MOJ
eISSN: 2374-6939


Research Article Volume 5 Issue 4
Dolomiti Sportclinic, Italy
Correspondence: Andrea Cosentino, Dolomiti Sport clinic, via Purger 181, 39046 Ortisei/St. Ulrich (BZ), Italy, Tel 39 3334503625
Received: August 05, 2016 | Published: September 2, 2016
Citation: Gurndin A, Cosentino A, Bizzotto N (2016) Femoral-Side ACL Rupture: Arthroscopic Transosseous Refixation Technique and Early Outcomes.MOJ Orthop Rheumatol 5(4): 00190. DOI: 10.15406/mojor.2016.05.00190
Background: Many different surgical techniques are nowadays performed in Anterior Cruciate Ligament (ACL) lesions. Several studies demonstrated that native ACL contains mechanoreceptors that are fundamentals for the proprioception of the knee, which are removed during the standard arthroscopic ACL reconstruction.
Material and Methods: This article shows a new arthroscopic way to reinsert an ACL, through a Vycril® #2 wire using a modified Mason-Allen technique, combined with the “healing response technique”, described by Steadman. We recommend this technique for patients with an ACL lesion, detached from his femoral insertion, as suggested by MRI and confirmed by arthroscopic view. Postoperatively the patient must have a knee brace locked at 15-degrees of flexion for the first two weeks with partial weight bearing and prophylaxis of thrombosis with low-molecular-weight heparin until the complete weight bearing; then gradually the flexion will be increased during the next month.
Discussion: This new technique permits to maintain the native ACL, reinserted into his anatomical insertion and the mechanoreceptors that are fundamentals for the proprioception, associated with the healing power of the bone marrow cells and blood.
Keywords: ACL suture, ACL proprioception, Steadman technique
ACL, Anterior Cruciate Ligament; MRI, Magnetic Resonance Imaging
The Anterior Cruciate Ligament (ACL) tears are common injuries, especially during the winter sports.
The current gold standard for ACL tears is anatomic ACL reconstruction with autograft or allograft,1 recommended first of all for athletes and active patients, but also for patients with giving-away symptoms.
The femoral and tibial attachment sites of the anterior cruciate ligament contain mechanoreceptors such as the Pacinian corpuscles, Ruffini endings, and Golgi tendon organ-like corpuscles, all of which play a role in proprioception. With an ACL tear, those mechanoreceptors undergo to a rupture that may lead to a lack of afferent sensory input to the central nervous system.2,3
In addition, elapsed time from the injury may affect proprioception and postural stability.
In some cases, the ACL tear consists in an isolated femoral-side rupture, clinically diagnosed with positivity of Drawer, Lachman and (depending on the pain) Pivot shift test, shown during MRI exam and confirmed during the arthroscopic procedure.
Our study consists, in those cases, in a new ACL refixation technique, with the aim of preserving the native ACL and his mechanoreceptors that lead to a better proprioception and stability. Moreover, drilling the femoral bone leads to a lack of bone marrow stem cells that promote the healing of the ligament, as described by Steadman et al.4 in the “healing response technique”, an all-arthroscopic procedure that preserves the native ACL and makes use of an arthroscopic awl with a 45-degrees angle to make holes in the femoral attachment of the ACL.4
The inclusion and exclusion criteria for this technique are shown in Table 1.
|
Inclusion criteria |
|
Acute ACL lesion - Femoral Detachment |
|
Intra-Synovial ACL Lesion |
|
Synovial Sleeve Still Intact |
|
Exclusion criteria |
|
ACL Intraligament Lesion |
|
Associated Collateral Lesions |
|
Bony ACL Avulsion |
|
Unstable Meniscal Lesions |
Table 1 Inclusion and Exclusion criteria
We suggest this technique for patients with an intra-synovial ACL lesion, detached from the femoral insertion, proved positive by Lachman and Drawer tests and as the MRI exam can primarily show (Figure 1).
Before the arthroscopic procedure, the patient is in supine position and after endovenous infusion of antibiotic solution; the knee is positioned on a leg holder, flexed at 90-degrees, with a hemostatic device at proximal femur.
The first step consists in a diagnostic arthroscopy through the standard arthroscopic portals; after lavage of hemarthros, all the slight meniscal lesions are regularized, if present. If in the pivot compartment the ACL shows a detachment from femoral insertion with synovial sleeve still intact around the bundles and unstable during the hook-traction-test (Figure 2), we proceed with the second step that consists in the ACL suture.
After partial removal of the Hoffa’s fat-pad, a cannula is inserted in the standard antero-medial portal, with the arthroscopic optical device in the standard antero-lateral portal.
Through a modified Mason-Allen stitch technique, a Vycril® #2 wire is passed through the distal ACL fibers with an arthroscopic special tool (Figure 3) and both Vycril® wires ends are drilled outside with two slotted guide wires to the distal lateral femur in a parallel way (Figure 4).
