MOJ
eISSN: 2374-6939


Mini Review Volume 13 Issue 5
1Prof. Ph.D, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Kurgan
2Prof. DG, BIRDEM (Bangladesh Institute of Research and Rehabilitation in Diabetes, Endocrine and Metabolic Disorders), Bangladesh
3Dr. Md. Shahidul Islam, MD; FCPS, Prof., Bari-Ilizarov Orthopaedic Centre, Bangladesh
4Dr. Mohammad Tanvir Ashraf, D(Ortho), MS (Ortho), Consultant, Orthopaedics, NITOR, Bangladesh
5Dr. A.M. Shayan R. Bari, Medical officer, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Bari MM, Bari-Ilizarov Orthopaedic Centre, 1/1, Suvastu Shirazi Square, Lalmatia Block E, Dhaka-1207, Bangladesh, Tel +8801819211595, Tel +8801819211595
Received: September 10, 2021 | Published: September 28, 2021
Citation: Bari MM, Quayyum CMKI, Shahidul I, et al. Management of diabetic foot ulcer & atherosclerosis using tibial transverse bone lengthening technique; Bangladesh experience. MOJ Orthop Rheumatol. 2021;13(5):99-104. DOI: 10.15406/mojor.2021.13.00557
Diabetic foot ulcers (DFU) are chronic skin ulcers associated with deep tissue destruction around the foot and ankle region with varying degrees of lower extremity vasculopathy and neuropathy. Diabetic foot ulcer is associated with a high rate of morbidity, disability, mortality and psycho-social cost.
Keywords: DFU, TTT, Osteotomy, ulcer, gangrene
Diabetic foot ulcer (DFU) is always associated with peripheral and automatic neuropathy that prevents with red swollen foot. We can easily identify clinically by seeing the presence of ulceration in the foot. The diabetic foot ulcer with deformity depends on some factors which includes osseous mal-alignment, trauma, metabolic abnormalities, and osteoporosis. The loss of vasomotor control permits vasodilatation that leads to increase peripheral blood flow, which increases arteriovenous shunting that causes bone resorption. Obesity and muscle atrophy do not allow the patient to bear weight. Sometimes osseous projections are the potential areas for diabetic foot ulcer. Osteomyelitis should be ruled out with ulcer. Infectious, ulcers and bone resorptions are always integrated. Dorsal and planter ulcers are very much common in diabetic foot. Medial column ulcers are associated with tarsometatarsal medial column collapse. Lateral column ulcers are more proximal to mid foot deformity that does not unite. Chronic ulcerations lead to deep infection and osteomyelitis. Surgical intervention and debridement are essential to remove all devitalized tissue.1,2
As an excellent treatment for diabetic foot ulcers our study at Bari-Ilizarov Orthopaedic Centre and BIHS (Bangladesh Institute of Health Science) showed that 50% DFU are Wagner type lll.
Ilizarov’s law of tension-stress promotes formation of
Kurgan evidence suggests that Tibial Transverse Technique may mobilize stem cells and helps in formation of mesenchymal stem cells towards damaged tissues.
The Wagner diabetic foot ulcer classification system assesses ulcer depth and the presence of osteomyelitis or gangrene by using the following grades:
Principles of debridement for diabetic foot ulcers:
Protocols for tibial transverse technique surgery - Basic requirements
We must have indications and contraindications for TTT.
Indications:
Contraindications
Mentally ill patient who cannot assist the orthopaedic surgeon during treatment.
A small 5 incisions were made at the anterolateral part of the tibia. The distance between two incisions are 2cm. Through each 5 incisions a 5mm osteotome is used to do the osteotomy so that we can osteotomize the incised tibia in a colinear fashion. In the proximal incision we should cut the bone 2cm transversely. After that below each incision’s osteotomy 1.8mm 5 olive wires were introduced to connect with lateral plate via slotted bars. The tibial section has been moved approx. 1 mm/day for 3 weeks. The clinical status improved within a few weeks. Cure of trophic ulcers and no more pain. Arteriogram on the 2nd months improved circulatory result.3–7
The diabetic foot ulcer under the great toe and little toe are seen in most of the cases. Pre surgery color duplex confirmed the extrusive occlusion of anterior tibia, posterior tibia, and anteria dorsalis pedis. After surgery with 5 days of interval we started distraction of the osteotomised bone with the plate. Tibial section has been moved approximately 1 mm per day for 3 weeks. The clinical condition improved in 3 weeks and cure of diabetic foot ulcer were seen.
Postsurgical management
Recent advances (Diabetic foot ulcers)
Ilizarov discovered distraction histoneogenesis for limb regeneration. The tension-stress law could activate and enhance the regenerative potentials of living tissues, leading to growth or regeneration of muscles, fascia, blood vessels, and nerves simultaneously.
Clinical outcome of 58 cases of diabetic foot ulcers following Tibial Transverse Technique (TTT), bone lengthening
|
Total Cases |
58 |
|
Male |
46 |
|
Female |
12 |
|
Age (Years) |
35-72 |
|
Diabetes duration |
1-25 |
|
Foot Ulcer |
|
|
Duration |
3 days- 10 years |
|
Wagner Grading |
|
|
Grade ll |
25 |
|
Grade lll |
26 |
|
Grade lV |
06 |
|
Grade V |
01 |
In 2020, our study reported that 290 million adults worldwide had diabetes and it will rise to 450 million by the year 2035. This big demographic shift shows the prevalence of diabetes chronic complications in the foot. If we continue the conservative therapy the foot ulcers do not cure, surgical debridement, dressings, strict glycemic control and intravenous antibiotic therapy may eradicate infection but foot problems remain life threatening to the patient, that’s why we need to do distraction angiogenesis to increase microcirculation in the limb.
The Tibial Transverse Technique is based on Ilizarov's “law of tension-stress” for limb regeneration and functional reconstruction. The principle is slow and steady traction on a living tissue creates a stress and which is metabolically activated and which stimulates histoneogenesis”. It promotes cell division and differentiation of adult stem cells like that in the fetal tissues development and lead to tissue regeneration.1– 4

