MOJ
eISSN: 2374-6939


Research Article Volume 14 Issue 3
1Junior Resident, Department of Orthopaedic Surgery, JN Medical College, India
2Assistant Professor, Department of Orthopaedic Surgery, JN Medical College, India
3Professor, Department of Orthopaedic Surgery, JN Medical College, India
Correspondence: Yasir Salam Siddiqui, Assistant professor, Department of Orthopaedic Surgery, J. N. Medical College, Faculty of Medicine, A.M.U., Aligarh, Uttar Pradesh, India, Tel +919837343400;
Received: March 30, 2022 | Published: May 22, 2022
Citation: Dhakshanamoorthy R, Siddiqui YS, Abbas M, et al. Management of tibial plateau fractures with special reference to column classification. MOJ Orthop Rheumatol. 2022;14(3):58-63. DOI: 10.15406/mojor.2022.14.00579
Objective of the paper is to evaluate the outcome of the management of tibial plateau fractures with reference to Luo’s three column classification concept. The selection of surgical approach and appropriate fixation construct was dictated by the number of distinct articular fragments on CT scans and the concomitant soft tissue injury. The primary outcome measure was to evaluate the relationship between the number of column involved and fixation construct on secondary loss of reduction at healing. Secondary loss of reduction was defined as a change of alignment of ≥ 5 degrees into either varus or valgus at union. The secondary outcome measures were delayed union, non-union, peri-implant fracture and infection rates. Functional outcome were evaluated using Knee Society Score. Forty-six patients were available for final follow up. Immediate postoperative mal-alignment was noted in 5 patients. For our primary outcome measure, we have one patient with secondary loss of reduction at final follow-up in double plating group. Secondary outcome measures showed non-union in 1 (2.17%), delayed union in 3 (6.52%), superficial infection in 3 (6.52%) and deep infection in 1 patient (2.17%). No peri-implant fracture was seen. The mean time for bone healing and full-weight bearing walk was 14.5 weeks. The mean range of motion of the affected knees was 2.39 to 131.27 at final follow-up of 12 months. In sight of the findings of our study along with existing literature Luo’s three column classification is an ideal classification in managing tibial plateau fractures as it dictates the appropriate fixation construct based on the number articular fragments. However it does not take into account the integrity of soft tissues, which is almost universal association with high velocity complex tibial plateau fractures. Hence, repercussions of use of fixation construct with multiple plates will unfold in future with long follow-up comparative studies addressing the bony as well as soft tissue complications.
Keywords: tibial plateau, column classification, fixation constructs, secondary loss of reduction, non-union, infection
Tibial plateau fractures are high-energy injuries, often associated with significant soft tissue compromise. Optimal management of both bone and soft tissue component of the injury is of utmost importance for achieving good outcome. Management of tibial plateau fractures have witnessed a significant change in last two decades with the prototype shift from conventional orthogonal radiological centered management to CT based management, particularly of articular depression and shear fracture patterns. Shear fracture patterns and articular depression are not clearly delineated on conventional plain radiographs, often leading to incomplete planning and consequent sub-optimal outcome.1,2 Therefore, careful evaluation of fracture geometry on CT scan and thus planning accordingly is endorsed in recent studies.1–7
Luo proposed a comprehensive three column classification based on multi-planar CT which not only guides the surgeon in selecting the correct surgical approach but also in selecting the appropriate fixation construct.1 Currently, Luo three column classification is preferred over the Schatzker’s and AO/OTA classifications in management planning for achieving optimal outcome.1,2,8–10 Hence, we conducted a prospective study to evaluate the outcome of the management of tibial plateau fractures with reference to Luo’s three column classification concept.
Study design
This is a prospective study of the management of tibial plateau fractures with reference to three column classification concept of Luo.1. The duration of study was two years extending from November 2017 to October 2019. Fractures were classified using Luo’s column classification system.1 The study was approved by the institutional ethical committee. Informed consent was obtained from all the patients. The study was performed according to the ethical standards of the 1964 Declaration of Helsinki as revised in 2000.
