MOJ
eISSN: 2374-6939


Case Report Volume 13 Issue 3
1Senior Consultant, Department of Orthopedics, Al-Haramine Hospital, Bangladesh
2Assistant Professor, Department of Orthopedics, President Abdul Hamid Medical College, Kisoregonj, Bangladesh
3Classified Orthopaedic Surgeon, Combined Military Hospital (CMH), Bangladesh
4Assistant Professor, Department of Dermatology and Venereology, Sylhet MAG Osmani Medical College, Bangladesh
5Student of MS in Orthopaedics Course, Sylhet MAG Osmani Medical College, Bangladesh
Correspondence: Dr. Chowdhury Foyzur Rob, Senior Consultant, Department of Orthopedics, Al-Haramain Hospital, Sylhet, Bangladesh, Tel +8801715250800
Received: April 28, 2021 | Published: May 14, 2021
Citation: Rob CF, Mustofa MG, Islam LCMS, et al. Nonvascularized autologous fibular strut graft can be an option for treatment of segmental bone loss in comminuted femoral shaft fracture. MOJ Orthop Rheumatol. 2021;13(3):39-41. DOI: 10.15406/mojor.2021.13.00545
We present the case of a patient who suffered a comminuted femoral shaft fracture. The patient was a 20 years-old male following a sustained RTA and presented at our hospital after about 6 weeks after the incidence. Initially he was treated with skeletal traction with surgical toileting and debridement; and later on external fixator with dressing several times. Open reduction and internal fixation was performed with the use of a non-vascularized autologous fibular strut graft as an augmentation technique in conjunction with dynamic plating. Bony union occurred at 24 weeks. Clinically patient had stable, painless extremity, and resumed active use of the involved extremity without protective device after 2 year after femur fixation. No pain involving the donor graft site was reported at the time of the most recent follow-up examination. This case study demonstrates the use of free non-vascularized autogenous fibular strut bone graft as an option to bridge segmental bone loss in comminuted femoral shaft fracture. This is a relatively simple, not expensive procedure.
A large diaphyseal, segmental defect of bone is a challenge for an orthopaedic surgeon.1 This injury is increasing due to increase in social conflicts and road traffic accidents. These type of fractures are resulting from high-energy trauma and are of three types with A and B subtypes whether open and closed respectively. In developed countries orthopedic surgeons used many options to treat such type of fractures like vascularized bone transfers, bone transport, allogenic bone grafts, bone graft substitutes and several other options.2 However, in developing countries such options or expertise are not always available. They are relying on other treatment options.
At the beginning of the twentieth century non-vascularised fibular autografts was used as biological reconstructions in segmental defect of bone. The advantages of this technique over vascularised autografts are easier operative procedure, shorter operative time and remodeling capacity at the donor site.3,4
Application of dynamic compression plates (DCP) has been suggested in the fracture of the shaft of femur as it allows early mobilization. However fracture of the shaft of femur with segmental bone loss required an augmentation technique, cortical strut graft used as increasing mechanical strength of the site of the fracture.5–8
We present a case who suffered a comminuted femoral shaft fracture with segmental loss of bone. The reduction of the fracture site and stabilization with DCP were performed and a nonvascularized autologous fibular strut graft was applied.
We present a case who suffered a comminuted femoral shaft fracture with segmental loss of long bone. The reduction of fracture and fixation with long dynamic compression plate and a nonvascularized autologous fibular strut graft.
A 20-year aged male after a sustained Road Traffic Accident initially got admitted in Sylhet MAG Osmani Medical College Hospital, Sylhet with open fracture shaft of right femur. Radiographs demonstrated a fracture shaft of right femur type Gustilo IIIB with a segmental loss of bone. He was treated with upper-tibial skeletal traction and surgical toileting with debridement and was referred to National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, where they fixed the femur with external fixator and surgical toileting with dressing several times.
After about one and a half month the patient attended in Ibn Sina Hospital, Sylhet where surgical toileting was done and swab was taken from the wound for culture and sensitivity (C/S). Partial wound closure was done and was planned for fibular strut graft with ORIF. After five days of antibiotic treatment fibular non-vascularized fibular strut graft was planned. ORIF was by fibular strut graft and fixed with long and broad DCP (12 holes and 8 screws).
Patient was operated on under spinal anesthesia without using tourniquet. The right fibula was harvested using the procedure of Mukherjee et al.9
A part of safe area of right fibula was selected suitable for bridging the defect. At proximal and distal end of the selected part of fibula two small incisions, one cm in length were given. The selected part of the fibula was removed without injury the neurovascular bundle, and proximal and distal tibiofibular joints.
