MOJ
eISSN: 2374-6939


Research Article Volume 10 Issue 5
1Service de Traumatologie etd
2Laboratoire d
Correspondence: Boubacar Soumare, Medecin Resident traumatologie-orthopedie A/Faculte de Medecine et de Pharmacie de /Universita Sidi Mohammed Ben Abdellah de Fes/Maroc,, Tel 213000000000
Received: August 10, 2018 | Published: October 26, 2018
Citation: Soumare B, Amine M, Sidibe S, et al. Patellar tendon rupture. MOJ Orthop Rheumatol. 2018;10(5):341-344. DOI: 10.15406/mojor.2018.10.00445
Patellar tendon rupture is a rare pathology with few cases series reported in literature. The aim of this study is to describe the epidemiological, clinical profile of patellar tendon ruptures as well as its operative management and outcome. We carried out a retrospective descriptive study involving 11 cases of patellar tendon rupture managed between 2012 and 2018 at the department of Traumatology and Orthopedic surgery A of Hassan II Teaching Hospital, Fez. It is an infrequent injury potentially occurring at any age in life with a clear predominance in young male adults.
All cases pertain to an acute post-traumatic rupture. Diagnosis was made preoperatively on physical examination in most patients. Surgery found a full body mid substance ruptures in most cases with a distal tear only in the 33.3% of cases.
Surgery is the mainstay treatment. It involves repair using vicryl 2sutures reinforced by a wire frame in most cases patients: transosseous sutures augmented with a steel wire frame or an autologous semitendinosus graft.
Functional outcomes were evaluated using Swik's criteria, with 58.3% cases exhibiting excellent or good results.
Thus the authors conclude that acute patellar tendon ruptures affect mainly young active males with surgery being the mainstay treatment that guarantees favorable outcome depending on the time of repair and postoperative patella height.
Keywords: orthopedic surgery, hospital, patients, epidemiological, traumatology
Patellar tendon can rupture following sudden forceful movement. Dynamic forces applied during sports are often higher than the static resistance of the tendon. In a healthy male (without patellar tendinopathy or underlying systemic disease), the patellar tendon ruptures when a force 17.5 times the body weight is applied. To illustrate, climbing a flight of stairs loads the patellar tendon by a force 3.3 times the body weight1 whereas jumping loads the tendon up 7 to 8 times the body weight. Acute patellar tendon ruptures are infrequent yet represent a severe potentially debilitating injury of the adult male with nearly 80% of cases involving patients under 40years old.2
We retrospectively reviewed the folders of 11 patients managed at the Department of Traumatology and Orthopedics Surgery A, Hassan II Teaching Hospital, Fez between May 2012 and May 2018. Only patients with an acute patellar tendon rupture were included in this study thus all patients with spontaneous rupture were excluded. All patients underwent emergent repair. Clinical presentation was dominated by patellar gapping, in addition to intense pain and inability to actively extend the knee. Plain x-ray, AP and lateral views, obtained in all cases to rule out any fractures or bony avulsions allows to measure patella height using the Caton-Deschamps index. Ultrasound was performed in 7 patients whereas 4 patients underwent MRI as part of preoperative workup.
All patients underwent repair under spinal or general anesthesia on an ordinary table in supine position with an upper thigh tourniquet to aid exposure. We performed an anterior approach with a midline skin incision extending from the patella apex to the tibial tubercle (TT). After careful dissection of tendinous sheath over the unruptured portion, the tendon was released along its length and all its edges. The ends of the tear were careful debrided as the tendon was brought together and sutured end to end and tied using the Judet suture technique.3 To protect against failed repair, a patellar tendon frame was made with either a steel wire passing through the patella and the TT, or an autologous tendon frame using semitendinosus in one case. Post-operative immobilization using removable splint was worn for a duration of 45days in all patients with brace-ambulation and weight bearing advocated on the 21st post-operative day. Rehabilitation began on the 3rd postoperative week with passive range of flexion up to 70° for up to 45days. Patients were regularly reviewed with routine physical and x-ray. After a minimum follow-up of 6 months we measured functional outcome using the Siwek criteria4 based on two elements: range of motion and quadriceps tone. Included in this series was a case of bilateral rupture in a young amateur sportsman of 25years who sustained the injury after being stabbed.
83.3% of cases involved patients aged less than 40years old, 41.7% were amateur sportsmen, 25% of whom were practicing daily and 91.7% were male. Tobacco and alcohol were the most common toxic habits with 25% and corticosteroids use was observed in 41.7% of patients.
Rupture was traumatic in all cases with direct impact (91.7%): 33.3% cases following fall, 25% of cases sports related injury, 8.3% due to accidents and 33.3% of cases involving stabbing injuries.
Pain and knee hemarthrosis was found in all patients with an open wound in 3 cases. Functional impairment was total in only 58.3% of cases. Pre-operative Caton-Deschamps showed patella alta in 83.3% of the patients which was corrected postoperatively.
Majority of the patients underwent emergent repair under spinal anesthesia in 75% of cases whereas 25% were operated under general anesthesia. The average admission time was 3hours (between 1-6hours). The mean hospital stay was 2days (ranging from 1-4days).
A midline anterior approach was used in all cases with peroperative discovery of: complete tear near the tip of the patella (33, 3%), midsubstance tear tendon (33, 3%), and near the TT in 25 % of cases.
Seventy-five percent of patients underwent end to end repair using the double KESLER suture technique protected by a steel wire frame in 33.3% of patients or autologous semitendinosus tendon frame in 33.3% whereas 25% of patients benefited repair using trans-osseous patella drills using vicryl 2 sutures in 2 cases and wire frame augmentation in 1 case.
