MOJ
eISSN: 2374-6939


Research Article Volume 12 Issue 4
Orthopaedic Trauma Surgeons, Santander University Hospital, Colombia
Correspondence: Carlos Arroyo Sánchez, Orthopaedic Trauma Surgeons, Santander University Hospital, Bucaramanga, Colombia, Tel +57 3123251248
Received: January 27, 2020 | Published: July 24, 2020
Citation: Sánchez CA, Abril C, David A, et al. Minimally invasive surgery of humeral fractures with posterior approach and anatomical plate. MOJ Orthop Rheumatol. 2020;12(4):80-84. DOI: 10.15406/mojor.2020.12.00523
We evaluate the functional and radiological outcomes, the union rates and functional results in a group of patients with diaphyseal fracture of the humerus of the distal third with a minimally invasive technique whit posterior approach and anatomical plate. Between 2013 and 2017, 32 patients were operated, with an average age of 31years. Functional assessment was performed using the abbreviated DASH functional scale and pain was classified according to the VAS scale.
All the fractures healed successfully, except for two cases that presented in union delay. The radial nerve injury prior to the intervention was recovered progressively without requiring transfers. The functional results were satisfactory in the patients who completed more than one year of follow-up. The posterior approach of the minimally invasive surgery in the treatment of this particular fracture pattern seems to show a biological advantage by allowing complete union rates in all patients. The iatrogenic injury of the radial nerve does not seem to increase in relation to its isolation and protection in the proximal portion of the triceps Level of evidence: IV
Keywords: humerus fractures, minimally invasive approach, posterior approach, anatomical flocking plate
Diaphyseal humerus fractures belong to 3 to 5% of fractures in general.1,2 Diaphysis engagement in its middle third is the most common with around 60%.1 Fractures with compromise of the distal third of the diaphysis have an 10 - 48% of incidence.1,3 Surgical treatment of this subgroup of fractures has shown good functional results on the Bickel-Perry scale when compared with non-operative treatment, reporting excellent and good outcomes.4 The rates of union seems to be higher in the surgical treatment compared with the non-surgical treatment, the last has an increasing in the rate of non-union up to six times.5,6
Previous papers has shown the benefit of minimally invasive techniques in surgical treatment in terms of safety, functional results and biological advantages.6–8 Within the minimally invasive surgical approaches used, we found the anterior and lateral approach.9 The posterior approach has been indicated in the treatment of fractures close to the olecranon fossa allowing a greater location of screws in the distal portion of the plate, generating greater stability. However, we consider that the application of straight plates can generate difficulties in the location of multiple distal screws and it is technically difficult to bend the implants. We present an evaluation of the clinical and functional results in a series of cases of patients with fractures of the distal humeral shaft treated with distal extraarticular anatomical humerus plate with a posteriorly minimally invasive approach.
Between the years 2013 to 2017, 32 patients with a diaphysial fracture of the humerus located in its distal third were included in the case series.
The inclusion criteria for treatment with this technique were:
Fractures proximal 6cm from the olecranon fossa; fractures AO 12 A 1.3, 2.3 and 3.3. AO 12 B 1.3, 2.3 and 3.3 and AO 12 C 3.1, 3.2 and 3.3. Damage of the soft tissues in the anterior surface of the arm. We also included patients fractures with unacceptable angulation in varus or valgus, associated or not with radial nerve injury.
Patients affected with distal humerus articular traces, under 18 years old, pathological fractures, poor state of soft tissues in the posterior aspect of the arm, those who underwent an open posterior approach and those who did not tolerate the prone position were excluded. All patients were informed about the surgical technique and accepted their surgery consent.
A data collection form was used to record sociodemographic, clinical and follow-up variables. The operative notes were evaluated to locate the specific data describing the injury and surgical technique and radial nerve injury. Shoulder and elbow range of motion (ROM) were measured in the office by the treating surgeons with goniometry. The pain was value with the visual analogue scale (VAS). The Quick-DASH (Disabilities of Arm Shoulder and Hand) functional score was applied in its version adapted to Spanish.