Inclusion and exclusion criteria
We included all skeletally mature (≥18 years) patients having tibial plateau fractures with a minimum follow-up of 12 months. Closed as well as compound grade I and II fractures were included.11 Pathological fractures, compound grade III fractures, skeletally immature patients (< 18 years), polytrauma patients and tibial plateau fractures associated with neurovascular compromise or compartment syndrome were excluded from the study.
Management protocol
All the patients with tibial plateau fractures were hospitalized and evaluated for soft tissue injury including bruises, swelling, blisters and features of compartment syndrome. The anteroposterior (AP) and lateral radiographs of the knee with leg were performed. Computerized tomography scan was done to classify the fracture as per the Luo’s column concept. All X-rays and CT scan were assessed to define whether inclusion criteria were met, followed by a detailed case sheet evaluation to check for exclusion criteria. Patients were initially managed with long leg slab or skeletal traction on Bohler Braun splint. The decision for back slab or skeletal traction was based on soft tissue condition and fracture displacements. Skeletal traction was preferred in patients with soft tissue injury and gross fracture displacements. Surgery was undertaken only after the swelling had subsided and skin condition improved (appearance of wrinkle sign). In our study, selection of surgical approach and appropriate fixation construct (single or multiple plates with or without cancellous screws) was dictated by the number of distinct articular fragments on CT scans of the proximal tibia and the concomitant soft tissue injury. We took soft tissue condition also for selecting the appropriate fixation construct in addition to the distinct articular fragments. Thus, we formulated a specific selection criterion for fixation construct, based on fracture geometry and soft tissue status. The fixation construct selected was applied with a goal to minimize complications (bony as well soft tissues), allowing early knee range of motion and is sturdy enough to maintain the articular reduction and alignment throughout bony healing. Following groups were made based on the fixation construct:
1. Single plate group (lateral or medial plate)
2. Single plate with cancellous screw group (SP + CCS)
3. Dual plate group (DP).
Lateral column was approached via the conventional anterolateral approach and minimally invasive fixation technique was utilized. Medial column was approached via the conventional posteromedial approach as described by Lobenhoffer.12 Posterolateral fragment was approached via posterior approach. Per-op limb alignment was checked under image intensifier. Distinct fracture fragments were addressed by separate plate or cancellous screws along with elevation of concomitant articular depression. Decision to bone graft was at the discretion of the operating surgeon. Post-operatively early physiotherapy was encouraged, consisting of quadriceps strengthening and gradual knee bending exercises. Patients were allowed toe-touch weight bearing with walking aid for the initial 8 weeks followed by partial weight bearing. Unaided full weight bearing was allowed only after clinico-radiological union.
Radiological assessment
Immediate post-operative AP & lateral radiographs of leg including knee were assessed for quality of reduction. The quality of the initial reduction and its maintenance were assessed by the alignment measured immediately postoperatively and again at the time of fracture healing. An immediate postoperative mal-alignment was defined as a varus or valgus alignment of 5 degree or more on the initial postoperative films.13,14 Secondary loss of reduction was defined as a change of alignment of ≥5 degrees into either varus or valgus at union.15 Radiological union was defined as bridging callus on at least three of four cortices on AP and lateral radiographs. Functional outcome were evaluated using Knee Society Score at final follow-up.16
Outcome measures
The primary objective of the study was to evaluate the relationship between the number of column involved and fixation construct on secondary loss of reduction at healing. The secondary objectives were delayed union, non-union, peri-implant fracture and infection rates (superficial and deep). Deep infection was defined as the infection requiring operative debridement for control of infection.
Statistical analysis
All statistical analysis was done using Microsoft office 2010. The calculation of averages and standard deviation was done using data analysis tool. Unpaired t test was used for continuous variables, whereas for categorical variables Fisher’s exact test was used. A P value of < 0.05 was considered to indicate statistical significance.