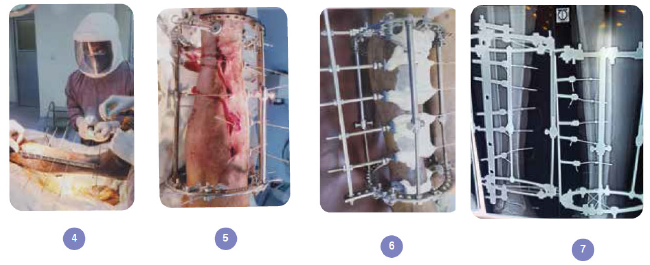

Figure 1 72 years old man, Diabetic Foot Ulcer with atherosclerosis.
(1) Diabetic foot of right little toe ulcer with dry skin.
(2) Dry skin of lower tibia and ankle.
(3) Radiograph of right foot with resorption of right 5th and 4th phalanges.
(4) In OR, multiple incisions and introducing the olive wires.
(5) In OR, long plate is fixing with the olive wires.
(6) View of Ilizarov fixation in the diabetic leg to increase vascularity.
(7) Radiograph of right foot with Ilizarov fixation, widening of tibia is seen.
(8) After 14 days of Ilizarov fixation in the right leg, little toe ulcer is healed.
(9) View of the leg with Ilizarov fixation, skin color changed and ulcer is healed after 21 days.
(10,11) Clinical appearance of the patient and right leg without ulcer.

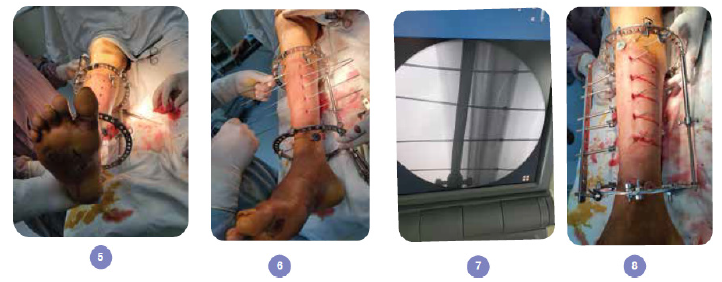



Figure 2 33 years old man, Diabetic Foot Ulcer with vasculopathy and neuropathy.
(1) Diabetic Foot Ulcer of dorsum of right foot, Wagner type III.
(2) Same patient, sole of the foot and dorsum of the great toe.
(3, 4) Dorsum and sole of the foot after debridement.
(5) In OR, multiple incisions seen in the tibia.
(6) In OR, placement of olive wires.
(7) Radiograph of right foot, placement of olive wires.
(8) Olive wires were connected through slotted bars and plate.
(9) Radiograph of distraction time.
(10) View of placement of Ilizarov apparatus for TTT (Tibial Transverse Technique).
(11) 14 days after the TTT surgery.
(12) After 21 days, ulcer is healed.
(13, 14) Radiograph of right tibia with Ilizarov fixation, ulcer is healed (AP and Lateral view).
(15) Before dismounting Ilizarov fixation, healed dorsum of the foot.
(16) Sole of the foot healed, before dismounting Ilizarov fixation.
(17) Radiograph after removal of Ilizarov apparatus.
(18-20) Final follow-up after 2 months without any ulcer.
None.
The authors declare no conflicts of interest

©2021 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.