Surgical technique
The patient was located in prone position with a support in the middle third of the affected arm. The anatomical landmarks are: olecranon, lateral epicondyle, medial epicondyle, radial nerve, ulnar nerve. A first incision was made between the lateral column and the olecranon fossa, two centimeters proximal from the lateral lateral epicondyle making a lateral window to expose the distal humerus. Then a skin mark is made with the plate to make the proximal incision (Figure 1). A 3cm proximal incision is made in the posterior arm , the radial nerve its exposed between the long portion of the triceps and the posterior edge of the deltoid , is repaired with a vessel loop to avoid its compression during the plate fixation. An LCP anatomical extraarticular 3,5mm plate (Depuy Synthes) is it slipping retrograde from distal in the lateral epycondile placing it below the radial nerve. Reduction of the fracture is made with axial traction and compression maneuvers verified by fluoroscopy. We put the first screw in the distal portion of the plate on the lateral column; and then we put the first proximal screw achieving the alignment in the anteroposterior plane avoiding distal displacement. Once the reduction of the fracture and optimal plate location are confirmed, the distal screws are fixed, alternating with proximal screws until a minimum of six corticals proximal and distal. Finally, the reduction was verified by fluoroscopy.
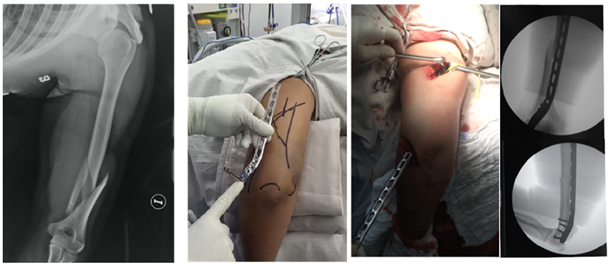
Figure 1 Humeral fracture fracture due to horse fall. Note the landmarks and approach maneuver with dissection of the radial and distal nerve over the lateral epicondyle. Sliding of the plate and revision of the reduction by fluoroscopy.
In case of a radial a radial nerve injury in a closed fracture, no routine exploration was performed in the proximal portion, except in cases of exposed fracture where it was necessary at the time of debridement to determine the interposition of the radial nerve. A soft brachiopalmar immobilization and a palmar hand splint were applied in cases where the nerve was injured. The clinical control was carried out at two weeks, the second month, the fourth month and the postoperative year. Rehabilitation was started at the second postoperative week (Figure 2).
The mean age was 31.5 years (range 17-78, SD +/-14.9). 65% were male and 35% female. According the trauma mechanism, the traffic accident was the most common with 14 cases, followed by 13 falls, gunshot wounds in four and the work accident in one case (Table 1).
|
Case |
Age |
Gender |
Mechanism |
AO |
Open fracture |
Complications |
Union time weeks |
Alignment |
Follow up months |
|
1 |
30 |
M |
Car Accident |
12A2.3 |
No |
Praxia Radial |
12 |
2º |
12 |
|
2 |
78 |
F |
Fall |
12C1.1 |
No |
No |
12 |
0º |
14 |
|
3 |
23 |
F |
Carr Accident |
12A1.3 |
No |
No |
11 |
1º |
18 |
|
4 |
44 |
M |
Gunshot |
12C3.1 |
IIIC |
No |
12 |
4º |
24 |
|
5 |
17 |
M |
Fall |
12A1.3 |
No |
No |
12 |
2º |
12 |
|
6 |
29 |
M |
Fall |
12A2.3 |
No |
No |
12 |
4º |
18 |
|
7 |
49 |
