MOJ
eISSN: 2374-6939


Research Article Volume 11 Issue 1
1Assistant Professor, Department of Orthopaedic Surgery, J N Medical College, India
2Professor, Department of Orthopaedic Surgery, J N Medical College, India
Correspondence: Yasir Salam Siddiqui, Assistant professor, Department of Orthopaedic Surgery, J N Medical College, AMU, Aligarh, Uttar Pradesh, India, Tel 9837343400
Received: January 09, 2019 | Published: January 25, 2019
Citation: Siddiqui YS, Khan AQ, Asif N, et al. Modes of failure of proximal femoral nail (PFN) in unstable trochanteric fractures. MOJ Orthop Rheumatol. 2019;11(1):7-16. DOI: 10.15406/mojor.2019.11.00460
Background: Several fixation devices have been developed to overcome the difficulties encountered in the management of the unstable trochanteric fractures. PFN in unstable fracture patterns is progressively becoming standard method of fixation in view of its superior biomechanics and prevention of varus collapse in comparison to extramedullary devices. However, evolution of PFN is also not free from complications and may comprise complications associated with the migration of the interlocking head screws (Z-effect and reverse Z-effect), varus collapse, screw cutout, peri-implant fracture, non-union, delayed union, shortening and infection.
Aims & Objectives: The objective of the paper is to describe the technical hitches, errors and modes of failure of PFN in unstable trochanteric fractures with their literature-based explanations and the recommendations to avoid such complications.
Materials and methods: The current study is a critical appraisal of the technical hitches, errors and modes of failure of PFN in the course of its evolution in treatment of unstable trochanteric fractures. All patients with unstable trochanteric fractures from July 2013 to June 2015, treated with PFN were included in the study. The technical complications involved with surgical procedure and techniques adapted to overcome such complications were noted. All patients were followed up for a period of 2 years and final outcome assessment comprised the post-operative complications, mobility status, shortening and Harris hip score.
Results: Forty five patients with unstable trochanteric fractures were treated with PFN during the study period. Forty two patients were available for final follow up at 2 years. Technical difficulties with the implantation of the PFN were documented in a total of 16 patients (35.55%) which included failed closed reduction in 8, entry point issues in 7, guide wire breakage in 3, fracture at nail tip in 1, difficulty in proximal locking due to Jig mismatch in 4. Post-operative complications included varus mal-reduction in 4, lag screw cut-out leading to non-union in 2, differential migration of screws in 3, locking bolt missing the nail hole in 1 and peri-implant fracture in 1. All fractures went into union, except two with mean shortening of 0.5 cms. Mean neck shaft angle achieved post reduction was 130.5 degrees (range from 125-137) and at final follow up was 129.8 degrees.
Conclusion: Even though intramedullary fixation is an established method of treatment of unstable trochanteric fractures, the evolution of the procedure is not free from complications. Surgery is technically demanding. However with proper execution, good outcome can be achieved with acceptable rates of complications even in unstable trochanteric fractures. Concerning the techniques making proper entry point, adequate reaming of proximal femur, passing the nail to avoid varus & distraction at fracture site and placing the lag screw in the inferior part of neck in anterior posterior projection and central in lateral projection reduces risk of fixation failure.
Keywords: Unstable trochanteric fractures, PFN, Z-effect, Reverse Z-effect, Varus collapse, Cut-out
Trochanteric fractures are one of the commonest fractures in aging population.1 The prevalence of these fractures has increased substantially over the last few decades as a result of the larger longevity of the population.2 About 35 to 40% of such fractures are unstable one.3,4 Surgical stabilization of these fractures is preferred method of treatment for restoring pre-fracture mobility.5,6 Several fixation devices have been developed to overcome the difficulties encountered in the management of the unstable trochanteric fractures. Of late, most of these fractures were treated by lateral devices. As lateral devices were associated with high rates of complications7,9 intramedullary fixation devices have become gradually more prevalent.10–12 The proximal femoral nail (PFN) is an intramedullary system, intended to improve the management of unstable trochanteric fractures. Intramedullary implants are preferred in treatment of unstable trochanteric fractures, especially in the absence of medial buttress.13,14 In 1997 the AO designed an innovative intramedullary implant, the proximal femoral nail (PFN)6 for management of such fractures. Hence, PFN in unstable fracture patterns is progressively becoming standard method of fixation in view of its superior biomechanics and prevention of varus collapse in comparison to extramedullary devices.15 However, the evolution of the procedure may include complications associated with the migration of the interlocking head screws (Z-effect and reverse Z-effect), varus collapse, screw cutout, peri-implant fracture, non-union, delayed union, shortening and infection. The objective of the paper is to describe the technical hitches, errors and modes of failure of PFN in unstable trochanteric fractures with their literature-based explanations and the recommendations to avoid such complications.
