MOJ
eISSN: 2374-6939


Literature Review Volume 15 Issue 1
1Professor at the department of Stomatology, Faculty of Dentistry, UNAH, Honduras
2Chief of the Dentistry Service, Hospital Escuela. Professor at the Catholic University of Honduras, Honduras
3Oral and Maxillofacial Surgeon, Teaching Hospital, Honduras
4Periodontist. Professor of the Faculty of Dentistry, UNAH, Honduras
5Dentist, Private practice, Hondura
Correspondence: Romero H, Professor at the department of Stomatology, Faculty of Dentistry, UNAH, Honduras
Received: January 15, 2023 | Published: February 1, 2023
Citation: Romero H, Guifarro JJ, Díaz F, et al. Giant ossifying fibroma of the mandible treated with en bloc resection and reconstruction plate placement in pediatric patient: case report and literature review. MOJ Orthop Rheumatol. 2023;15(1):10-13. DOI: 10.15406/mojor.2023.15.00610
Ossifying Fibroma is a benign fibro-osseous tumor, but osteolytic and invasive, as well as being a rare lesion. It manifests itself more frequently in the mandible than in the upper jaw, being located preferably in the molar (52%) or premolar (25%) region. It is most commonly diagnosed in women (5:1) between the 3rd and 4th decades of life. It is related to other pathologies such as bone dysplasia, florid cement-osseous dysplasia, among others. This lesion was called a tumor by the World Health Organization (WHO) in 1992 in its classification of Odontogenic tumors, because its possible etiopathogenesis is due to periodontal ligament cells. In 2003, the WHO called it a single entity, classified like a bone tumor. The following case that is presented is about a pediatric patient with a diagnosis of Ossifying Fibroma in the mandibular area of large size, which was treated surgically with an en bloc resection of the affected area due to the great extension of the lesion and the compromised tissue. and literature review.
Keywords: fibroma ossificans, osteolysis, en bloc resection, tumor
Ossifying fibroma (FO) is classified as a benign neoplasm of the fibro-osseous type, which originates from the cells of the periodontal ligament.1 This lesion belongs to the group of fibro-osseous lesions affecting both maxillae and cranial bones.2 It is an uncommon lesion that affects more females and occurs between the third and fourth decade of life.1 It was first described in 1872 by Menzel, and the term "ossifying fibroma" was first used in 1927 by Montgomery.3 For many years it was believed that FO and fibrous dysplasia were the same pathology, but it was not until 1950, when Sherman and Sternberg, divided both entities by various histopathological, clinical and radiographic studies that they performed, concluding that they were two distinct pathologies.3
Several studies have demonstrated mutations of the HRPT2 gene in fibroma ossificans, suggesting a genetic factor in its occurrence.4 This gene, located on chromosome 1q, manufactures the parafibromin protein.5 It is also implicated in hyperparathyroidism-jaw tumor syndrome.4 It is an autosomal dominant syndrome that is associated to varying degrees with parathyroid tumors, ossifying fibromas of the jaws, renal and pancreatic tumors.4 Therefore, the discovery of an ossifying fibroma should lead to the search for genetic abnormalities and/or other anomalies mentioned above.4
Clinically, FO is characterized as an asymptomatic lesion, of highly variable size and generating bone expansion in the cortices, as osteolysis of the affected area.6 The mucosa overlying the lesion is normal. The radiographic characteristics vary according to its evolution, where it can be characterized as a radiolucent lesion at the beginning, progressively presenting areas of radiopacities in its interior, to end as a completely radiopaque lesion surrounded by a radiolucent halo.6 From the radiological point of view, they usually appear as unilocular lesions with well-defined borders, showing different degrees of opacification, related to the amount of mineralization. Initially, the lesion is osteolytic followed by gradual transformation to a mixed lesion.6
The histology of the lesion is characterized by a well vascularized fibrous stroma and variable cellularity; it also presents laminar and cancellous bone trabeculae, and rounded cement-like structures.6 Histologically all these fibro-osseous lesions have replacement of normal bone by tissue composed of collagen fibers and fibroblasts, with variable mineralization that can be osseous or cement-like.6 This type of tumor is derived from mesenchymal blast cells of the periodontal ligament and has a potential to form fibrous tissue, cementum and bone or a combination of such elements.7 Eversole et al, describe that these cementum-like structures are associated with membranous bone.8
FO belongs to the category of fibro-osseous neoplasms, in this category are also found the "active", "juvenile" or "aggressive" forms of FO.6 In several references it is mentioned that the origin is the periodontal ligament, the latter is a layer of fibro-connective tissue that surrounds the roots of the teeth and contains multipotential cells.6
The most common area that can occur in the mandibular area, according to the literature, is in the premolar and molar areas.10 The gold standard treatment consists of complete resection surgery. Unlike fibrous dysplasia, there is no data available on the use of bisphosphonates. Early diagnosis of these lesions gives the possibility of opting for more conservative treatments, such as enucleation of the lesion and subsequent curettage.6,10 Rosenberg et al.11 described that in those cases in which there is no deformity, an expectant behavior can be adopted and serial controls can be performed. Otherwise, they describe remodeling of the bone tissue. However, the literature widely agrees that complete enucleation of the lesion is the treatment of choice.11 In the case of extensive lesions with extensive involvement of bone tissue, resection of the involved segment is performed and, subsequently, the treatment can be complemented with the placement of a mandibular reconstruction plate, free grafts or microvascularized grafts depending on the size of the defect.12,13
A 16 year old male patient was presented by the pediatrics department to the maxillofacial surgery service of the Hospital Escuela, with no relevant systemic compromises, with a history of an increase in volume in the right mandibular area of 8 cm in relation to the opposite side, facial asymmetry (Figure 1); with one year of evolution according to the patient's mother. Clinically there was an expansion of the vestibular and lingual cortex in the area of the mandibular body, an indurated and well delimited lesion. The patient did not report any symptoms.