Study population and demographic characteristics
During the study period 60 tibial plateau fractures presented to our institute. Patients were assessed and evaluated clinico-radiologically. Forty eight patients met the inclusion criteria whereas 12 patients were excluded from the study (polytrauma=5, compound grade III fractures=3, skeletally immature=2, vascular injury=2). Out of 48 patients, two patients were lost during follow-up evaluation. Finally 46 patients (28 SP, 5 SP + CCS and 13DP) were available for assessment. Patient demographics and operative details are shown in Table 1. Among these 46 patients, there were 38 males and 8 females. Road side accidents were the mode of injury in majority of patients (n = 37) followed by domestic falls (n = 5) and fall from height (n = 4). Right knee was injured in 28, while left in 18 patients. Mean age of patients was 48.4 years (range 19 to 62 years). Thirty six fractures were closed, while 10 patients had open fractures.
Total no. of patients available for final follow-up |
46 |
Male : Female Ratio |
38:8 |
Mode of injury |
Road Side Accident = 37 |
Domestic falls = 5 |
|
Fall from height = 4 |
|
Mean Age |
48.4 years (Range 19 – 62 years) |
Closed : Open fracture |
36:10 |
Right : Left knee involvement |
28:18 |
Mean Follow-up |
14 months (Range 12 – 18 months) |
Mean duration of surgery |
105 minutes (range 90 min. to 140 min.) |
Mean length of Hospital stay |
7.5 days (Range 5 – 14 days) |
Table 1 Demographic and operative details of patients
Fracture classification and fixation construct
As per Luo’s three column concept, single column fracture n=20, two column = 11 and three column involvement was seen in 15 cases. As mentioned earlier, the selection of surgical approach and appropriate fixation construct (single or multiple plates with or without cancellous screws) was dictated by the number of distinct articular fragments on CT scans and the concomitant soft tissue injury. The fixation construct in our study cohort consisted of single plate in 28, single plate with cancellous screws in 5 and dual plating in 13 patients. Column classification, approach (es) and fixation construct is depicted in Table 2.
Column classification |
Type of column involved |
No. of patients |
Approach |
Fixation construct |
One column |
Lateral |
17 |
Lateral |
Lateral Plate alone |
Medial |
3 |
Medial |
Medial Plate alone |
|
Posterior |
0 |
|||
Two column |
Latera l + Medial |
9 |
Latera l + Medial = 2 cases |
Lateral + Medial plate = 2 |
|
Lateral = 6 cases |
Lateral Plate alone = 6 |
||
Lateral + Posteromedial = 1 case |
Lateral + Posteromedial = 1 |
|||
Lateral + Posterior |
0 |
|||
Medial + Posterior |
2 |
Posteromedial = 2 cases |
Posteromedial =2 |
|
Three column |
Lateral + Medial + Posterior |
15 |
Lateral = 5 cases |
Lateral Plate + CCS = 5 |
Lateral + Medial = 8 cases |
Lateral + Medial = 8 |
|||
Lateral + Posteromedial = 2 cases |
Latera l+ Posteromedial = 2 |
Table 2 Column classification and fixation construct
Outcome measures and functional results
Immediate postoperative mal-alignment was noted in five patients (10.86%, varus ≥ 5 degrees). In other words acceptable reduction was achieved in 89.14% of the patients. For our primary outcome measure, we have one patient with secondary loss of reduction at final follow-up in double plating group (Figure 2). Secondary loss of reduction was defined as a change of alignment of ≥5 degrees into either varus or valgus at union.
Secondary outcome measures showed non-union in 1 (2.17%), delayed union in 3 (6.52%), superficial infection in 3 (6.52%) and deep infection requiring revision surgery with removal of implant for control of infection in 1 patient (2.17%). No peri-implant fracture was seen. Hardware removal was done in 4 (8.69%) patients owing to hardware irritation. The mean time for bone healing and full-weight bearing walk was 14.5 weeks. The mean range of motion of the affected knees was 2.39 to 131.27 at final follow-up of 12 months. The mean Functional Knee Society Score at 3 months, 6 months and 12 months was compared between columns 1, 2 and 3 using the one-way ANOVA test with post-hoc bonferroni test for inter-group comparisons. The mean Functional Knee Society Score at 3 months was significantly more among column 1 than columns 2 and 3. The mean Functional Knee Society Score at 6 months was significantly more among column 1 compared to column 3 which was significantly more than column 2. At later follow ups it was found to be not significant in our study population.
