MOJ
eISSN: 2374-6939


Case Report Volume 1 Issue 3
1University Hospitals of North Midland NHS Trust, UK
2New Cross Hospital, Royal Wolverhampton NHS Trust, UK
3Nottingham University Hospital, UK
Correspondence: Konstantinos Starantzis, Consultant Spinal Surgeon, University Hospital of North Midlands NHS Trust, Royal Stoke University Hospital, Old Yoo Restaurant, City General Site, Newcastle Road, Stoke-on-Trent, ST4 6QG, UK, Tel 1782679862, Fax 01782 679915
Received: October 30, 2014 | Published: November 13, 2014
Citation: Starantzis KA, Papanikolaou PD, Shafafy M. Is once failed back surgery, always failed back surgery? a relative success of surgical intervention in a patient with failed back surgery on intrathecal morphine pump. MOJ Orthop Rheumatol. 2014;1(3):68-70. DOI: 10.15406/mojor.2014.01.00018
Purpose: To present a case, previously been labelled as failed back surgery with Intrathecal Morphine Pump and yet successfully treated surgically through a far lateral approach.
Methods: A 54 years old man with a long history of complicated lumbosacral surgery on Intrathecal Morhpine Pump presented with worsening of back pain. Further investigations revealed adjacent level disease next to the previous fusion level. A far lateral approach was employed to perform a lumbar interbody fusion.
Results: The back pain significantly subsided soon after the surgery and the patient returned to his previous pain control regime. On the latest follow up, 2 years following surgery, he remained stable with regards of his symptoms with the IT morphine pump controlling the leg pain.
Conclusion: Patients with such devices should not be considered as non-surgical candidates by definition. New symptoms, correlating with possible surgical targets, could be tackled by novel techniques.
Keywords: Failed back syndrome, Intrathecal morphine pump, XLIF, Neuropathic pain, Chronic lower back pain, ITP
ITP, Intrathecal Morphine Pumps; IT, Intrathecal; BMI, Body Mass Index
Intrathecal Morphine Pumps (ITP) have been used for the treatment of chronic back and leg pain in patients that surgical intervention is not indicated. Implanted cord stimulators and intrathecal pumps, represent the last resort for pain control in carefully selected patients when non-surgical modalities have been exhausted.1,2 Patients with these devices, therefore, are generally considered as non-surgical candidates by definition. Is that true, or are there any indications to consider a re-referral to the spinal surgeon?
A 54 years old man with a long history of complicated lumbosacral surgery was referred from another centre to our spinal unit for a second opinion. This gentleman has had multiple posterior lumbar surgical procedures. It had started 25 years ago with a decompression and discectomy at L5/S1 level followed by the same procedure on L4/L5 2 years later. This time the surgery was complicated by a dural tear and surgical wound infection. He then underwent an instrumented L4/S1 posterolateral fusion using pedicle screws, which subsequently were removed on one side because of deep infection. He continues to suffer from back and leg pain and subsequently he was labelled as a case of Failed Back Surgery Syndrome.
When conservative modalities including multi-modal oral analgesia, interventional pain clinic, physical therapy and complementary techniques were exhausted, an intrathecal (IT) morphine pump was inserted. His pain was well managed for 8 years at a steady and stable dose to such an extend that he could hold a part time light job. However, his back pain then gradually became unmanageable despite increasing doses of morphine. One year later he lost his part time job and was referred to local spinal surgeons, who were very reluctant to offer any surgical innervation given the complicated spinal surgery he previously had and the fact that he had been labelled with Failed Back Surgery Syndrome. As the pain became worse, in desperation and in search of a second opinion, the patient was referred to our spinal unit.
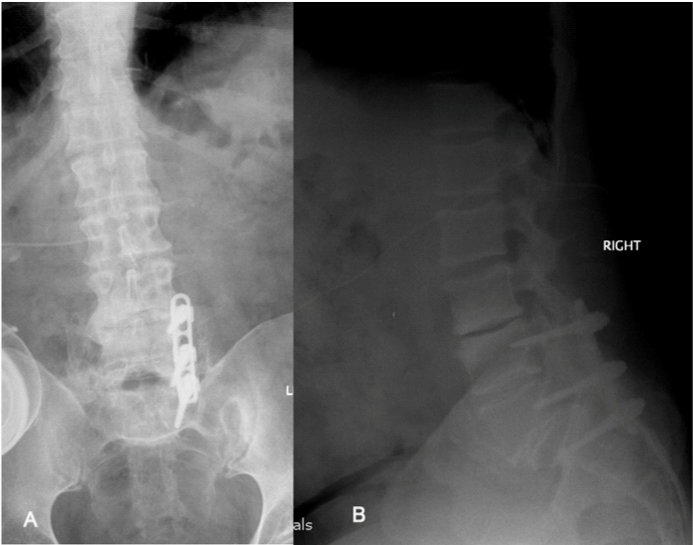
On presentation patient confessed and accepted the fact that he could never been pain free but stated on the top of his normal back and leg pain he had developed a much worse back pain just above his normal pain. He stated that the pain on his back had significantly worsened over the last 2 years as opposed to his leg symptoms that had remained unchanged. On examination, he was an obese gentleman with slightly positive saggital balance and a long posterior lumbar surgical scar. There was also an intrathecal morphine pump in his left loin. Neurological examination was unremarkable apart from knee reflexes been diminished bilaterally. Plain x-rays confirmed the presence of intrathecal catheter and implants were remaining intact and in situ and also demonstrated some evidence of L4-S1 bony fusion (Figure 1), which was further confirmed with CT scan. At L3-L4 level it demonstrated disc space narrowing and endplate sclerosis suggestive of adjacent segment disease requiring further imaging investigations. An MRI scan of the lumbasacral spine showed severe degeneration of the L3-L4 disc (adjacent level to previous fusion) with associated lateral recess stenosis impinging the left L2 and the right L3 nerve roots (Figure 2).

