MOJ
eISSN: 2374-6939


Mini Review Volume 11 Issue 1
1Lecturer of Rheumatology and Rehabilitations, Egypt
2Lecturer of Radio diagnosis, Egypt
Correspondence: Shimaa M Abdelwhab, Lecturer of Rheumatology and Rehabilitations, Egypt
Received: July 17, 2018 | Published: February 28, 2019
Citation: Abdelwhab SM, Elsmmak AA. Imaging of musculoskeletal infection. MOJ Orthop Rheumatol. 2019;11(1):60-65. DOI: 10.15406/mojor.2019.11.00472
Musculoskeletal infection is commonly encountered in the rheumatology department1 appropriate imaging work-up of the various musculoskeletal soft tissue infections aids early diagnosis and treatment and decreases the risk of complications resulting from misdiagnosis or delayed diagnosis and can take many forms depending on the involvement of the various soft-tissue layers2 as shown as showed in Table 1.
Specific imaging features exist that help identify the numerous forms of infection in the bones and soft tissues.2
|
Anatomic Plane |
Infection |
|
Skin |
Cellulitis |
|
Fascia |
Infective fasciitis |
|
Necrotizing fasciitis |
|
|
Muscle |
Pyomyositis |
|
Bursa |
Spectic bursitis |
|
joint |
Spetic arthritis |
|
Bone cortex |
Infective osteitis |
|
Bone marrow |
Osteomyelitis |
Table 1
Risk factors of MSK INFECTION include: Vascular insufficiency, Soft-tissue ulcer (often secondary to diabetes), Immunosuppression, Foreign bodies and DM.3
Cellulitis is acute infectious process limited to the skin and subcutaneous tissues. Radiographic signs of soft tissue infection are generally nonspecific, Computed tomography (CT) and magnetic resonance imaging (MRI) with contrast enhancement can be more specific.4
Radiographic findings seen in Figure 1 is Non specific soft-tissue swelling and Obliteration of fat planes.
Computed tomography Cross-sectional imaging is Thickening of the skin and the septa in the subcutaneous tissue and occasionally, small fluid collections may be present in the sub dermal areas or superficial to the fascia. In practice: Diagnosed when Doppler is performed to rule out DVT (Figure 2).
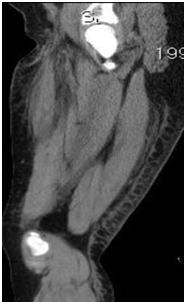
Figure 2 Sagittal CT of the thigh shows skin thickening posteriorly with thickened subcutaneous septa.
Necrotizing fasciitis
Fulminant form of septic fasciitis associated with rapid spread of infection and prominent tissue necrosis. Surgical emergency, so rapid and accurate diagnosis is important4 (Figure 3).
Abcess
Abscess may be simulated at imaging by necrotic tumors,myonecrosis due to severe trauma or extreme overuse, or ischemia (e.g., as can occur in patients with diabetes or sickle cell anemia).1
Radiographs7
Nonspecific soft-tissue mass
Gas bubbles or gas-liquid levels are visualized.
CT
Heterogenous fluid collection with thick irregular margins that enhance after the administration of intravenous contrast.
Inflammatory changes in the soft tissues adjacent to the abscess may lead to overestimation of its size.
CT is particularly useful for detecting gas present within the abscess cavity.
Both radiographs and CT can demonstrate retained foreign bodies that may be the cause of abscess
MRI
Soft-tissue abscesses have variable signal characteristics on MRI.
The typical abscess shows central areas of low signal intensity on T1-weighted (T1W) images and high signal intensity on T2-weighted (T2W) images.
Though the proteinaceous granulation tissue on the inner margin may show intermediate signal on T1W images.
The thick, irregular wall enhances after administration of intravenous gadolinium.
Adjacent soft tissue and skin inflammation are generally present (Figure 3B) (Figure 4).
Pyomyositis
Pyomyositis is pyogenic infection of skeletal muscle characterized by muscle swelling, and it frequently leads to abscess formation, which is a focal collection of inflammatory cells, bacteria, and necrotic tissue debris contained by hypervascular connective tissue.8 The buttock and thigh are the most commonly affected locations.
Appearance: The muscle is typically edematous, partially necrotic, and can contain multiple abscesses.9
Myonecrosis: Muscle infection with extensive gas formation due to myonecrosis, also referred to as “gas gangrene,”6 (Figure 5).
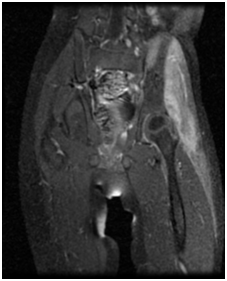
Figure 5 MRI of thighs. Coronal fat suppressed T1WI with contrast showing inhomogeneous muscular enhancement in keeping with pyomyositis.
Septic arthritis
Most joint infections are diagnosed clinically, without radiographs or other imaging. Joint aspiration is the gold standard test. However, imaging studies are sometimes requested.Joint effusion is the first radiographic sign of septic arthritis. With time, hyperemia may lead to periarticular osteoporosis.11
Predisposing factors10
Rheumatoid arthritis
Foreign bodies such as joint prostheses.
Pregnancy is an often overlooked risk factor. The increased laxity of the sacroiliac joints during pregnancy makes them prone to fluid accumulation and seeding during episodes of transient bacteremia
Children Vs adults11
In children, septic arthritis involves the large joints of the extremities and is typically hematogenous in etiology.
In adults:
The etiology is usually direct inoculation from penetrating trauma to hands and feet.
Hematogenous spread in adults is less common than direct inoculation, but when it does occur it typically involves the 5 “S” joints: sacroiliac joint, symphysis pubis, sternoclavicular joint, spine, and acromioclavicular joint (shoulder).
Major complications
Premature physeal closure
Premature osteoarthritis
Avascular necrosis
Osteomyelitis.
Radiographic findings
Very early: Particularly in young children whose joints are relatively lax, the joint space may be widened by a reactive effusion (Figure 6).
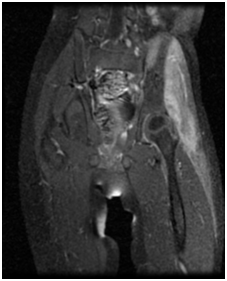
Figure 5 MRI of thighs. Coronal fat suppressed T1WI with contrast showing inhomogeneous muscular enhancement in keeping with pyomyositis.