Figure 1 Preoperative clinical photographs showing the increase in volume in the right mandibular area.
It was decided to perform an incisional biopsy of the lesion, to send the sample for histopathological study and a computerized axial tomography (CT) with 3D reconstruction, to define the treatment. It was reported as a cemento-ossifying fibroma by the laboratory of the Pathology Department of the Teaching Hospital, described as a fibrous lesion, with lamellar and cancellous bone and cement. The CT scan showed a well-defined, hyperdense lesion with isodense material in its interior and expansion of the vestibular and lingual cortex, involving the mandibular body and part of the ascending branch of the right side of the mandible with a dimension of 12 cm wide and 10 cm long (Figure 2).
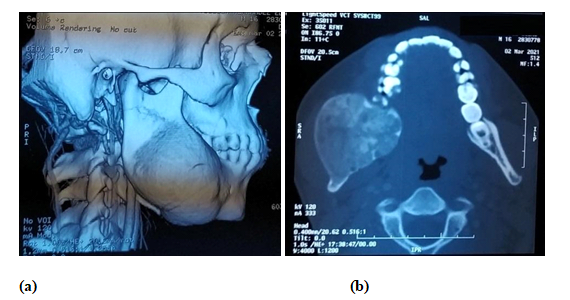
Figure 2a) Axial computed tomography showing a 3D reconstruction of the patient, with an increase in volume and expansion of the mandibular cortical body and right mandibular ascending mandibular branch. b) Axial section showing a circumscribed lesion, with isodense content and expansion of the vestibular and lingual mandibular cortical.
After the histopathological diagnosis and considering the large size of the lesion, it was decided to perform an en bloc resection of the lesion and the placement of a 2.4 titanium mandibular reconstruction plate (Figure 3) and to perform again the histopathological study of the entire lesion, confirming the initial diagnosis. Resection of the lesion was performed under general anesthesia and with a reciprocating saw for osteotomies 5 days after diagnosis.

Figure 3a) Transoperative photograph showing a macroscopic view of the tumor, with an expansion of the vestibular cortex of the affected area. 3b) Placement of the mandibular reconstruction plate, after resection of the lesion.
Analgesic and anti-inflammatory management was performed by the anesthesiology department, with the use of an elastomeric pump. The antibiotherapy management was left to the discretion of the pediatrics department, using clindamycin 600 mg iv every 8 hours and ceftriaxone 1g every 12 hours, both for 7 days.
The patient was given control appointments every two weeks for one year, with clinical and radiographic control (Figure 4). Currently the patient is stable and in good evolution, with rehabilitation plan and control appointments. No genetic study was performed.
The ossifying fibroma or ossifying cementum is a rare fibro-osseous tumor that has osteolytic activity and can grow if not diagnosed in time. The origin of the lesion, according to the WHO, comes from cells of the periodontal ligament,1,2 but there are several studies that suggest that it may be caused by genetic factors.4,5 It appears most frequently in the maxillary bones, with the mandible being the most prevalent location (75-89% of cases),14,15 with the most frequent site in the mandible being the posterior region;10 although cases have also been reported where it appears in other bones of the skull. 3,16
Management of FO tends to be difficult due to its aggressive nature, as well as the high recurrence rate.11 Surgical resection rather than enucleation and curettage (which have a considerably high recurrence rate) is therefore the preferred treatment of choice.11,12,13 However, surgical treatment results in major hard and soft tissue defects that affect not only esthetics and function, but also craniofacial development as well.11 These defects can be reconstructed by treatments such as free bone grafts (small defects) or microvascularized grafts (large defects).12,13
The reconstruction of these post-tumor ablative defects is a great challenge, especially in developing patients such as pediatric patients.11 The surgeon in charge can rely on several auxiliary diagnostic methods such as the use of CT to define the spaces involved and stereolithographic models to reduce surgical time and patient morbidity. 17
Ossifying fibroma is an invasive and osteolytic lesion, which is caused by cells of the periodontal ligament and there may be genetic implications. Patients who present this type of lesion should undergo prophylactic studies to rule out any alteration, as discussed in this article. This neoplasm can be managed in different ways depending on the size of the lesion. It is clear that conservative management, such as enucleation and subsequent curettage, is the most indicated treatment in young or pediatric patients, but the size of the tumor must be taken into account. It can often go unnoticed by the patient and family members until it reaches a considerable size, and conservative management does not become a useful option for the surgeon. In cases where the FO reaches a large extension, and has invaded considerably the bone tissue in great quantity, surgical resection is the treatment of choice.
Author Contributions: For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used "Conceptualization, Hugo Romero and Mario Gabrie; methodology, Juan José Guifarro; validation, Hugo Romero, Juan José Guifarro and Francisco Díaz; formal analysis, Francisco Díaz and Vilma Umanzor; investigation, Mario Gabrie, Francisco Díaz, Vilma Umanzor.data curation, Vilma Umanzor; writing-original draft preparation, Hugo Romero and Mario Gabrie; writing-review and editing, Mario Gabrie and Vilma Umanzor; visualization, Francisco Díaz and Juan José Guifarro; supervision, Hugo Romero.Juan José Guifarro; project administration, Vilma Umanzor. All authors have read and agreed to the published version of the manuscript". Please turn to the CRediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the reported work....
To Karen Elizabeth Sabillón Ellner, for support in providing data and review of the article along with the main authors.
The author declare that there are no conflicts of interest.

©2023 Romero, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.