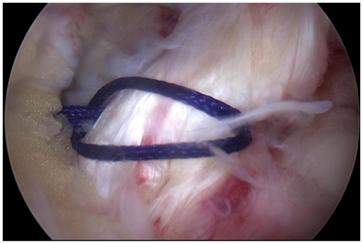
Figure 3 Vycril® #2 wire passed through the distal ACL fibers with a modified Mason-Allen stich technique.
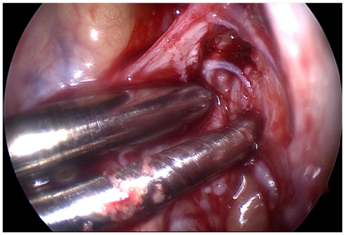
Figure 4 Two guide wires are drilled to the distal lateral femur in a parallel way through the anatomical insertion of ACL
After a small incision of the skin and the split of the fascia lata, the two wires are knotted over the transosseous bridge with an appropriate push-knot device, directly over the lateral distal femoral cortex.
By this technique an anatomical reinsertion of the ACL is achieved, as well as a normal tensioning of the previous ligament fibers (Figure 5).
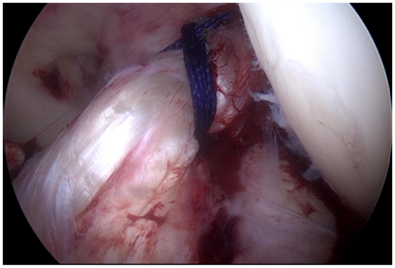
Figure 5 Normal tensioning of ACL after knotting the two wires over the lateral distal femoral cortex.
Finally, after a plentiful arthroscopic lavage of the joint, soft tissues are closed layer by layer and covered with sterile dressing; the knee is locked at 15° of flexion with an adjustable R.O.M. knee brace for the next two weeks with partial weight bearing, with an accurate antithrombotic prophylaxis with low-molecular-weight heparin.
At the end of the surgical procedure we performed again Lachman, Drawer and Pivot shift tests that result completely negative, as also shown by the arthroscopic view of the reinserted ACL, extremely stable at the hook-traction-test.
We performed another MRI the day after the surgical procedure that shows how the native ACL has a good tension (Figure 6), with the holes centered in the femoral isometric insertion point (Figure 7); it’s also possible to see the micro fractures for the Steadman’s healing response technique (Figure 8).
The stitches are removed after 14 days, than the flexion of the knee brace must be increased by 60-degrees for other two weeks during which the patient can start with isometric exercises of the quadriceps, walking into the water and gradually achieve complete weight bearing, without crutches.
After one month from the operation, the knee flexion with the brace must be increased by 90-degrees for other two weeks and the patient can start swimming (it’s forbidden the breaststroke). At the end of those two weeks the patient can start home cycling, if the knee flexion reaches easily 90-degrees; jogging is permitted not before the end of the 12th week and contact sports, ball-sports and pivot-torsional movements are forbidden until the end of the 6th month.
Patients who accepted this new technique were just 10 in the past winter-sport season; for that reason we cannot have long-term results and there are no references of this surgical procedure in literature.
However after 6 months, those patients were interviewed and they referred that they didn’t feel any instability problems of the knee and would be able to start again their sports activities.
This new technique is a valid option for patients with an isolated, acute, femoral-side ACL lesion, without any collateral ligaments lesions or unstable meniscal tears, and in which cases we prefer the standard reconstruction with ST.
Performing this technique permits to preserve the native ACL, avoiding all the risk of an ACL reconstruction, such as graft failure or the lack of proprioception, well documented in patients who have undergone ACL reconstruction, highlighting the advantages of ACL further preservation.
The ACL refixation leads to keep the original proprioception, due to the maintenance of the patient’s ACL that contains all the mechanoreceptors involved in knee proprioception.
As described by Steadman et al. in the healing response technique,4 93% of patients had a minimum of 2-year follow-up at an average of 7.6 years. Average preoperative Lysholm score was 54 and improved to an average of 90 postoperatively (p = 0.001); Tegner activity scale mean at follow-up was 5 (range, 2 to 9); patient satisfaction mean was 10 (range, 4 to 10); higher patient satisfaction was correlated with increased Lysholm score at follow-up. Tegner activity scale was associated with postoperative Lysholm score. This study demonstrates the effectiveness of the healing response procedure to allow patients to return to high levels of recreational activity and to restore knee function to normal levels.
In a select group of mature patients with acute proximal ACL tears, the healing response procedure is an effective treatment technique.
Therefore we believe that reattaching the proximal ACL stump to the footprints of the femoral insertion after drilling holes in this region to deliver stem cells and growth factors to the scaffold might be a way to create the best possible conditions to stimulate the healing process.5,6
None.
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.

©2016 Gurndin, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.