MOJ
eISSN: 2374-6939


Conceptual Paper Volume 5 Issue 1
Center for Sports Medicine, USA
Correspondence: Brett Sanders, Center for Sports Medicine, 26 ridge rock drive signal mountain, TN 37377, USA
Received: May 02, 2016 | Published: May 12, 2016
Citation: Sanders B (2016) Novel Reusable Transosseous Tunnel Based Soft Tissue Repair Techniques about the Shoulder: A Rational, Value BasedApproach. MOJ Orthop Rheumatol 5(1): 00164. DOI: 10.15406/mojor.2016.05.00164
The value based approach to medical care has created a new practice environment which is more focused on delivering non-inferior or equivalent evidence based outcomes at a sustainable cost. In a system where value based principles have been slowly adopted, shoulder care is ideally suited to provide leadership in value based medical practice.1 Technology remains a high cost driver for health systems, and surgeon owned facilities or gain sharing arrangements are beginning to enable the opportunity to co-align technology end users with payor’s incentives and that of institutional value assessment committees, which is critical to foster adoption of a value based approach.2 With regard to rotator cuff repair, outpatient rotator cuff repair saves cost when compared to inpatient repair, and open cuff repair is more cost effective compared to all arthroscopic.3,4 There is also evidence that anchor burden may increase cost significantly.5,6 Adla et al.7 showed that arthroscopic cuff repair was less cost effective by an average of $1,248.75 per case.7 Narvy et al.8 recently defined the direct economic cost of rotator cuff repair in the outpatient setting as $5,904.21.8 In their study, implantable anchors were the dominant cost driver, with a mean anchor cost per case of $3,432.67, with double row repairs averaging $4,570.25 anchor cost per case. In a similar vein, Genuario concluded in a decision-analytic model that double row rotator cuff repair was not cost effective for any size tear.5 While there is evidence that anchors increase cost, there is little evidence that any one implant or method is superior to another in terms of implants or repair techniques.9,10 Because clinical outcome does not correlate well with structural integrity of the cuff after repair, it is likely that various implants and techniques will be equivalent or non-inferior in evidence based analysis.11 Arthroscopic soft tissue repair about the shoulder offers a prime opportunity to provide high value, time honored repair techniques with updated cost effective arthroscopic approaches for our changing environment.
Transosseous cuff repair has been utilized with good success for decades, and is considered by many to be the gold standard.12-15 Arthroscopic transosseous approaches for cuff repair have been previously described in literature.16-20 More recently, arthroscopic tunneling has been performed with comparable results to standard anchor approaches21-24 In a recent retrospective case-control study of anchor based versus anchorless transosseous repairs, Srikumaran et al.6 showed no difference in ASES scores, NRS pain scores, SSV, procedural time, or ultrasound proven tendon integrity between arthroscopic transosseous technique and anchor based repairs for rotator cuff repair.6 Despite encouraging early evidence, arthroscopic transosseous technique has not been widely adopted, possibly because of technical difficulties, lack of familiarity, lack of marketing, or cost of a disposable device. To mitigate some of these concerns, a simple, reliable, and reusable device has been designed to enable all arthroscopic or open approaches to soft tissue repair in the outpatient setting for shoulder and other soft tissue repair procedures that may offer viable cost effective approaches with limited technology cost burden in a more sustainable fashion. As bundling payment methodologies approach, surgeons may be more incentivized to consider cost in the episode of care. This article will explore novel all transosseous and hybrid arthroscopic techniques and rational for soft tissue repair about the shoulder.
The Transos tunneler (tensor surgical, chattanooga, TN) is a reusable, value-based device which enables accurate and reliable tunneling through the humerus with simple retrieval mechanisms and simultaneous suture delivery and retrieval, reducing the number of steps and complexity in creating tunnels arthroscopically. (Figure 1) Similarly, it passes suture through compacted rather than drilled bone tunnels for added mechanical strength. This device can be used as a stand-alone device or in combination with anchors for a hybrid approach to soft tissue repair. Reusable tunnel creation allows extra fixation points and circumferential compression at no additional cost, thereby maximizing outcome and minimizing cost.

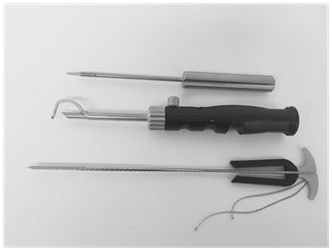
Figure 1 A reusable transosseous tunneler design breaks down for sterilization and allows repeatable transosseous tunneling within the case.