Tibial Plateau fractures are usually high energy injuries involving young adults, majority resulting as a consequence of road side accidents (80.43%), as was observed in our study.17 In our study, the mean age was 48.4 years, affecting primarily males. Severe soft tissue compromise is commonly accompanied with high energy tibial plateau fractures, which must be taken into contemplation while plotting out the management plan. Literature dictates staged management for achieving optimal outcome of both bone and soft tissue component of the injury as it allows settling of soft tissue injury, and consequent definitive management.2,18,19 In our study, the mean interval between injury and surgery was 6.4 days and most of the cases were initially managed either with back slab or skeletal traction. Open fractures (n=10) were debrided at presentation. Earlier studies have reported a mean time to surgery of 9.2 days.20 and 8.5 to 9 days.21 Our mean interval between injury and surgery was less as compared to previous studies due to inclusion of compound fractures in the study, which underwent debridement at presentation followed by definite treatment as per the study protocol.
Management of tibial plateau fractures have evolved over the last two decades with the advancements in implant design, fixation construct based on fracture personality and utilization of surgical approaches to optimally deal with the soft tissue and bony component of injury simultaneously. The major advancement is change from radiological centered management to CT based management, especially of the shear fracture patterns and articular depression for obtaining good outcome.1,2
Fracture reduction vs fixation construct
Our study highlights the utility of fixation principles based on column classification in treating tibial plateau fractures, with achievement of reduction and its maintenance at healing (Figure 1). In our study, immediate postoperative mal-alignment was noted in five patients (10.86%, varus > 5 degrees). Among these five mal-alignment cases one case was from single column fracture and two cases each from two and three column fractures. However, there were no significant differences in the incidence of immediate postoperative alignment regardless of fracture pattern or type of fixation. This suggests that we were able to achieve an acceptable reduction in 89.14% of the patients regardless of the technique chosen or method of fixation used. This was in concordance with the study performed by Weaver MJ, which concluded that immediate post-operative alignment was not related to the fixation construct.14 The mal-reduction in our study is comparable to the results published in earlier studies. Barei20 and Grosling22 reported 10% and 23% incidence of immediate post-operative mal-alignment in their studies respectively.
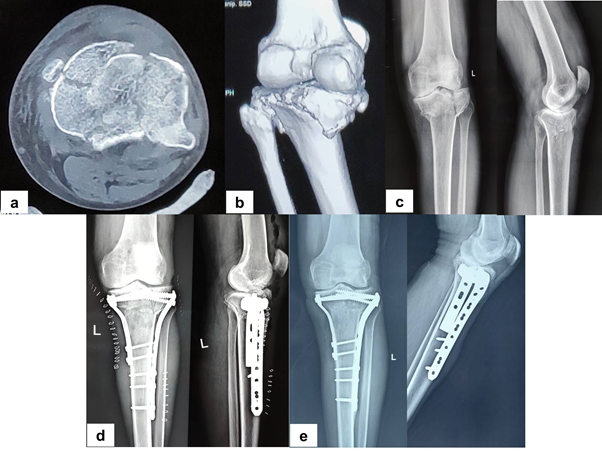
Figure 1 a & b) Pre-operative CT showing Luo’s three column fracture. c) Plain radiograph of the patient showing bicondylar fracture with coronal split. d) Post-operative radiograph showing acceptable reduction and alignment. e) Radiograph at healing with maintenance of reduction and alignment.