Associated injuries included 1 case of patella fracture, 3 cases of meniscal injury and 1 case of anterior cruciate ligament (ACL) injury. After a minimum follow-up of 6months we noted flexion deficit of 10 to 20° in 3 patients whereas 2 patients had an extension lag of 5 to 10° compared to the uninjured side. According to Swik's criteria, these represented excellent or good results in 58% of cases (Figure 1).
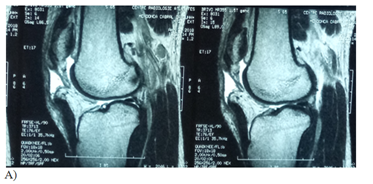
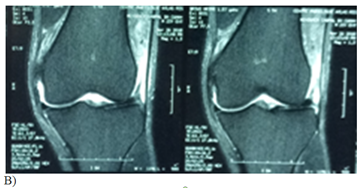
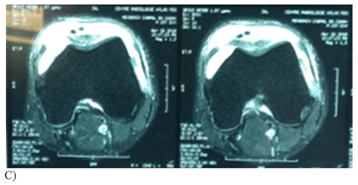
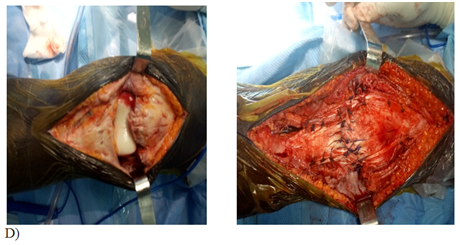
Figure 1 Case: Patient 28 years old male, 10 day history of sports injury with complete patella tear accident: we proceeded to a repair using trans-osseous patella suturing with vicryl 2 and reinforcement semitendinosus.
A-T2 sagittal section
B, C etc- coronal and axial section in particular sequence of proton density
D- per-operative image.
The actual incidence of patellar tendon rupture is not known. It accounts for the 3rd most frequent cause of adult native extensor mechanism ruptures after patella fractures and quadriceps tendon ruptures.5 It is often seen in young males under 40years old who rupture their extensor mechanism during sports activities.6 This is corroborated by our results with 83.3% of patients under 40 and a male predominance of 91.7%.
Rupture of the patellar tendon is often as a result of a direct trauma during the sports activity as was the case in our series with predominant causes being falls 33.3%, sports injury in 25% and assaults in 33.3%. Underlying tendinopathy or systemic disease and even repetitive micro trauma called "jumper’s knee" are also believed to be major risk factors of this pathology7 as the prevalence of "jumper’s knee" is more frequent in contact sports requiring high level of speed and strength of leg extensor mechanisms such as volleyball, football and athletics.8 In our series we observed a high prevalence of jumpers ‘knee in 41.7% of our amateur athlete population whereas substance abuse like tobacco and alcohol was noted in 25% and long corticosteroid use in 41.7% of the patients.
Clinically, patients present with acute knee pain, edema, and functional impairment and especially a palpable patellar gap and a failure to maintain active knee extension on physical examination.9 Plain X-rays could reveal "patella alta"10 The use of complementary diagnostic imaging such as ultrasound and MRI is necessary if there is surrounding diagnosis and allows associated injury assessment11,12 as evidenced by our study.
Current literature is unanimous on the emergent surgical repair of patella tendon ruptures. When the diagnosis of patellar tendon rupture is made, surgical repair should be considered regardless of the time of the rupture.9
Several techniques have been previously described for the repair which need to be used on a case-by-case basis.13 Surgical exploration during repair found rupture: close to the patella border in 33.3%, midsubstance tear 33.3%, and a complete tear near the TT in 25% of cases. Our results are similar to those of Ait Selmi,14 rupture usually occurs close to the patella border in 43% of cases, and the subpatellar region in 14% of cases.
Several techniques have been previously described for repair which need to be used on a case-by-case basis13 and in general, simple sutures are not biomechanically sound to allow for early motion. They need to be protected through one or several augmentation techniques using non-resorbable sutures instead of a metallic frame9 although in our series we found 33.3% of cases involved a steel wire frame. This augmentation technique is not without drawbacks. First the rigidity of construct, its tendency to fail and need for secondary surgery for hardware removal. Also its tendency to tilt the patella in the sagittal plane, or even to lower it.9 We also carried out an autologous tendon reinforcement using semitendinosus in 33.3% of cases as reported by many authors although we found large variety of autologous reinforcement techniques in literature (semi-tendinous, gracile –semitendinosus (GST) graft, fascia lata...). As in our series, most authors advocate postoperative immobilization,15 although a select few have reported excellent result with early motion.16,17 This they argue contributes to quadriceps muscle atrophy and joint stiffness. For our part, rehabilitation was started on the 45th postoperative day.
Functional outcomes are measured using several knee scoring systems available in literature an indirect indication of lack of reference. Our results are similar to those reported in literature .Despite numerous technically challenges, we reported favorable outcomes with 58, 3% excellent and good results according to Swik’s criteria. Outcome depends largely on the age of the patients, early repair and finally the technique of repair which confers adequate strength of construct to restore early motion and patellar height. The diversity of techniques of repair does not allow for clear cut guidelines regarding operative management of patella tendon ruptures.to a uniform therapeutic choice. Nonetheless, regardless of the technique of repair used, satisfactory outcome is usually attributed to early repair.
Patellar tendon rupture is an uncommon injury in the broad spectrum of extensor mechanism ruptures affecting young active males. Diagnosis is most often clinical. Management is surgical. (Early repair guarantees good functional outcome.
None.
The author declares no conflict of interest.

©2018 Soumare, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.