All transosseous approaches to rotator cuff repair have been previously described in the early 20th century, and are considered by many to still be the gold standard repair. Current technology allows the arthroscopist to create simple suture repairs, box repairs, or x box repairs with mattress and crossing sutures.18,19,25 Biomechanical studies have shown similar properties in anchor and tunnel repairs,25,26 with higher technology cost for the tunnel repairs.21 Early clinical studies have shown favorable results when comparing anchor based and arthroscopic tunnel repairs.22,23 Anchorless repairs may offer some potential advantages over anchor based repairs, given that Johst et al.27 have shown that strength or repair is determined only by the number of sutures crossing the repair site, not necessarily the number of anchors used.27
Biological considerations are currently believed to be the predominant factor in rotator cuff healing, along with clinical factors such as timing of repair, host factors, size of tear, and chronicity. An excellent biological milieu is created in transosseous repairs by allowing easy ingress of stem cells from the proximal humerus bone marrow to the repair site with no inert substance in the tunnel to block access. Bone tunnels essentially mimic the micro fracture technique of the tuberosity which has been linked with increased healing of the rotator cuff.28,29 The Transos device creates a 2.9mm medial and 1.9mm lateral tunnel, so there are no problematic bone voids in revision cases, and an anchor can always be introduced into the small diameter hole in the case of soft bone, a bone cyst, or any technical problem. Failure mode of transosseous repairs typically spare tendon substance, thus creating a less complex revision surgery in the case of a re-tear. If the failure mode occurs through suture cut through in the bone, it has occurred through one of the only tissues in the body that can heal with regenerative healing, allowing more options for revision fixation. If the failure mode of the repair construct is shifted to the biologically disadvantaged rotator cuff tendon, tendon truncation may occur, requiring a graft for salvage. Some anchor constructs exceeding the tendon modulus may create medial stress risers and tissue strangulation,30 which could contribute to tendon substance loss and difficult revision circumstances. Additional technical benefits of transosseous tunnels include excellent footprint area restoration through circumferential tendon compression, the ability to make large bone bridges with mattress sutures while simultaneously sealing off fibrinolytic synovial fluid from the repair site, and two fixation points per tunnel. Additionally, the surgeon may choose the number of sutures placed in the tunnel for added strength, and create unlimited repeat tunnels within a case with no extra cost burden. This is an important facet when considering that strength of the composite repair parallels the number of sutures through the tendon, not the strength of a bone- anchor interface.27 Similiarly, more tunnel fixation points with more sutures gives the surgeon an option for increasingly strong repair with a higher cost ceiling compared to increasing anchor fixation points alone. Arthroscopic grasping sutures and suture tapes are further methods to add strength to tunneled repair constructs. It is possible that a new goal in arthroscopic rotator cuff surgery should not be to reproduce a “transosseous equivalent” anchor repair, but rather to consider a “true arthroscopic transosseous” technique in conjunction with anchor repair to achieve a maximized gold standard repair while practicing value based medicine and minimizing cost.
All transosseous techniques offer several permutations and combinations of suture patterns. The simple repair, the box repair, and the X box repair, are demonstrated in Figure 2. These techniques allow for multiple small diameter fixation points to create whichever fixation pattern the surgeon chooses as appropriate.
A promising technique for small or partial tears (PASTA) is a single tunnel repair (Figure 3). As demonstrated, this repair can create excellent coaptation of the tendon, with added strength from suture grasping stitches. A single tunnel in small repair area can provide “2 for 1” fixation points relative to a single anchor with a true transosseous, circumferential stitches rather than a transosseous equivalent construct with multiple anchors. It is likely that lateral anchors in this clinical situation add little value relative to their cost.
For those new to tunneling techniques, a transitional approach with hybrid techniques may be of value, just as they have been with transitioning from open to mini-open to arthroscopic approaches for rotator cuff repair. Two hybrid techniques have been explored to provide maximum strength of repair in necessary situations at minimum cost, maximizing benefits of both repair strategies. There are an almost unlimited amount of anchor tunnel construct iterations and permutations possible, depending on specific needs. However, in the author’s experience, two have proved to be particularly useful, especially as a surgeon transitions from experience in all anchor approaches and becoming familiar with suture management.
Anchor Bounded hybrid Repair (Figure 4): This technique prioritizes anchors as the primary means of fixation, and allows for the repair of any sized cuff tear with a transosseous equivalent four anchor construct. This repair is typically applied in severely retracted tears, reconstructions, or tears with noncompliant tissue. Anchors are placed at the margins of the tear, securing the mechanically important cables of the rotator cuff, while the intervening tissue is circumferentially opposed to bone with either one or two transosseous tunnels. The tunnels between the anchors respect the biology and bone stock of the tuberosity, while adding additional circumferential compression points of the tendon footprint. Additional tunnels may be created as needed for “dog ears” or further cuff reduction. This paradigm may also be used in superior capsular or graft augmentations, as there are often edges of the graft which must be secured for stability of the graft interface, even after multiple anchors have been used (Figure 5).
