MOJ
eISSN: 2374-6939


Research Article Volume 11 Issue 3
Orthopaedic Professor, Complexo Hospitalar, Brazil
Correspondence: Prof. Dr. Carlos Roberto Schwartsmann, Professor Titular Ortopedia e Traumatologia da Universidade Federal de Ciências Saúde Porto Alegre/RS - Chefe do Serviço de Ortopedia e Traumatologia da Santa Casa de Porto Alegre/RS - Chefe do Grupo de Quadril do Serviço de Ortopedia e Traumatologia da Santa Casa de Porto Alegre/RS, Brazil
Received: May 17, 2019 | Published: May 22, 2019
Citation: Schwartsmann CR, Spinelli LDF, Silva GSD, et al. Macroscopic analysis of the patella cartilage during total knee replacement. MOJ Orthop Rheumatol. 2019;11(3):125-128. DOI: 10.15406/mojor.2019.11.00485
Background: Knee osteoarthritis is diagnoses and monitored with radiography. Arthroscopy is considered the most valid method for evaluation of cartilage lesions. The best way for grading, measure and dimension is direct visualisation.
Methods: Patelar cartilage lesion was analysed macroscopically during 176 total knee replacement. The grading of cartilage lesion, by direct visualisation, indentified six diferents groups.
Results: Patellar articular cartilage was damaged in all 176 cases. There was no evidence of association between grade of arthrosis, gender, side or age. There is an association between tricompartmental arthrosis, varus deformity, obesity and grade of patelar arthrosis.
Conclusion: All classifications systems regarding the femoropatellar cartilage lesions are unrealistic. Important subchondral bone exposure occurred in 77,2% patelar articular surface.
Keywords: Patella, Femoropatelar joint, Patellar cartilage, Arthroscopy, Radiographic classification, Grading cartilage lesions
Knee osteoarthritis is commonly diagnosed and monitored with radiography. Intra-observer and inter-observer reliability of radiographic classification systems in this pathology are poor to moderate. When assessed arthroscopically, a wide range of inter-observer reliability is found. Probably the best way to classify what happens with the patellar cartilage is direct visualisation.
During 176 Total Knee Arthroplasties, the articular surface of the patella was analysed macroscopically and the degree of degeneration of the cartilage was graded. The study was prospective and occurred between April 2016 and August 2017. Femoropatellar replacement was not implemented in our cases. Osteophyte resection was achieved for articular surface regularization and anatomical reestablishment. Electrocautery denervation of the patellar edges was performed circumferentilly.1,2 The age of the patients ranged from 51 to 97 years with a mean and standard deviation of 70.1±7.8 years. In total, 140 patients (79.5%) were female and 36 (20.5%) were male. Right and left knees were compromised in the same proportion: 88 cases each. The body mass index (BMI) ranged from 18.4 to 46.2 kg/m2 with a mean of 30.3±4.8 kg/m2. Only 18 (10.2%) patients were considered normal based on BMI (18–24.9 kg/m2). BMI data were: overweight (25–29.9), 73 cases (41.5%); obese (30–39.9), 57 cases (32.4%); and severely obese or worse (IMC>35), 28 cases (15.9%). To radiographically grade osteoarthritis, we used the Kellgren-Lawrence3 scale: Grade III, 10 cases (5.7%); and Grade IV, 166 cases (94.3%).
Regarding axial deviation, only 3 cases were considered normo-axis (1.7%); 40 had genu-valgum (22.7%) and 133 had genu-varus (75.6%). Mean varus deviation was 10.2º±4.1º. Mean valgus deviation was 16.8º±6.8º. The anatomic tibiofemoral angle was determined with the use of the method described by Hsu et al.4 Overall, 170 cases had radiographic signs of tricompartmental arthrosis (96.6%) and there were 6 cases of bicompartmental arthrosis (3.4%). Transoperative patellar evaluation was obtained after exposure and eversion.
The classification was consensually performed by the surgeon and three assistants. We classified the articular surface in 6 different groups (Group I–VI):
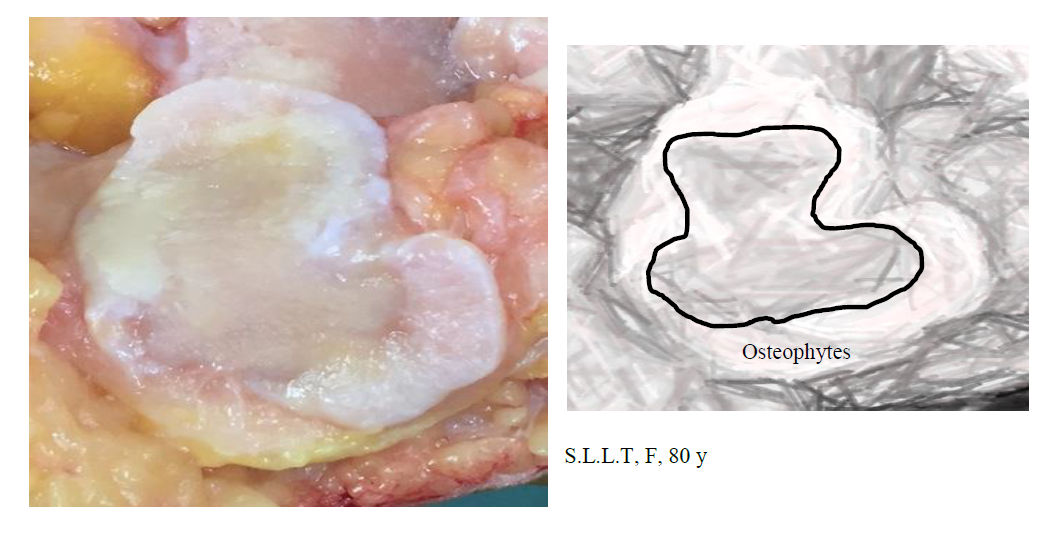
Group V: Erosion of more than 50% of the cartilage and osteophytes in more than 50% of the perimeter of the patella;
In all cases, some degree of cartilage damage was observed. Only one case was classified as Group I (0.6%), 18 as Group II (10.2%), 21 as Group III (11.9%), 42 as Group IV (23.9%), 50 as Group V (28.4%) and 44 as Group VI (25.0%). Combining the three more severe Groups of patients (IV, V and VI – erosion exposing the subchondral bone of more than 50% of the diameter of the cartilage), we identified 136 patients (77.2%). Statistical analysis was performed using SPSS (version 21), and Fisher`s exact test and Spearman’s correlation coefficient were used. This study was approved by the ethics committee of our institution.