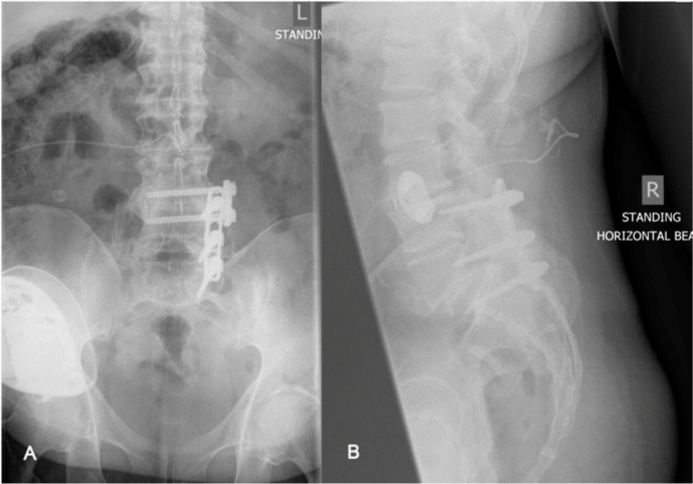
This was clearly a surgical target correlated with the patient’s symptoms and clinical findings. However, there were significant concerns about revision surgery through previous posterior approach because of previous complications; in particular deep infection for which part of the implants had been removed, albeit many years previously. Anterior surgery was not without significant risks because of his size. A relatively new but established technique, using trans-psoas approach via a small incision through loin was exploited. Through this approach, both aforementioned concerns were circumvented whilst it allowed discectomy and indirect decompression and fusion. It restored the lateral recess and foramina height, by restoring the disc height when an oversized cage packed with bone graft placed in the disc space after discectomy. This was then stabilised by a plate and two screws inserted parallel to endplates (Figure 3). The back pain significantly subsided soon after the surgery and the patient returned to his previous pain control regime. O.D.I. score decreased from 84 pre operatively to 46 six weeks post operatively and maintained at the same levels two years after this intervention. VAS back was 10 and 5 while VAS leg was 7 and 6 respectively. On the latest follow up, 2 years following surgery, he remained stable with regards of his symptoms with the IT morphine pump controlling the leg pain.
Failed Back Surgery Syndrome, also known as “Failed Back” or “Post Laminectomy Syndrome”, refers to persistent neuropathic pain after spinal surgery.3,4 Whether this is a misnomer or a redundant term, whether there are different types and causes of such clinical entity, requiring different types of treatment,3 is not going to be the subject of our debate. It is assumed that every patient that is on the chronic pain pathway does not have surgical target anymore and/or the surgical armamentarium has been tried and exhausted and failed. Such patients are assumed to have almost no potential to benefit from yet another operation hence non-surgical modalities are recruited.2 Pain specialist input is playing a crucial role for management of such difficult to treat patients.
When final step in analgesic ladder is reached without a satisfactory pain control and all other interventions including physical therapy complementary techniques5 are tried and failed, an IT morphine pump implant may be considered.2,6 Even in the presence of such device, co-medication with one or combination of different classes of analgesics may still be necessary. A favourable result and a satisfactory pain control is then expected for approximately 60-95% of these patients.6–10 When a patient whose pain has been satisfactorily controlled with such regimen for many years, as in our patient, suddenly starts to experience more pain out of character for his/her normal pain, differential diagnosis should include device related problems, drug tolerance or disease progression.6,10–13 Once the first two have been excluded, consideration for seeking spinal surgical opinion to investigate the third should seriously been considered. Disease progression in such circumstances, in general, includes development of post surgical instability, infection, mechanical failure of the implants or junctional problems. Junctional problems specifically can manifest themselves as accelerated disc and facet degeneration resulting in hyper-mobility of the motion segment or even instability with or without stenotic features. In our patient, the junctional problem presented itself with pain due to hypermobility as well as painful radicular symptoms due to lateral recess and foraminal stenosis. Both these pains in our patient were firstly different in character and location and secondly were over and above our patient’s normal pain for which he had had pain management and ITP.
Once this fact was established through taking a careful history thorough examination and appropriate investigation, surgical intervention was deemed reasonable. The patient was properly counselled about the potential risks and was warned about unrealistic expectation of being completely pain free afterwards. The aim was to get the patient’s pain to the level previously controlled with ITP.
Since the patient had undergone previous posterior lumbar procedures and had developed infection after one of them, going through the same surgical field was associated with high risk of infection and dural tear. Anterior lumbar surgery in this case was also not straight forward because of previous history of abdominal surgery and high BMI. To avoid that a more recent far lateral trans-psoas approach was therefore employed. To the best of our knowledge this is the first case to be reported, who had previously been labelled with failed back surgery with ITP and yet successfully treated surgically through far lateral approach.
None.
The author declares that there is no conflict of interest.

©2014 Starantzis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.