ACL graft in 70º in tibia, according to Fanelli recommendation35. If there is also a collateral ligament injury, the hemostatic device is released and the collateral ligament is repaired without having to re-inflate it.

Figure 10 Once the graft is hoisted, while the assistant pulls it, the surgeon makes maneuver of tension: with a forearm behind the leg doing strong anterior drawer and with the other hand doing knee flexion-extensions numerous times.

Figure 11 Drawing of the system with graft fixed in tibia with Sar Bone and in femur with interference screw, from outside to inside.
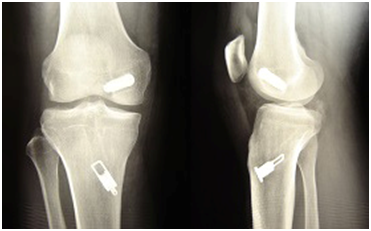
Figure 12 Postoperative Rx control, with E Solid, showing again that the tibial tunnel is correctly located without the need to use posterior internal approach.
9) Inguinal malleolar brace fixed in knee extension with back leg discharge to relax the LCP for 4 weeks, then progressive mobility, support with crutches at week six, removal of splint at week eight, progressive removal of crutches according to muscle strength and plan of rehabilitation for 2 to 3 more months.
With this technique SAR-Bone device was used in 53 knees (Figure 1 & 5). Due to discontinuity in the production of the Sar Bone, the E Solid device was used in the following 16 surgeries (Figure 2 & 12).
Over 110 PCL surgeries 96 reconstructions (92 men and 4 women) were included, with average age 33.6 years (range 17 to 55 years), and 12 patients who had not been discharged, or were lost during the treatment were excluded. The result in the first surgeries with different techniques was:
First group: BTB graft fixed with two interference screws1–7 consists of 13 patients with average age 33.4 years (range 17 to 52 years), with Rx PDT at discharge of 8.08 mm. (range 7 to 11 mm).
Second group: QH graft8–24 fixed with interference screws in femur and tibia, in some cases plus staple tibial, in 4 cases double fascicle, consists of 14 patients (1 female) with average age 31.7 years (range 22 to 44 years) with Rx PDT at discharge of 8.07 mm. (range 3-11 mm).
Third group: Two types of devices that are attached to the tibial cortical and have a stirrup from which hangs a QH graft folded over itself were used. This last group includes 69 patients, 66 men and 3 women with average age 34.2 years (range 19 to 55 years) with an Rx PDT at discharge of 4 mm (range 0 to 14 mm).
Since July 2004 with this technique significantly reduction of PDT at discharge has been achieved, with an average within the grade I (0-5 mm), similar to other publications.
In the statistical analysis, the variable PDT does not present a normal distribution so the non-parametric test of Kruskal Wallis was used, and significant differences were found. To compare pairs to groups the Mann-Whitney test was used, and because multiple comparisons were made, the Bonferroni correction was used to handle the error of type 1. No significant differences were found between first and second groups treatments (Pv=0, 430), but by comparing each of the first two with the technique of retrograde cortical tibial fixation, significant differences were found (Pv < 0.001) (Table 1).
In patients with work-related injuries subjective tests are unreliable, and patients are lost to long term follow-up, therefore to evaluate the final results with the new technique at discharge Rx PDT measured in mm25–28 has been used. The results in the two first groups of surgeries was: in 13 patients using BTB graft fixed with two interference screws the Rx PDT was 8.08 mm at discharge, and in 14 reconstructions with QH graft, fixed with interference screws, in some cases plus staple tibial, in 4 cases double fascicle, the Rx PDT was 8.07 mm at discharge.
It was thought that because the tibial tunnel was locked distal in the cortical where the mineral bone density is minor, it caused the loss of fixation obtained at the end of the surgical procedure29–33 and so two devices that allowed to suspend QH grafts of a Stirrup were used successively. Also the difficulties to see the final position of the tibial screw at the bottom of a long tunnel were solved simultaneously, avoiding the introduction of the optic into the tibial tunnel to view the screw position or Rx controls in case of doubt, (once in a BTB reconstruction a screw was surpassing the posterior tibial cortical in half of its length, without vascular or nervous complications). In cases of rupture of both cruciate ligaments34–36 after seeing through the anterior-lateral approach the posterior slope with the PCL insertion, reconstruction of both ligaments began without doing posterior internal approach. Then in cases of PCL ruptures isolated, favored by ACL laxity, relaxed by the back subluxated tibia, it was possible to see and clean the rear slope, see the tibial Guide and locate the wire Guide at the angle where the pending ends, with the lens via anterior lateral side and the instrumental anterior medial. Since then the accessory posterior-medial approach has not been used in our surgeries. We would like to emphasize that there is no consensus on the exact location of the tibial tunnel, and that small variations in anterior-posterior position do not alter the final result.37
In 69 patients, treated with the technique in which graft was fixed in cortical tibial and in femur with interference screw, Rx PDT at the discharge was 4 mm. Although at the end of surgery the knee was stable, at the patient discharge a satisfactory PDT less than 5 mm, similar to results in published techniques for PCL had not been achieved. Fixing the graft to the tibial cortical, an immovable and rigid fixation was achieved. The possibility to pull directly from the proximal graft made it possible to tighten it further, avoiding forcing the tibia backwards in the placement of staples or screws when the final fixing is tibial, all of which has contributed to stability at discharge within Group I from 0 to 5 mm. Tibial cortical fixation also freed from doubts a tibial screw position.
On the other hand avoiding posterior internal approach, has also helped to shorten the operating time by 50%, so we can currently do this surgery by inflating the hemostatic device once, and to do at the same time reconstruction of the ACL and/or Collateral Ligaments if necessary. It is debatable whether the results of the technical inlay38–41 are better. This could be because of strong tibial fixation, or because having a single tunnel produces less friction and tightens more graft, but our technique is simpler and does not require the opening of the popliteal area. The weak points of this presentation are that only subsequent Rx PDT have been compared, that the measurements were not made by an independent observer, and the short follow-up of patients, only until discharge.
The reconstruction of the PCL with the described technique has improved radiographic final PDT which was the stated objective and has simplified the surgery, shortening the duration of the procedure, and allowing simultaneous ligament reconstructions.
None.

©2019 Alonso. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.