The fracture was opened by the lateral approach. The ends of the graft were accommodated 1cm inside the medullary canal of the femur and then were fixed with a long and broad dynamic compression plate (12 holes and 8 screws) to hold it to right femur.
Postoperatively, the patient was started rehabilitation and was discharged after 72 hours of the procedure. Follow up was done clinically and radiologically at 6, 12, 16, 20 and 24 weeks until bony union. The final radiological examinations showed osseointegration of the fibular strut graft (Figure 1–5) with complete healing of the fracture site and bony union was declared at 24 weeks.
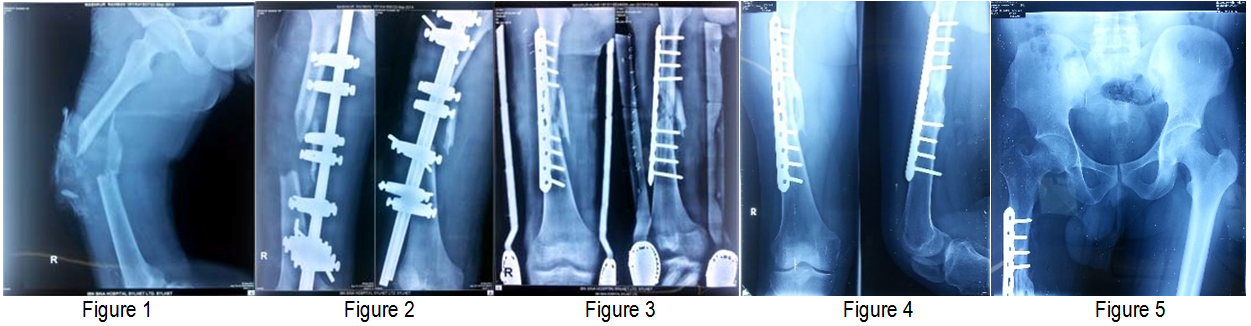
Figure 1 Lateral view of thigh (preoperative).
Figure 2 AP and Lateral view of thigh (postoperative).
Figure 3 Open reduction and internal fixation by metaphyseal locking plate.
Figure 4 AP and Lateral view of thigh shows Callus formation after 3 months of operation.
Figure 5 AP view of pelvis including hip joint to proximal thigh.
In the final follow up at 2 year, the patient was stable, right lower limb was painless extremity, and resumed active without using any protective device and absence of pain at the site of donor graft in the fibula (Figure 6).
Vascularized fibular autograft in segmental defect in long bone is a microsurgical technique. On the other hand non-vascularized fibular graft application is a autograft with rapid technique and is suitable than an allograft.10,11 Moreover, it is easily available without hampering the donor-site morbidity.12 This technique is also suitable for the most of orthopedic surgeons to carry out the procedure in an average setup.13,14 The nonvascularized fibular strut grafts, a reliable surgical options to reestablish continuity of bone in segmental defects in long bone was reported in several studies.2,7,8
Like several authors, we accommodated the end of the fibular strut grafts inside the medullary canal of the fragment of femur.7,8
The previously reported complications of fibular graft were injury in common peroneal nerve, infection, weakness of extensor hallucis longus, instability of ankle joint, nonunion, and stress fracture.2,9 To prevent these complications during fibular harvest, at least 5 cm of the upper and the lower parts of the fibula should be preserved.2,4 By preserving the 5 cm of lower part of fibula, complications related to the distal tibiofibular syndesmosis and the ankle joint instability can be prevented.15 Moreover, harvesting nonvascularized fibular strut graft as a biological autograft mentioned in the study conducted by Mukherjee et al.9 reduces the morbidity of donor site. It is safer than conventional vascularized fibular strut graft. Several studies reported that application of fibular autograft resulting in osteogenic stimulus and subsequent good results was obtained.3–8,15,16
In our patient we do not use cancellous bone graft because the defect was basically shaft of the femur and we did not face any difficulties in using the fibular strut graft. Taraz-Jamshidi et al.17 treated 15 patients with giant cell tumor of distal radius by en-block resection and reconstruction with nonvascularized fibular autograt without additional cancellous bone autograft and found solid bone union in all patients.
Nonvascularized fibular strut autograt is a good option for treatment of segmental bone loss in comminuted femoral shaft fracture. It is a simple, not expensive options in bridging the segmental loss of bone.
The authors have obtained the patient’s written informed consent for print and electronic publication of the report, as well as permission for the use of photographs.
None.
The authors declare that there are no conflicts of interest regarding the publication of this paper.

©2021 Rob, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.