The current study is a critical appraisal of the technical hitches, errors and modes of failure of PFN in the course of its evolution in treatment of unstable trochanteric fractures. All patients with unstable trochanteric fractures from July 2013 to June 2015, treated with PFN were included in the study. All the patients gave the informed consent for inclusion into study and the study was approved by the ethical committee of our hospital. The study was performed in harmony with the Ethical standards of the 1964 Declaration of Helsinki as revised in 2000. All unstable fracture patterns according to AO/OTA classification were included in the study16 comprising fracture patterns including the reverse oblique, broken lateral wall, trochanteric fracture with subtrochanteric extensions. All patients were evaluated at the end of 2 years. Pre-operative evaluation of the patient included age, sex, mode of injury, fracture classification, pre-operative mobility status, Harris hip score17 and other co-morbidities. Patients were operated on fracture table with closed or minimal open reduction to create a mechanically stable fracture-bridging osteosynthesis using PFN. Fixation of fracture with a PFN was carried through longitudinal traction on a fracture table, under C-arm guidance, with five small incisions (one for entry point, two for proximal locking screws and two for distal locking bolts). In the case of failed closed reduction, manipulation with Steinmann pin was done (Figure 1a & b), and in some cases we have to enlarge the probable incision site for proximal neck screws, so as to apply reduction forceps. For distal locking we mostly used both dynamic and static locking bolts. Both shorter and longer versions of nail were used depending upon the extent of fracture. The intraoperative characteristics studied were duration of surgery, blood loss and technical difficulties encountered in fixation with PFN. Post-operative findings recorded were post-operative complications, mobility status and shortening at final follow-up of 2 years. For better understanding of PFN implantation techniques, the technical hitches were classified into:
1) Issues related to Reduction
2) Issues related to entry point and guide wire placement
3) Issues related to PFN insertion
4) Issues related to accurate placement of lag screw and derotation screw
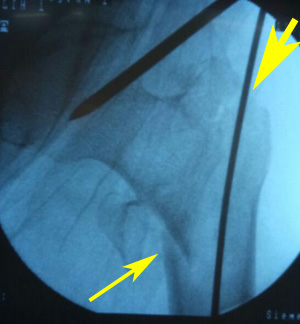
Figure 1a Varus reduction as demonstrated by medial overlap of fragments (thin arrow). Also note lateralization of entry point (thick arrow).
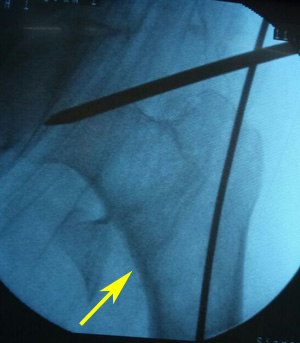
Figure 1b Manipulation with Steinmann pin to correct neck shaft angle as demonstrated by medial continuity and correction of overlap (arrow).
Methods used to solve these problems were noted in the operative notes and these data were used for discussion and analysis.