Figure 6A Plain x-ray of the pelvis in a case of early septic arthritis showing mild widening of right hip joint space.
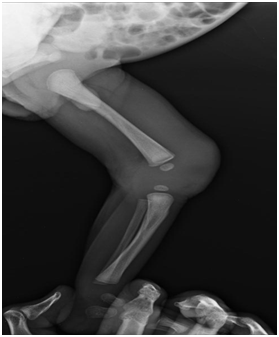
Figure 6B Plain x-ray of the knees in a case of septic arthritis showing soft tissue swelling and increased density at left knee joint.
Radiographic findings
Later:
Joint space narrowing secondary to cartilage destruction and osseous erosions are identified.
Joint-space loss is uniform and is not accompanied by sclerosis or productive bony changes, features which help differentiate infection from degenerative arthropathy (Figure 7).
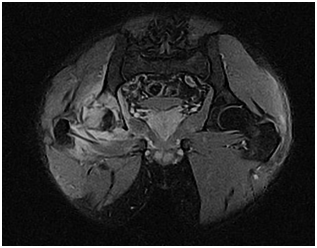
Figure 7 Coronal MRI of the pelvis fat suppressed T1WI: Diffuse marrow edema within the right femoral head and neck, as well as the acetabulum which extends to involve AIIS. There is destruction of the posterosuperior femoral head and adjacent acetabulum. A large joint effusion is present. Para-acetabular muscle edema is noted which involves the gluteal muscles most severely.
TB Arthritis
Tuberculosis arthritis are more chronic processes than bacterial arthritis. Therefore may elicit little or no host bone reaction. Cartilage destruction is often much slower and joint space width remains normal and may demonstrate osteoporosis with minimal cartilage destruction. Erosions are slow to progress and may appear particularly well delineated.12
Radiographic findings include phemister’s triad
Ill-defined erosions
Profound osteoporosis
Relative preservation of joint space till late (Figure 8)
Rice bodies13
Thickened areas of synovial proliferation, typically detached from the underlying synovium
Characteristic appearance on MRI, appearing as 5 mm to10 mm elongated fragments shaped like rice kernels, with intermediate T1W signal and low signal on T2W images (Figure 9).
Osteomyelitis
Infection of bone or, more precisely, bone marrow. Infection of bone may be caused by hematogenous seeding, penetrating injury, or surgery, or contiguous spread from an adjacent joint or soft tissue infection. A direct penetrating injury or adjacent infection can result in osteomyelitis at any site. Infection by contiguous14 spread begins with infection of the periosteum (truly, periostitis), followed by infection of the cortex (osteitis), then infection of the marrow cavity (osteomyelitis).15
Acute osteomyelitis imaging characteristics: 15
Radiographs
Radiographic findings of acute osteomyelitis are typically not present for 7 to 14 days following the onset of infection.
The early radiographic manifestations of osteomyelitis consist of:
Permeative osteolysis
Endosteal erosions
Intracortical fissuring
Periostitis.
Differential diagnosis: Ewing sarcoma, aggressive neoplasm or Stress fracture (Figure 10).
Late radiographic findings: destruction
CT16
Insensitive for early marrow infection.
More sensitive than radiographs for detection of early periostitis and trabecular or cortical erosion.
Nuclear medicine
Technetium-99m methylene diphosphonate, either alone or in conjunction with Gallium-67 or Indium-111 labeled leukocytes.
Scintigraphy is more sensitive for early osteomyelitis.
Findings
Abnormal increased uptake on all 3 phases, with increasing activity on the delayed images.
Gallium and Indium scanning are adjunct techniques that are particularly useful when there is an underlying disorder (e.g. trauma or surgery) that produces bone remodeling.
False negative
Uncommonly, marrow pressure may be sufficiently increased to produce hypoperfusion, resulting in a false-negative bone scan.
Gadolinium enhancement is present, except in rare cases where the bone is poorly perfused due to vascular compromise from high marrow pressure or underlying vascular disease leading to bone infarction.
Subperiosteal abscess might be present, MRI tends to overestimate the extent of infection due to difficulty distinguishing adjacent reactive edema from frank marrow infection (Figure 11).