Secondary loss of reduction
In our study varus collapse was seen in one patient (2.17%, Figure 2), measured in terms of change in medial proximal tibial angle (mPTA ≥5 degree). Prior to three column classification, only few studies hypothesized that lateral construct alone may not be as effective as double plating construct in preventing secondary loss of reduction at healing.13,23 Certain biomechanical studies comparing fixation methods for tibial plateau fractures have demonstrated a slight superiority of dual plating over lateral locked plating with respect to both subsidence and cumulative load to failure with repetitive loading.22,24 Other studies have not shown a significant difference.25 Weaver MJ in 2011 evaluated the relationship between fracture pattern and fixation construct with secondary loss of reduction at healing.14 They concluded that in most of the patients with bicondylar tibial plateau fractures with fracture line in sagittal plane, lateral plate alone is as effective as dual plating in maintaining reduction and alignment at healing. Conversely, bicondylar fractures with coronal split, treated with lateral plate alone, showed higher rate of loss of reduction and alignment at healing. Analogous to Weaver MJ, our study also supports that lateral construct alone perform well in fracture patterns with no medial fracture line or a non-coronal fracture line. In nut shell, the column classification emphasizes upon for exactly delineating the fracture geometry, especially of the medial condyle in tibial plateau fractures, by using 3-D CT scans, as the plain radiographs fails to delineate the exact fracture geometry. CT scans clearly outlines the fracture geometry along with the principal fracture lines, thus differentiating the coronal shear fragment from the sagittal one.1,2, 1 The orientation of the principal fracture lines on CT scan (coronal vs sagittal) governs the fixation construct. However, the concomitant soft tissue injury should also be taken into consideration while planning the treatment. Hence we used postero-medial plate in cases with coronal split to buttress the fragment in addition to the lateral plate. In cases of sagittal orientation of fracture line of the medial fragment, cancellous screws along with lateral plate were used to fix the fragment, so as to prevent further soft tissue damage to already traumatized soft tissue envelop. Our approach is in accordance with Weaver MJ.14 However, Trikha V emphasizes on dual plating in all cases where postero-medial fragment is present.2 Neogi DS also opined that a single lateral plate may not hold the medial fragment effectively and may lead to loss of reduction and alignment.21 Table 3 compares the incidence of loss of reduction and alignment at healing, as reported in literature.
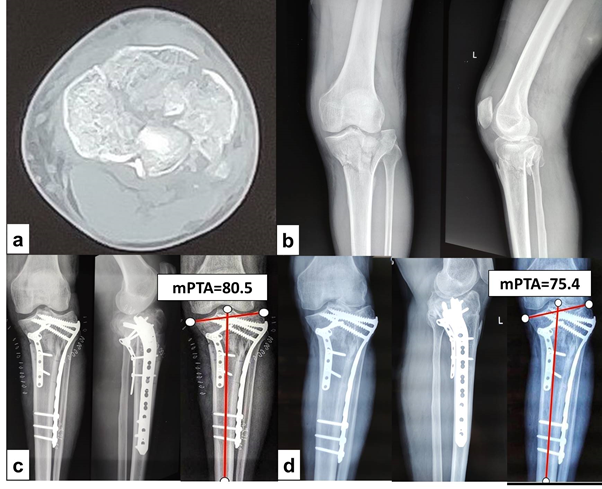
Figure 2 a) Pre-operative CT showing Luo’s three column fracture. b) Plain radiograph of the patient showing depressed bicondylar fracture with coronal split. c) Post-operative radiograph showing acceptable mPTA of 80.5 degrees. d) Radiograph at healing showing secondary loss of reduction (varus collapse) with change of mPTA ≥ 5 degrees. The mPTA at healing was 75.4 degrees.