M |
Car Accident |
12C3.3 |
No |
No |
12 |
2º |
24 |
|
8 |
30 |
F |
Car Accident |
12B1.2 |
No |
No |
10 |
5º |
12 |
|
9 |
51 |
M |
Fall |
12B3.2 |
No |
Delay |
20 |
1º |
12 |
|
10 |
23 |
M |
Fall |
12B1.3 |
No |
No |
10 |
2º |
12 |
|
11 |
46 |
F |
Car Accident |
12A2.3 |
No |
No |
12 |
1º |
12 |
|
12 |
31 |
M |
Gunshot |
12B3.3 |
IIIA |
No |
10 |
3º |
14 |
|
13 |
26 |
M |
Car Accident |
12C3.3 |
II |
No |
12 |
0º |
16 |
|
14 |
32 |
M |
Gunshot |
12B1.3 |
IIIA |
No |
10 |
3º |
18 |
|
15 |
24 |
M |
Gunshot |
12C3.3 |
IIIA |
No |
11 |
4º |
12 |
|
16 |
22 |
F |
Car Accident |
12B2.2 |
No |
No |
11 |
0º |
12 |
|
17 |
54 |
M |
Car Accident |
12B3.3 |
No |
Pain |
10 |
3º |
12 |
|
18 |
55 |
M |
Car Accident |
12B3.2 |
No |
Delay |
16 |
2º |
24 |
|
19 |
22 |
M |
Car Accident |
12C3.1 |
No |
No |
12 |
5º |
12 |
|
20 |
48 |
M |
Car Accident |
12B1.2 |
No |
No |
10 |
4º |
22 |
|
21 |
41 |
F |
Fall |
12A1.3 |
No |
No |
11 |
3º |
12 |
|
22 |
37 |
F |
Car Accident |
12C1.3 |
No |
No |
12 |
0º |
18 |
|
23 |
34 |
M |
Car Accident |
12C1 |
No |
delay |
18 |
3º |
16 |
|
24 |
56 |
F |
Fall |
12B3.3 |
No |
Praxia Radial |
12 |
2º |
12 |
|
25 |
34 |
F |
Fall |
12C2.2 |
No |
No |
11 |
3º |
12 |
|
26 |
28 |
M |
Fall |
12B1.3 |
No |
No |
10 |
2º |
14 |
|
27 |
33 |
M |
Car Accident |
12C2.2 |
No |
No |
12 |
5º |
12 |
|
28 |
22 |
M |
Fall |
12A2.3 |
No |
No |
11 |
4º |
12 |
|
29 |
30 |
M |
Fall |
12B2.2 |
No |
No |
12 |
2º |
12 |
|
30 |
28 |
M |
Car Accident |
12B2.3 |
No |
No |
11 |
5º |
12 |
|
31 |
29 |
F |
Fall |
12B1.2 |
No |
No |
12 |
3º |
12 |
|
32 |
21 |
M |
Car Accident |
12C2.3 |
No |
No |
12 |
2º |
12 |
Table 1 Demographics and radiological values
|
Case |
Elbow flexion |
Elbow extension |
Shoulder flexion |
Quick DASH |
VAS |
|
1 |
120° |
0° |
150° |
20 |
2 |
|
2 |
130° |
5° |
160 |
16 |
4 |
|
3 |
130° |
0° |
120° |
9 |
0 |
|
4 |
130° |
5° |
170° |
9 |
0 |
|
5 |
120° |
0° |
120° |
9 |
3 |
|
6 |
130° |
5° |
150° |
9 |
3 |
|
7 |
125° |
20° |
130° |
7 |
0 |
|
8 |
150° |
0° |
160° |
7 |
0 |
|
9 |
135° |
0° |
150° |
20 |
0 |
|
10 |
130° |
0° |
160° |
0 |
2 |
|
11 |
130º |
0º |
150 |
3 |
0 |
|
12 |
120 |
10º |
160º |
7 |
1 |
|
13 |
120 |
0º |
150° |
12 |
1 |
|
14 |
130 |
0 |
140º |
9 |
1 |
|
15 |
130 |
5 |
150 |
11 |
0 |
|
16 |
122 |
0 |
150 |
7 |
1 |
|
17 |
110º |
20º |
150º |
24 |
6 |
|
18 |
130º |
5° |
150º |
9 |
1 |
|
19 |
120º |
0º |
160º |
11 |
1 |
|
20 |
130º |
10º |
150º |
12 |
0 |
|
21 |
120º |
5° |
160º |
7 |
2 |
|
22 |
130º |
0º |
150º |
9 |
1 |
|
23 |
120º |
5º |
130º |
11 |
1 |
|
24 |
120º |
10º |
140º |
13 |
0 |
|
25 |
130º |
5º |
150º |
15 |
2 |
|
26 |
130º |
10º |
140º |
11 |
1 |
|
27 |
130º |
0 |
150º |
7 |
0 |
|
28 |
120º |
0º |
160º |
9 |
1 |
|
29 |
130º |
5º |
150º |
11 |
0 |
|
30 |
120º |
10º |
150º |
21 |
1 |
|
31 |
130º |
0º |
150º |
7 |
0 |
|
32 |
130º |
5º |
140º |
11 |
0 |
Table 2 Functional outcomes
The fracture was closed in 27 cases and open in five. The classification of the exposed fractures was made according to Gustillo-Anderson were presenting a case of type II, three of type IIIA and one of type III C.