With crossed analysis using Fisher’s exact test we concluded:
There was no evidence of association between grade of arthrosis and gender (P=0.261).
There was no evidence of association between grade of arthrosis and side (P=0.264).
The sample indicates that there is an association between varus deformity and grade of patellar arthrosis (P=0.019).
The sample indicates that there is an association between radiographic tricompartmental arthrosis and grade of patellar arthrosis (P=0.034).
Spearman’s correlation coefficient did not show a correlation between age and grade of arthrosis (P=0.119). However, we found a significant correlation between BMI and grade of arthrosis (0.010), indicating obesity as an important risk factor of patellofemoral arthrosis.
Osteoarthritis of the knee is a disabling disease, resulting in pain, joint discomfort, diminished function and restricted motion. Osteoarthritis is commonly diagnosed and monitored with radiography. Many radiographic classification systems are used in an attempt to confirm articular degenerative cartilage lesion with reliability. For knee osteoarthritis, the most widely used systems are: Kellgren-Lawrence,3 Ahlbäck,5 Fairbank,6 Brandt,7 and the international knee documentation committee (IKDC).8 Specifically for the femoropatellar joint, the Iwano9 and Merchant10 classifications are the most commonly used. All of these classifications had fair to moderate inter-observer and intra-observer reliabilities.11–16 However, analysing their correlation with cartilage status assessed arthroscopically, they showed only moderate inter-observer reliability.17–26 Many authors agree that radiographic images must be taken in orthostatic and monopodalic weight-bearing. Rosenberg radiographs had a higher correlation with arthroscopic findings of chondral disease than anteroposterior radiographs.27–29 Wright and MARS group, correlating osteoarthritis classification with arthroscopic articular cartilage findings, concluded that “IKDC classification assessed with use of 45º postero-anterior flexion Weight-Bearing radiographs had the most favourable combination of reliability and correlation’’.30–32 Of course, the best way to confirm articular cartilage degeneration is observing directly using arthroscopy.
The most commonly used scale in literature for femoropatellar evaluation is the Outerbridge classification,33 but this scale also has a wide range of inter-observer reliability.34–37 Cameron,38 in a cadaver-based study, concluded: “The Outerbridge classification was moderately accurate when used to grade chondral lesions arthroscopically”. Brismar,39 in a videotape study, concluded: “The arthroscopic grading of early osteoarthritic lesions is inexact”. Razak40 found a weak correlation between radiographic and arthroscopic findings in Asian osteoarthritic knees. Spahn,41 in a multicentre survey with 301 highly experienced arthroscopists, concluded that arthroscopy was not perceived to be as reliable as a “Gold standard” for the diagnosis of cartilage lesions.
The Outerbridge classification is very simplistic and is not a good parameter for deciding whether the patella will be replaced or not in total knee arthroplasty.
Grade 0: is normal articular cartilage,
Grade I: softening of the cartilage,
Grade II: fibrillation or superficial fissures,
Grade III: deep fissuring without exposed bone,
Grade IV: subchondral bone is exposed.
In our study, in all patients we found patellar cartilage lesions. Only 19 (10.8%) patellae were free of subchondral bone exposure (19/176). In 157 (89.2%) cases, the subchondral bone was exposed to different degrees. These findings corresponded to Grade IV in the Outerbridge classification. Exposed subchondral bone of more than 50% of patellar diameter (Grades IV,V,VI) was found in 136 cases (77.2%). All of these correspond to Outerbridge IV. When we considered the worst situation, almost all cartilage disappearance or flattening or inversion of the patellar triangle, we found 44 cases (25.0%). This indicates severe osteoarthritis. When analysing the mean age of this group (70.1 years), we recognise it as an elderly group, but we did not find a correlation between age and arthrosis degree (P = 0.119). Another important subject forgotten in the Outerbridge classification is the presence of marginal ostheophytes, especially in early stages. Kijowski et al.42 correlated the radiographic findings of osteoarthritis and arthroscopic findings of articular cartilage degeneration within the patellofemoral joint. They analysed the sensitivity for the presence of osteophytes, joint-space narrowing, subchondral sclerosis and subchondral cysts. The conclusion was “marginal osteophytes were the most sensitive radiographic feature for the detection of articular cartilage degeneration”. Osteoarthritis rarely occurred in the absence of associated osteophyte formation. For this reason, we considered it important to include osteophyte formation in our classification system. With extensively exposed subcondral bone and many osteophytes, more than 50% of the patellar perimeter, we considered it to be the more severe level (Grade V). In the worst scenario, patellar cartilage disappeared completely (Grade VI).
Analysing 176 patellar articular surfaces transoperatively in total knee arthroplasty, we concluded:

©2019 Schwartsmann, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.