Study |
No of patients |
Loss of alignment/varus collapse |
Cong Feng Luo et al.22 |
287 |
Nil |
Florence Unno et al.23 |
101 |
3 (2.9%) |
Hong Wei Chen et al.24 |
39 |
Nil |
Barei et al.25 |
83 |
2 (2.4%) |
Devdutta Neogi et al.17 |
61 |
5 (8.2%) |
Gosling et al.18 |
68 |
9 (13.2%) |
Jiang et al.26 |
84 |
3(3.57%) |
Our Study |
46 |
1 (2.17%) |
Table 3 Literature review comparing the incidence of secondary loss of reduction
The delayed union was seen in 3 (6.52%) and infected non-union in one (2.17%). For controlling deep infection we have to remove the implant before fracture union and consolidation (Figure 3). Hence the patient landed into non-union. Patient was offered revision surgery, which was not done because of patient refusal for revision surgery. The superficial infection rate (6.52%) and deep infection rate (2.17%) in our study was comparable to earlier studies.2,20,21 Literature quotes 23 to 88% infection rates with double plate osteosynthesis through a single extensile incision, while it drops down to 4.7 to 8.4% with the dual-incision double plating technique.31,32 Furthermore, with LISS fixation, it is reported to range from 0% to 22%.31, 33,34
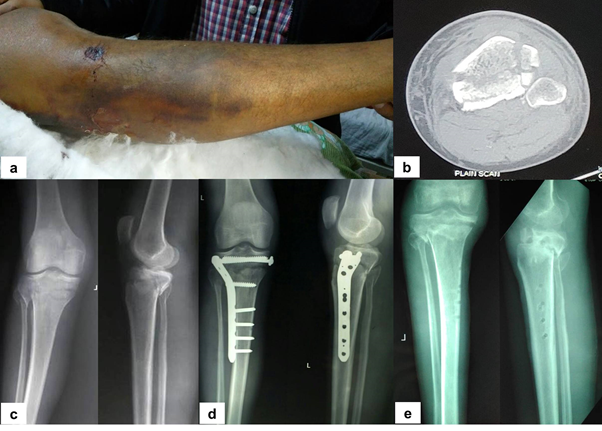
Figure 3 a) Clinical photograph of the knee with leg, showing severe soft tissue injury. b) Pre-operative CT showing Luo’s three column fracture. c) Plain radiograph of the patient showing bicondylar fracture with coronal split. d) Post-operative radiograph showing acceptable reduction and alignment with fixation construct consisting of lateral plate and medial screw. Severe soft tissue injury prevented us from utilization of fixation construct consisting of multiple plates, as per Luo’s column fixation concept. e) Radiograph after debridement and removal of implant for eradicating deep infection. Also note development of non-union as a consequence of removal of implant for controlling deep infection before fracture union and consolidation.
In our study, the patient who developed infected non-union was having three column fracture (Schatzker’s type 5), sustained injury due to high velocity trauma (motor vehicle accident). Patient was having extensive soft tissue damage. Although we have fixed the fracture with single plate along with cancellous screw, even then patient developed deep infection which required debridement and removal of implant. This case in our study emphasizes the need for addressing the soft tissue envelop optimally and if required utilizing the other modalities of fixation of complex tibial plateau fractures associated with severe soft tissue injuries.35 Morris in 2013, based on his observations also suggested that Schatzker’s type V & VI fractures have a significant autonomous effect on development of deep infection,36 as was seen in our patient. The concept that fracture type could reflect the severity of soft tissue injury to a certain extent is also supported by few other studies.32,37 We believe that the timing and method of definite fixation of the fracture is the key to reduce infection rate and soft tissue complications.
Luo’s column specific fixation is the best treatment approach for tibial plateau fractures, as the classification is simple and dictates the fixation construct by identifying the number of articular fragments. The classification has led to use of multiple plates for fixation of complex tibial plateau fractures. The repercussions of the use of multiple plates on infection rates, soft tissue complications, implant irritation cannot be ignored and will better evolve in future. Nevertheless, Luo’s classification is the ideal one for managing tibial plateau fractures, especially the coronal shear fragment.
Strengths, limitations and future recommendations
Our study highlights the utility of fixation principles based on column classification in treating tibial plateau fractures, with achievement of reduction and its maintenance at healing. The strengths of the study are prospective nature of study, use of single classification (Luo’s three column classification) for classifying fractures and definite treatment protocol based on distinct articular fragments and concomitant soft tissue injury. However small sample size, short follow-up and lack of comparative groups are the limitations of current study. Future studies with long follow-up are required for delineating the onset of occurrence of secondary osteoarthritis and its clinical significance in managing complex tibial plateau fractures.
Luo’s three column classification is an ideal classification in managing tibial plateau fractures as it dictates the appropriate fixation construct based on the number articular fragments. However it does not take into account the integrity of soft tissues, which is almost universal association with high velocity complex tibial plateau fractures. Hence, repercussions of use of fixation construct with multiple plates will unfold in future with long follow-up comparative studies addressing the bony as well as soft tissue complications. Hence we recommend further studies for establishing superiority of 3-column concept in managing tibial plateau fractures, especially the complex ones associated with severe soft tissue injuries.
None.
The authors declare no conflicts of interest.

©2022 Dhakshanamoorthy, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.