A total of 45 patients with unstable trochanteric fractures were treated with PFN from July 2013 to June 2015. Two patients expired within 6 months of surgery and one patient was lost to follow-up; hence were excluded from study. Lastly, 42 patients were available for final analysis (Table 1). Among them there were 23 males and 19 females. Domestic falls were the cause of injury in majority of patients (30 Patients) followed by road side accidents (12 patients). Mean age of patients was 67.4 years (range 27 to 82 years). As per AO/OTA classification, there were 26 type A2 fractures and 16 A3 fractures (thus a total of 42 unstable fractures fixed with PFN were available for critical analysis). Technical difficulties with the implantation of the PFN were documented in a total of 16 patients (35.55%) which included failed closed reduction in 8, entry point issues in 7, guide wire breakage in 3, fracture at nail tip in 1, difficulty in proximal locking due to Jig mismatch in 4 (Table 2). Closed reduction failed in 8 patients, requiring extension of the probable incision site for proximal neck screws, so as to apply reduction forceps (17.7%). Average duration of surgery was 65 minutes (range 45 – 90 minutes). Immediate post-operative AP & lateral radiograph was assessed for quality of reduction, neck shaft angle (NSA) and position of hip screws. In 38 patients, lag screw was in the centre or inferior position while in 4 it was in the superior part of the head on antero-posterior projection. Post-operative complications included varus mal-reduction in 4, lag screw cut-out leading to non-union in 2, differential migration of screws (Z effect/Reverse Z effect) in 3, locking bolt missing the nail hole in 1 and peri-implant fracture in 1. At final follow-up of 2 years, all patients except two with screw cut out and non-union were walking independently. Mean time for fracture union was 6 months. Mean neck shaft angle achieved post reduction was 130.5 degrees (range from 125-137) and at final follow up was 129.8 degrees. Mean limb length discrepancy at final follow up was 0.5 cms. Functional assessment with Harris hip score showed almost near return to pre-injury score (pre-injury score of 76 versus final follow-up mean score of 70).
|
Total no. of patients available for final follow-up |
42 |
|
Male : Female Ratio |
23:19 |
|
Mode of injury |
Domestic falls = 30 Road Side Accident = 12 |
|
Mean Age |
67.4 years (Range 27 – 82 years) |
|
Mean Follow-up |
27 months (Range 24 – 36 months) |
|
Blood loss |
Approx. 75 ml |
|
Mean duration of surgery |
65 minutes (range 45 min. to 90 min.) |
|
Mean length of Hospital stay |
7.5 days (Range 5 – 14 days) |
|
Mean time to ambulate with support |
Third post-operative day |
Table 1 Demographic and operative details of patients
|
Technical Hitch |
Number |
|
Failed closed reduction |
8 |
|
Entry point issues |
7 |
|
Breakage of guide wires |
3 |
|
Fracture of Proximal femur |
0 |
|
Fracture at nail tip |
1 |
|
Difficulty in proximal locking due to Jig mismatch |
4 |
Table 2 Technical difficulties with implantation of PFN
Nevertheless PFN is technically demanding procedure, with appropriate technique; it gives excellent results even in unstable fracture patterns. The important technical aspects are attaining good reduction with acceptable neck shaft angle, making correct entry point, inserting nail properly and precise placement of lag screws.
The technical problems faced during surgery were classified as follows:

Figure 2a Radiograph showing lateralization and enlargement of the entry portal, with the nail acting as a distracting device (small arrow). Also note the varus mal-reduction (long arrow).
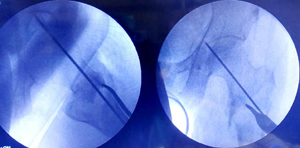
Figure 3b Preliminary fixation with K-wire before making entry point, so as to avoid loss of reduction while reaming and subsequent nail insertion.
There can be hitches while reaming over guide wire for hip screw, as guide wire may bend slightly as it reaches the hard subchondral bone. Drilling over bent guide wire may result in its breakage. We had 3 such complications. We recommend partial drilling over guide wire just proximal to bend, followed by pulling of guide wire up to the level of its bend, then drilling of hard subchondral bone by drill bit itself under C - arm guidance to prevent guide wire breakage. The guide wire is then reinserted after the removal of reamer for screw insertion. One should also avoid using previously damaged guide wires. Sometimes there is mismatch between the jig and the nail leading to difficulty in negotiating the drill for the hip screws due to some manufacture or implant assembly related problems. We had 4 such problems, three for lag screw and one for derotation screw. Prior to nail insertion, one should check the jig nail assembly for its alignment. Drilling with smaller sized reamer and proceeding with regular reamer will also help. One should also check the jig whether it is loosened or not. Sometimes manipulation and hammering may result in loosening of jig and subsequent mismatch. Sometimes distal locking may also be troublesome. In one of our case distal locking bolt missed the nail while in another hammering the Steinmann pin to make entry portal for locking bolt, resulted in iatrogenic fracture (Figure 4a & b). Patient was put on long leg slab, which resulted in healing of the iatrogenic fracture. One should always do locking with drill bits and should avoid doing with Steinmann pin and hammer, which may shatter the cortex as was seen in our patient.