The duration of the surgical procedure had an average of 76 minutes with a range of 60 to 120 minutes. The mean follow-up was 13,5 months with a range of 12 to 24. Radial nerve injury prior to surgery was present in eight patients out of 32 (25%), classified as a neurapraxia. The totality of patients recovered the function of the radial nerve in an average of 6 months.
Three patients presented other fractures associated between facial fractures, one case of poly trauma with fractures of the femur and distal radius and one case presented burns in the anterior region of the affected arm. The mean union rate was 12.1 weeks with a range of 10-20. There were no cases of non-union or reintervention. The average alignment in the anteroposterior axis was 2º.
Regarding the complications, three cases showed delayed union, two of them consolidated successfully at 16 weeks and the other case at 20 weeks without requiring reinterventions. One case presented praxia of the radial nerve in the postoperative period, which was recovered six months after the postoperative period. One case presented postoperative pain at the surgical site without requiring removal of the hardware one case presented a localized cellulitis associated with burns in the anterior region of the arm handled with antibiotic treatment. There were no cases of infection of the operative site off loss of fixation. Heterotopic ossification occurred in one case without impaired functionality.
All patients were fully evaluated one year after surgery. The mean elbow flexion was 124°, the average extension of the elbow was 3°. The mean shoulder flexion was 150°. On the VAS score scale, the average was 1 with a range of 0 to 6. The average of the abbreviated DASH score was 11(Range 0-25).
Surgical treatment for diaphyseal fractures of the distal humerus in its distal portion is the management standard5. Minimally invasive techniques have been gaining popularity, allowing the avoiding extensive dissection and disruption of vascularity and access to the fracture site, showing adequate functional outcomes.6–12
Gallucci et al.10 their series of 15 patients using a minimally invasive posterior approach reported successful union rates in 100% of the patients and a case of radial nerve apraxia that recovered completely, however, most patients presented fractures of the middle third. Ziquan12 evaluated the functional outcomes in a group of 13 patients with fractures of both the middle and distal third of the Humeral shaft and a minimally invasive technique through the anterior approach, finding union in 100% of the cases without presenting radial nerve palsy associated with the surgical technique. Balam et al.13 Show a series of 37 patients with fractures of the distal diaphysial humerus and of the middle third with a minimally invasive technique by posterior, presenting complete union rates with two cases of postoperative radial nerve neuropraxia that recovered satisfactorily. Gallucci13 shows again the advantages of the posterior approach specifically in patients with compromise of the distal third of the humerus; his series of 21 patients presented successful consolidation in 100%, recovery of functional mobility arches and adequate DASH and Constant scale results, with a single case of radial apraxia that recovered spontaneously.14,15
The results of this series of cases show us how the posterior minimally invasive technique with an anatomical implant is a good choice for the management of fractures of the distal humeral shaft, providing safety when performing direct control of the radial nerve, presenting low rates of complications. With complete control of the alignment in the anteroposterior plane and allowing technical skills and better distal fixation with the type of humerus plate used.
None.
The authors declare there are no conflicts of interest.
None.

©2020 Sánchez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.