Tunnel bounded, minimal anchor hybrid repair (Figure 6): Tunnel bounded hybrid repair technique prioritizes tunnels as the primary fixation and allows for repair of any cuff tear with at least a single anchor and multiple tunnels using a reusable device, creating a high value repair with five fixation points. A double or triple anchor is placed at the center of the repair construct. Two tunnels are placed at the anterior and posterior margins of the tear. Three sutures are placed in each tunnel. After passing all sutures through the tendon, the anchor sutures are tied at the medial margin of the repair site. A passing suture is used to shuttle the medial anchor sutures through the lateral tunnels in the inferior to superior direction, reconstructing the footprint as in a transosseous equivalent repair, without the need for extra lateral anchors. These sutures are then tied back to themselves, creating a medial mattress component with fixation to the anchor. The remaining simple transosseous sutures are then tied, using the lateral suture limb as the post. Only one anchor is used in this construct at the point of medial stress concentration, while the footprint is restored using circumferential compression sutures without the need for more lateral anchors. As many other single tunnels may be added as necessary to augment the repair. The medial tails of the sutures may then by incorporated into a secondary backup lateral anchor if desired, creating a double anchor hybrid repair (Figure 7). Anchors and tunnels are thus used synergistically to maximize repair integrity and minimize cost.
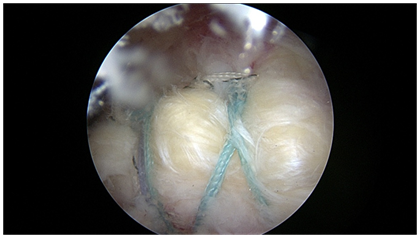
Figure 6 Single anchor: example of a tunnel bounded repair with a single anchor medially. Footprint reconstruction is achieved without the need for lateral anchors.
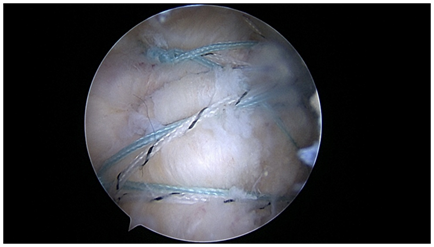
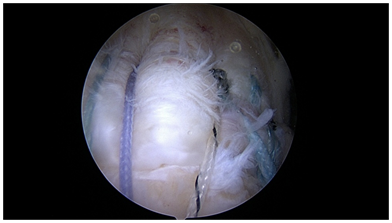
Figure 7 Tunnel bounded, double anchor repair: one medial and one lateral anchor are utilized with two tunnels, creating six fixation points.
Biceps tenodesis (Figure 8): Arthroscopic supra pectoral approaches to biceps tenodesis that release the sheath are an option for biceps tenodesis, likely because pain relief may be provided by releasing the biceps sheath.24,31 A transosseous approach in this setting reduces anchor use, and obviates the use of a potentially troublesome wound in the axilla. Bone in this area is the most robust in the proximal humerus, and thus readily accessible for strong fixation in anchorless techniques.
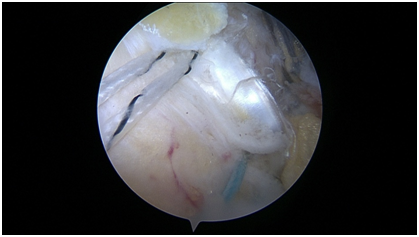
Figure 8 Biceps tenodesis: All transosseous suprapectoral biceps tenodesis with tendon grasping sutures.
The biceps may be released, or initially left in situ for this technique. We prefer to release the biceps to allow for an interesting tendon grasping repair. Two tunnels are created with an awl from an anterolateral portal after releasing the biceps sheath. The first tunnel is created from the same portal in the inferior position, just at the superior margin of the pectorals major and above the anterior circumflex vessels. The doubled suture is retrieved through the tendon from an accessory inferomedial portal, and a locking loop is formed utilizing a retrograde passing device. This suture loop is then locked with the lateral suture tail and tied arthroscopcially with the biceps at physiological length from a posterior arthroscopic grasper. The second, more superior tunnel is then created using the arthroscopic tunneler. This double passing suture is then brought through the tendon using a retrograde passing device from the inferomedial portal. Grasping instruments are used to pass the loop over the tendon, creating a strong circumferential grasp on the tendon. The retrograde device is then used to create another locking loop through the circumferential loop, creating excellent fixation with a “cinch loop configuration”. These sutures are then tied arthroscopically with the post lateral. The remaining tendon is removed, and the tendon ends are annealed with the electrocautery.32-38
Reusable arthroscopic transosseous tunneling is a reproducible and safe approach which adds multiple options to the arthroscopic surgeon’s armamentarium for many commonly performed arthroscopic procedures. These approaches may offer another surgical option for soft tissue repair which respects biology, offers a biomechanically sound repair, creates “two for one fixation points” with circumferential tendon compression, and synergies well with existing technology. As clinician’s incentives are increasingly aligned for value based treatments, these techniques could be employed to maximize clinical outcome, while minimizing cost in the value based era of medicine.
None.
None.

©2016 Sanders. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.