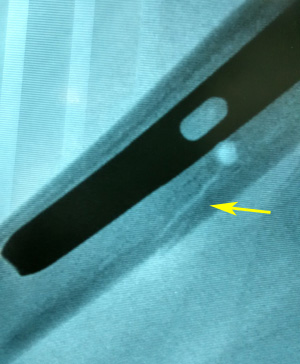
Figure 4a Image showing the iatrogenic fracture of the femur at locking bolt site, as a result of hammering the Steinmann pin to make entry portal for locking bolt (arrow).
Post-operative complications
During the observation period there were no postoperative haemorrhages or infections that required therapy. The complications developed following fixation of fractures with the PFN are tabulated in table – 3, and are discussed underneath.
|
Complications |
Number of patients |
|
Varus Mal-reduction |
4 |
|
Lag screw cut-out |
2 |
|
Non-union |
2 |
|
Z effect/reverse Z effect |
3 |
|
Missed distal locking |
1 |
|
Peri-implant fracture |
1 |
|
Nail breakage |
0 |
Table 3 Post-operative Complications
Varus mal-reduction and lag screw cutout
We have 4 cases of varus mal-reduction. Out of these 4 cases, two patients developed cutout, rest of the two went into successful varus mal-union. The 2 cutouts in our study had a fracture classification of 31-A2.3 and 31-A2.2. In addition, the fractures were inadequately reduced and noted to be fixed into a varus position (Figure 5a & b). Placement of hip screw is critical in the ultimate successful outcome of unstable trochanteric fractures. The tip-apex distance (TAD) has been described by Baumgaertner and associates22,23 as a useful intraoperative indicator of deep and central placement of the lag screw in the femoral head, regardless of whether a nail or a plate is chosen to fix the fracture.19 Position of hip screws in head and neck is dependent on quality of reduction. Varus reduction causes placement of hip screws in superior part of head and neck, leading to varus collapse and early cutout (Figure 5b & c). It is important to note that absolute anatomical reduction of unstable trochanteric fractures is a wishful thinking. One should target to achieve antero-medial reduction with correct neck shaft angle. P Janardhana Aithala15 also reported that maintenance of correct neck shaft angle and version leads to union, irrespective of comminution and non-anatomical reduction. Hence, the most important technical aspect of PFN implantation is maintaining the appropriate neck shaft angle so as to place hip screws in desirable position. Both are interlinked as screw placement angle is prefixed and hence unless good neck shaft angle is achieved, it is impossible to put the hip screw correctly. In the AP projection, varus at the fracture site is the main hitch to place the screw in centre or inferiorly, while in lateral projection posterior sagging or flexion of proximal fragment is the problem in putting the hip screw centrally. Several studies have reported a cutout rate of 2%–8%.10,26-31 We observed a cut-out complication in two patients (4.76%). One of them underwent partial hip arthroplasty, whereas the other one opted for implant removal only. Considering the two cut-outs in our study with resultant fixation failure, we believe it is more of technical failure rather than failure of implant. Proper execution of the procedure will give superior results. Our recommendation for lag screw placement position especially in dual screw nails is inferior in AP projection and central in lateral projection.

Figure 5b Post-operative radiograph showing varus mal-reduction (pointed by thin arrow as medial overlap of fragments). Also note the superior position of the screws (thick arrow).
