MOJ
eISSN: 2374-6939


Case Report Volume 3 Issue 3
University of Miami Miller School of Medicine, USA
Correspondence: Jonathan R, University of Miami Miller School of Medicine, 1400 NW 12 Avenue Miami, FL 33136, USA, Tel 305-720-7212
Received: July 01, 2015 | Published: September 10, 2015
Citation: Cerminara AJ, Silva O, Gottlieb JR (2015) Percutaneous Balloon Cementoplasty for Treatment of Bilateral Osteonecrosis of the Humeral Head. MOJ Orthop Rheumatol 3(3): 00094. DOI: 10.15406/mojor.2015.03.00094
Osteonecrosis of the humeral head occurs at a rate lower than in the hip, however, it can result in considerable morbidity. Left untreated, most cases result in subchondral collapse and eventual arthrosis of the glenohumeral joint.1 Risk factors associated with osteonecrosis include alcohol abuse, corticosteroid use, chemotherapy and other less common processes.2 The treatment for pre collapse osteonecrosis includes pharmacologics, core decompression, and bone grafting.3 Hemiarthroplasty and total shoulder arthroplasty are reserved for Ficat stage IV and V disease respectively.4
Percutaneous cementoplasty has been used for a variety of conditions including vertebral compression fractures, painful bone metastases, and avascular necrosis.5 Recent data from a randomized controlled trial of kyphoplasty versus medical management have shown that this procedure outperforms medical management in regards to pain relief and patient mobilization.6 Cementoplasty performed for osteonecrosis of the femoral head has been shown to temporarily relieve pain and improve function, however, it did not prevent eventual total hip arthroplasty in one retrospective study.7
We present a unique case in which a patient with severe pain due to bilateral osteonecrosis of the humeral heads, and a limited lifespan secondary to metastatic breast carcinoma, was treated with percutaneous balloon cementoplasty of the humeral heads. To our knowledge this treatment has not been reported in the literature. The patient gave informed consent to use this case in a case report, and understood that no identifying information would be used.
Keywords: osteonecrosis, percutaneous balloon cementoplasty, humeral head, shoulder pain
The patient is a 42 year old female with metastatic breast carcinoma with progressive metastatic brain disease requiring prolonged corticosteroid therapy. Her chief complaint was bilateral aching shoulder pain. Past history was also positive for diabetes mellitus, anemia, radical mastectomy, and gamma knife surgery for brain metastases. Medications included decadron, lamotrigine, oxycodone, fentanyl patch, clonazepam, and lorazepam.
On physical exam, the patient was a pleasant female in moderate distress due to pain and had obvious Cushingoid features. The right shoulder was diffusely tender about the area of the humeral head. Active and passive range of motion was 90 degrees of abduction and forward flexion. All motion in the right shoulder was painful. The left shoulder was tender about the humeral head. She had essentially no active or passive range of motion of the shoulder due to pain and contractures.
Radiographs revealed osteonecrosis of both humeral heads (Figure 1 & 2) with subchondral collapse bilaterally and mild arthrosis of the left glenohumeral joint. She had seen several orthopaedic surgeons regarding her severely disabling shoulder pain. It was determined that due to progressive CNS metastatic disease and recent hospitalization for gastrointestinal bleeding requiring transfusion that this patient was at unacceptably high risk for an arthroplasty procedure. Non operative therapy, including multiple opiate based pain medications, had failed to improve her quality of life so a less risky treatment was sought.
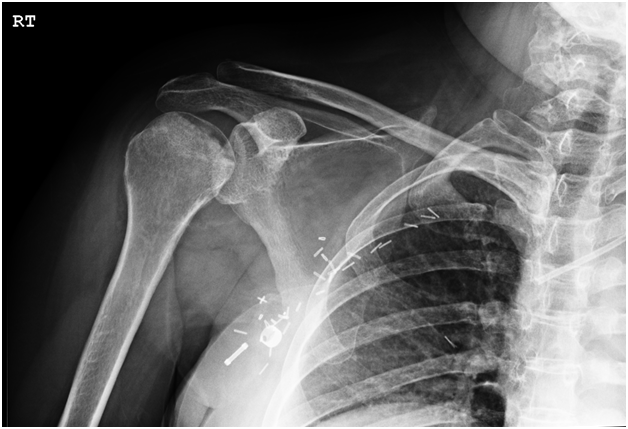
Figure 1 AP radiograph of the right shoulder. There is sclerosis of the humeral head as well as subchondral collapse present. There is osteophyte formation at the inferior humeral articular surface as well as the inferior glenoid.

