MOJ
eISSN: 2374-6939


Research Article Volume 4 Issue 4
1Chief Consultant, Bari-Ilizarov Orthopedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Russia
2Bari-Ilizarov Orthopedic Centre, Bangladesh
Correspondence: Bari MM, Bari-Ilizarov Orthopedic Centre, 72, Satmasjid Road, Nizams Shankar Plaza, Dhanmondi, Dhaka, Bangladesh, Tel 8800000000000
Received: February 22, 2016 | Published: March 3, 2016
Citation: Bari MM, Islam S, Muthiah K, Uddin J (2016) Ilizarov for Legg-Calvé-Perthes Disease. MOJ Orthop Rheumatol 4(4): 00145. DOI: 10.15406/mojor.2016.04.00145
This study presents the results of prospective consecutive cohort of patient with Legg-Calvé- Perthes disease treated by Ilizarov technique between 1995 and 2014. The primary aim is to determine the maintenance of head coverage and joint congruity and functional outcomes of this Ilizarov technique. Methods: 26 patients with a mean follow up of 12 years (range 4 to 12) were included. Results: Cumulative maintenance of head coverage and joint congruity rate for all was (95%) at 12 years. Conclusion: Articulated hinge distraction in LCPD gives satisfactory and reproducible long term clinical results.
Keywords: Legg-Calvé-Perthes, Ilizarov, Radiographic results, Arthrosis, Hip rotation,
The aim of treatment of LCPD disease is to prevent cox arthrosis.1 Several treatment options have been described in order to prevent or limit femoral head deformation by containing the head within the acetabulum. Varisation osteotomy of the femur, salter osteotomy sometimes resulted in a prolonged limb or inadequate containment.2 Ilizarov distraction technique is3,4 now well documented. The primary aim and objective of this study were to determine the long term radiographic results and functional outcomes.
9-years-old child demonstrating limitation of internal rotation of right hip. Hip rotation best assessed in prone position because any restriction can be detected and measured easily (Figure 1).
Trendelenburg test. Boy at left, standing on left leg, demonstrates negative test of right hip. At right, same boy demonstrates positive Trendelenburg test of involved right hip. Left side of pelvis drops; pelvis cannot be maintained level by left gluteus medius because of pain originating in hip joint. Trunk shifts right as patient attempts to decrease biomechanical stresses across involved hip and thereby maintain balance (Figure 2).
Same child demonstrating Thomas test for hip flexion contracture. Opposite hip flexed only until lumbar spine is flat against examining table. Lack of full extension in involved hip recorded. Child demonstrates 15° hip flexion contracture typically found in Legg-Calvé-Perthes disease.
“Roll” test for muscle spasm. Patient relaxed, lying supine on table. Examiner places hands on right limb, gently rolls hip into internal and external rotation, noting resistance (Figure 3).
Test for limitation of abduction. With child supine on table and relaxed, lower limbs gently and passively abducted to determine degree of motion of each limb (Figure 4).
Determination of proximal thigh atrophy. Circumference of each upper thigh measured and difference noted. Measurements should be made at most proximal level of thigh (Figure 5).
We treated 26 patients between 1995 and 2014. The indications for Ilizarov distraction technique includes: 1) 6 to 12 years of age at clinical onset 4. 2) Catterall III and IV and Herring5 lateral pillar group B and C, 3) Subluxation on the anteroposterior radiographs.
The surgery is performed under general anaesthesia. The child is installed in the three quarter supine position, and the position is maintained by a sheet rolled against the childs back. The intervention begins with introducing the schanz (5.5 mm) through the supraacetabular region and 2 k/wires above and below the schanz. This is fixed with arch. After that 5 to 6; 1.5 k/wires were introduced through the neck of the femur upto growth plate to increase vascularity and decrease the joint pressure.
Another one ring was applied in the upper 1/3rd of the femur with two cross k/wires. The frame is assembled with the above arch, with 15-20° abduction. Distraction is given on the table upto ½ cm. We continued distraction every 7 days alternatively for 3 weeks. Ilizarov apparatus was removed after 40 to 45 days.
Outcome measures
Children’s were evaluated every time. Complication and radiographic findings were recorded. Clinical results were assessed by Oxford hip score (OHS). Plain AP pelvic radiographs were analyzed. The neck shaft angle and the lateral extension index of Green6 were also assessed. Femoral head deformity and hip congruity were assessed by Stolberg classification7 (Figure 6).
After a mean follow up of 12 years (range 4-12) 26 patients were included. There were 18 males and 8 females. The mean age at time of diagnosis was 6 years. Mean age at surgery was 7 years (range 4-12). The disease was bilateral in one case. Four patients were rated Catterall 2.0 (58%), were catterall 3 and 12 (32%) were catterall 4. Two patients were rated Herring A; 18 Herring B and 8 Herring C (Figure 7).
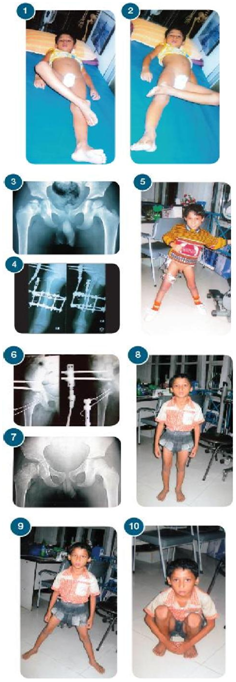
Figure 7 Diagnosis of 6years old boy.
Few studies to date have reported on the outcomes of Ilizarov distraction procedure in LCPD with long term follow up. Our study demonstrates very good long term survival after Ilizarov distraction with a rate of good radiological outcomes (Stulberg 1 to 3 and/or kellgreen Lawrence <2) of 95% at 12 years. Hinge abduction was performed at fragmentation stage.
Joseph et al.8 concluded that containment surgery aiming at preventing femoral head deformation in LCPD should be performed before the advanced stage of fragmentation. Green et al.6 noted 20% and less protrusion as a good prognostic indicator in LCPD cases (Table 1).
|
Characteristic |
Minimum |
Maximum |
Mean |
Standard Deviation |
|
Age at Diagnosis |
3.5 |
12 |
6 |
2.2 |
|
Catterall |
2 |
5 |
3 |
0.8 |
|
Deformity Index |
0.04 |
0.67 |
0.22 |
0.1 |
|
Duration of Symptoms (Months) |
2 |
10 |
3 |
3 |
|
Delay of Diagnosis (Months) |
3 |
36 |
6 |
3.38 |
Table 1 Potential risk factors
Our study is consistent with the good results of series with long term follow up by Ilizarov technique. Recently, Larson et al.9 reported on the 20 years follow up results of a prospective multicenter study of non-operative treatment and found a high prevalence of osteo-arthrosis and low clinical outcome scores.
Ilizarov articulated hinge distraction provides effective containment, which allows prolonged remodeling while avoiding the limitations of femoral varus osteotomy (short limb) and salter osteotomy (incomplete containment).10
None.
None.

©2016 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.