Differential migration of screws (Z-effect & Reverse Z-effect)
Z-effect and reverse Z-effect are complications that arise from the surgical treatment of trochanteric fractures with PFN comprising two interlocking head screws. Such complications are induced by the migration of screws in opposite directions, which may lead to treatment failure. The Z-effect involves the lateral migration of the lag screw, varus collapse and perforation of the femoral head by the superior derotation screw. The reverse Z-effect involves the lateral migration of the superior derotation screw accompanied by the medial migration of the lag screw. The first account of the Z-effect has been attributed to Werner-Tutshcku, et al.25 who reported an incidence of 7.1% in his study. While the published works designates the Z-effect and reverse Z-effect as the migration of proximal interlocking screws in opposite directions, in practice, sometimes only one screw actually migrates and the fracture undergoes an accommodation process that may lead to the perforation of the femoral head by the screw that remains in the normal position.32 Although the cause of this complication has been explained by varus collapse of the fracture and the lack of medial cortical support, its precise etiology requires further elucidation.33 Strauss EJ, et al. hypothesized in a biomechanical model that Z-effect & reverse Z-effect is the result of mismatch between the compressive strengths of the femoral head & femoral neck (later being lesser), which simulates fractures that have significant medial cortex comminution that are prone to varus collapse.33 Weil YA, et al. hypothesized that the nail toggling due to deficient lateral buttress & an unstable calcar pattern, leads to differential screw migration.34 We have total 3 cases of differential migration of screws. They are discussed here in detail (Table 4).
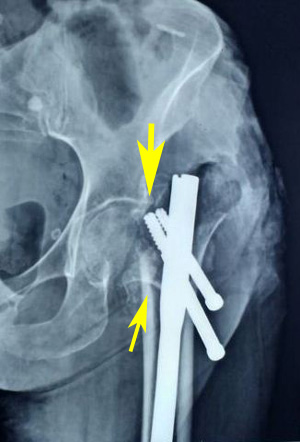
Figure 5c Six weeks post-operative radiograph showing varus collapse (thin arrow), cut-out (thick arrow) and fixation failure.
|
Case No. |
Age/Sex |
Mode of Injury |
Fracture Classification |
Time of development of Z-effect/Reverse Z-effect |
Possible factors contributing for differential migration |
|
1 |
70 years/Male |
Domestic Fall |
31A2.3 |
Z-effect at 3 months |
1. Unstable fracture pattern 2. Osteopenia 3. Superior position and size of screws 4. Lack of antero-medial buttress 5. Short nail 6. Early weight bearing |
|
2 |
32 years/Male |
Road side accident |
31A2.2 |
Reverse Z-effect at 5 months |
1. Unstable fracture pattern 2. Lack of anterior buttress 3. Short nail 4. Early weight bearing |
|
3 |
40 years/Male |
Road side accident |
31A3.1 |
Z-effect at 3 months |
1. Unstable fracture pattern 2. Lack of anterior buttress |
Table 4 Z-effect/Reverse Z-effect with possible factors contributing for differential migration of hip screws
Case 1
A 70 year old male with unstable fracture pattern was submitted to osteosynthesis with PFN. The fracture was classified as AO/OTA type 31A2.3 (Figure 6a). Immediate post-operative radiograph of the patient revealed relatively unstable fracture fixation because of loss of antero-medial buttress, superior placement of hip screws, almost same level of screw tips of both lag and derotation screw (Figure 6b). Because of relatively unstable fracture fixation, patient was advised delayed weight bearing. At home, patient started weight bearing with aid of walking frame. At 3 months post-operative, the patient evolved with varus collapse and differential migration of the hip screws, with the caudal one migrating laterally (typical of the Z-effect, Figure 6c). Patient was offered for removal of derotation screw. Patient refused for any surgical intervention as he was up and about with walker with minimal pain.

Figure 6b Immediate post-operative radiograph showing loss of antero-medial buttress (arrows). Also note the superior placement of hip screws & almost same level of screw tips of both lag and derotation screw.

Figure 6c Three months post-operative radiograph showing varus collapse (small arrow) and differential migration of the hip screws (long arrow), with the caudal one migrating laterally (typical of the Z-effect).
Case 2
A 32-year old male with a road side accident, presented with intertrochanteric fracture of the right femur (AO/OTA 31-A2). The patient was submitted to osteosynthesis with PFN. Immediate post-operative radiograph of the patient revealed acceptable NSA, acceptable position and size of screws, restoration of medial buttress. However anterior bony contact was lacking (lack of anterior buttress). Patient was on regular follow-ups, and at 5 months post-operative he developed varus collapse and reverse Z-effect. Gradually superior derotation screw migrated laterally, with inferior lag screw migrating medially. The resultant varus collapse headed to perforation of the femoral head by the inferior lag screw (reverse Z-effect). As fracture was uniting, we removed the inferior lag screw and tightened superior derotation screw, which lead to successful union of fracture at 9 months. Radiographic images of the patient are presented in Figure 7.