Figure 11 MRI of the legs T2WI showing large subperiosteal abscess extending along the tibia. The marrow signal abnormality in the proximal tibial epiphysis, metaphysis and diaphysis is consistent with osteomyelitis. There is soft tissue cellulitis and myositis.
Chronic osteomyelitis17
The classic radiographic appearance is thickened cortex and variable mixtures of lucency and density.
Chronic osteomyelitis may remain clinically silent for years, then reactivate. Such reactivation generally implies the presence of a necrotic, infected bone as the nidus of reactivation.
Sequestrum is necrotic bone, isolated from living bone by granulation tissue. It appears relatively dense because it has no blood supply.
Involucrum is a shell of bone that surrounds a sequestrum.
Cloaca is a cortical and periosteal defect through which pus drains from an infected medullary cavity.
Sinus Chronic osteomyelitis of the tibia or femur is often associated with a chronically draining sinus tract.
If the drainage occurs over many years (usually decades), the tract may develop a squamous cell carcinoma (Figure 12) (Figure 13).

Figure 12 Lateral radiograph of a proximal ulna shows osteomyelitis that has developed following an open fracture. There is permeative bone destruction, as well as an H-shaped dense fragment of necrotic bone (arrow), termed a sequestrum.

Figure 13 Lateral radiograph in a diabetic patient with neuropathic foot shows a round sequestrum (arrow) in the posterior calcaneus.
Brodie’s abscess17
Subacute or chronic osteomyelitis in a child.
Usually found in the metaphysis and may present in epiphysis.
Geographic lytic lesion with a well defined,often broad sclerotic margin.
Oval, with the long axis parallel to the long axis of the bone.
Borders the growth plate (Figure 14).
Conclusion appropriate imaging work-up of the various musculoskeletal soft tissue infections aids early diagnosis and treatment.

©2019 Abdelwhab, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.