Figure 2 AP radiograph of the left shoulder showing sclerosis and subchondral collapse of the humeral head, and no degenerative changes of the glenoid.
The patient was offered a percutaneous balloon cementoplasty procedure to treat her osteonecrosis palliatively as a less invasive alternative to an arthroplasty. The patient understood that this indication was not FDA approved, but was based on the success that kyphoplasty has shown in treating vertebral compression fractures. She willingly consented to the procedure. She was placed supine on the operating table and under fluoroscopic guidance a Jamshidi needle was advanced into the humeral head. A guide wire was then placed followed by a Kyphon trochar. A drill was advanced to within 2mm of the subchondral collapse and a Kyphon balloon was placed. The pressure was elevated to approximately 300cc of mercury. The balloon was then removed and 7.5mL of cement was injected into the humeral head (Figure 3). The procedure was repeated on the left side in which 7mL of cement was injected (Figure 4). The patient was successfully extubated and in stable condition following the procedure. The patient was intubated for less than 2 hours in total and was able to be dischared the same day.
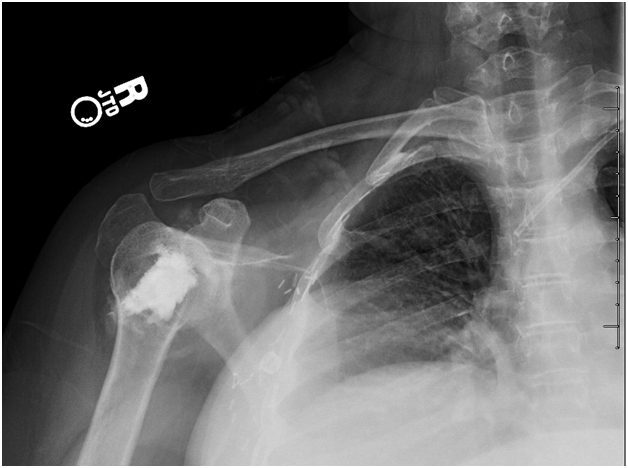
Figure 3 Post cementoplasty right shoulder radiograph revealing cement filling the void created by the kyphoplasty balloon. Assessment of the articular surface is difficult in this radiograph due to the angle of the beam.
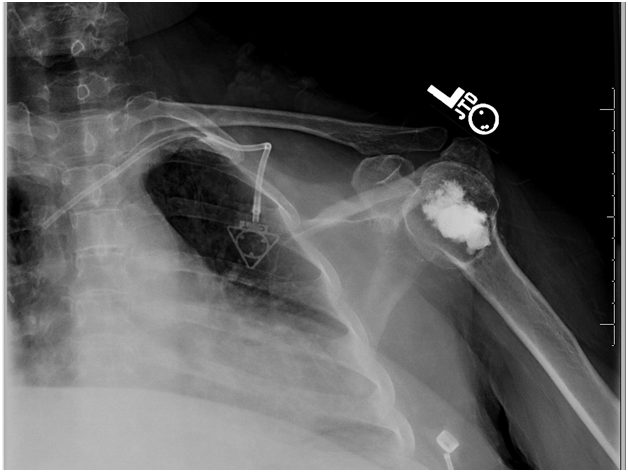
Figure 4 Post cementoplasty radiograph of the left shoulder revealing cement in place in the humeral head.
At one month the patient was seen in the office and stated that the pain in her left shoulder was essentially absent while the pain in the right shoulder was approximately 50% improved. Physical exam was significant for active painless abduction of the right shoulder to 90 degrees and painless passive abduction of the left shoulder to 90 degrees. By 2 months post-operative, pain had completely resolved and this was sustained for the remainder of her life.
Osteonecrosis of the humeral head is a debilitating condition; however, there are several treatments which have shown to be effective in the literature depending on the stage of disease. Arthroplasty would be the most appropriate treatment to consider in this case. Core decompression alone would not address the subchondral collapse and arthrosis. In addition, the poor medical condition of the patient would not allow us to safely perform an arthroplasty.
It has been shown that Ficat stage I and II disease of the shoulder can be treated effectively by core decompression. LaPorte et al.8 reported that 15 of 16 patients with stage I disease, and 15 of 17 patients with stage II disease had a successful outcome using core decompression at a mean follow up time of 10 years.8 In stage III disease, LaPorte et al.8 reported success in only 16 of 23 patients however. Mont9 reported poor results in 5 of 6 patients with stage IV disease treated with core decompression. The above patient had stage IV disease which would likely not have benefitted from a core decompression procedure.
The generally accepted treatment for stage IV disease is shoulder arthroplasty which has shown to result in improved or satisfactory results in several studies.3 In a study by Hettrich et al.10 osteonecrosis was found to be an independent favorable preoperative predictor of good outcome, with results better than in patients with rheumatoid arthritis, and cuff tear arthropathy.10 This would have been the best treatment for the above patient if she did not have such an unacceptably high surgical risk.
The work of Reuter et al.7 showed that cementoplasty for treatment of osteonecrosis of the femoral head reduced pain by more than 80% in two thirds of patients. This pain relief lasted only a mean of 8.1 months however, and 74.5% of patients in that series progressed to total hip arthroplasty at a mean of 19.9 months. It is possible that the results of cementoplasty may more durable in the setting of osteonecrosis of the humeral head because the shoulder is not a weight bearing joint.
This case illustrates a unique treatment for osteonecrosis of the humeral head which has not been reported in the literature. We acknowledge that this method is not a standard treatment for this condition; however the overall poor medical condition of the patient precluded a prolonged surgery. Using this technique, we were able to expeditiously treat both areas of disease and provide this patient with effective pain relief.
None.
The authors declare there is no conflict of interest..

©2015 Cerminara, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.