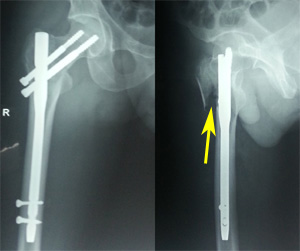
Figure 7b Immediate post-operative radiograph showing restoration of NSA & medial buttress. Also note the acceptable position & size of screws. Arrow in lateral view showing lack of anterior bony contact.

Figure 7c Three months post-operative radiograph showing development of varus at fracture (arrow) and backing out of hip screws.

Figure 7d Five months post-operative radiograph showing varus collapse (long arrow) and differential migration of the hip screws (small arrow), with the caudal one migrating medially & perforating the head (typical of the reverse Z-effect).
Case 3
A 40-year old male was injured in a road side accident resulting in intertrochanteric fracture of the left femur (AO/OTA 31-A3.1). The patient was submitted to osteosynthesis with PFN. Immediate post-operative radiograph of the patient revealed acceptable NSA, acceptable position and size of screws, restoration of alignment, but not maintaining anterior bony contact. At 3 months post-operative, the patient presented with lateral migration of the lag screw, with the derotation screw maintaining its original position (Z-effect). Patient was kept on strict follow-up, so that any chance of failure of fixation can be detected. At 7 months, patient showed clinico-radiological signs of union. Although, the lag screw moved laterally, but it was still well positioned with regard to the tip apex distance and the fracture was adequately aligned, hence no failure in osteosynthesis occurred. Radiographic images of the patient are presented in Figure 8.

Figure 8b Immediate post-operative radiograph showing restoration of NSA & medial buttress. Also note the acceptable position & size of screws. Arrow in lateral projection showing lack of anterior bony contact.

Figure 8c Three months post-operative radiograph showing lateral migration of the lag screw, with the derotation screw maintaining its original position (Z-effect).
Non-union
Though, postoperative non-union of intertrochanteric fracture is relatively rare, we had 2 cases of cutout leading to non-union. Factors contributing for non-union were fracture fixation in varus, superior placement of screws, osteopenia, and unstable fracture geometry. In our cases, even after fixation of a fracture with PFN, local instability at fracture site persisted leading to abnormal stresses and the fixation failed to provide a stable mechanical environment for fracture healing. One patient underwent arthroplasty procedure while other opted for implant removal only. Radiographic images of one patient are presented in Figure 5.
Peri-implant fracture
An unavoidable complication of peri-implant fracture occurred in 80 year old lady, following fall at 2 months after fixation of a 31A2 fracture with a PFN. She sustained a femoral shaft fracture at the level of the distal locking bolt (Figure 9). By changing the implant for a longer nail, we were able to achieve healing of the fracture. Initially patient was fixed with shorter version of PFN. Our recommendations for fixation of unstable trochanteric fractures with osteoporosis are to put longer nails, so as to splint the whole femur.
Our study highlights the technical hitches and modes of failure of PFN in unstable fracture pattern, but small sample size and retrograde design of study are the limitations of current study. Further studies are required to focus on improving the techniques of PFN and augmenting its stability, especially in unstable osteoporotic fractures to make the evidence strong that good outcome can be achieved with acceptable rates of complications in unstable trochanteric fractures.
Even though intramedullary fixation is an established method of treatment of unstable trochanteric fractures, the evolution of the procedure is not free from complications. Considering the failures in our study, we believe they are more of a technical failure, rather than failure of implant. Achieving good reduction (maintaining NSA, alignment & length) and placement of hip screws in a correct position are two important technical characteristics which prevent most of the complications associated with PFN. Although surgery is technically demanding, if one gives vigilant attention to minute technical aspects of the procedure as discussed above, good outcome can be achieved with acceptable rates of complications even in unstable trochanteric fractures.
None.
None.

©2019 Siddiqui, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.