MOJ
eISSN: 2374-6939


Research Article Volume 13 Issue 4
Department of Orthopaedic surgery, Ain Sham university Cairo, Egypt
Correspondence: Ebied Wessam, Department of Orthopaedic surgery, Ain Sham university Cairo, Egypt
Received: May 26, 2021 | Published: August 11, 2021
Citation: Maziad AM, Mahmoud AN, Wessam E. Failure due to metallosis after cruciate retaining total knee replacement. MOJ Orthop Rheumatol. 2021;13(4):75-78. DOI: 10.15406/mojor.2021.13.00552
Background: Rupture of PCL on cruciate retaining TKA can cause abnormal accelerated wear of polyethylene component which may result in metal/metal articulation and development of massive infiltration of metal debris in the periprosthetic soft tissue (metallosis).
Patient and methods: Eight cases (Five females, 3 males, mean age 64.6 years) with failed primary cruciate retaining knee arthroplasty were retrospectively studied. Revisions were performed after a mean of 59.8 months due to pain and instability. All the patients had variable degrees of clinically relevant posterior knee instability. Infection was excluded in all cases through microbiological examination and synovial fluid analysis.
Results: Abnormal direct metal-on-metal articulation between the femoral component and the tibial base plate with advanced polyethylene wear were found intraoperatively in all cases in addition to extensive tissues black staining, advanced osteolysis and pseudotumor formation. All cases were managed by single stage revision surgery with implant removal, profound synovectomy and revision using a more constrained modular revision knee system.
Conclusion: Metallosis after total knee arthroplasty is a rare situation that should be suspected in total knee arthroplasty cases with radiologically evident advanced polyethylene wear especially in cruciate retaining knee systems. It could lead to significant osteolysis making revision surgery technically challenging.
Keywords: metallosis, bubble sign, metal-line sign, cloud sign, cruciate retaining, revision total knee replacement
Metallosis is a condition characterized by an infiltration of periprosthetic soft tissues and bone by metallic debris. It is resulted from metal surfaces friction that may elicit an inflammatory response in the synovium and adjacent bone and can lead to significant osteolysis, tissue necrosis and formation of soft tissue pseudotumor,1 and can lead to pain, and swelling, osteolysis and implant loosening and joint instability.2,3 Metallosis after knee arthroplasty is a rare condition and its occurrence almost always indicates unintended direct metal-on-metal articulation at the tibiofemoral or the patellofemoral joint (in metal-backed patellar components) which typically occurs with advanced polyethylene wear.4
Metallosis triggers a cytokines chronic inflammatory process that is thought to be attributed to metal hypersensitivity, particle induced synovitis and the direct toxic effects of the metal particles. This can lead to osteoclastic bone resorption, progressive periprosthetic osteolysis and eventually implant loosening. On the contrary to hip arthroplasty, there are few reports on metallosis after total knee arthroplasty.3,5–8 This study describes 8 cases of knee instability following extensive metallosis in a previously well fixed cruciate retaining knee arthroplasty.
This is a retrospective series of 8 patients who had metallosis with their cruciate retaining TKA and all underwent revision total knee replacement. They were 3 males and 5 females with a mean of 64.6 years (range 55-73) (Table 1). All patients had their primary cruciate retaining fixed bearing total knee systems (Three Zimmer Nexgen CR, three Stryker Scorpio TKA and 2 ImplantCast GmbH TKA. All did well for at least 4 years before complaining of swelling, pain, instability, and skin redness. The mean time to revision surgery was 59.8 months (Range 49-72 months). Preoperatively, patients were evaluated clinically and radiologically. The radiographic signs of metallosis includes the metal-line sign, the bubble sign, and the cloud sign were noticed in preoperative radiographs. Other associated radiographic findings include advanced polyethylene wear with direct metal-on-metal contact at the tibiofemoral interface, osteolysis, implant loosening, joint effusion, and metallic fragmentation (Figures 1, 2). Septic loosening was primarily excluded preoperatively through laboratory investigations and synovial fluid analysis for all cases. A normal ESR and CRP with synovial fluid analysis free from infection has been ensured for all cases preoperatively.
|
Case |
Gender |
Age (Y) |
Side |
Time since primary knee replacement (M) |
Presentation |
Follow up after revision (M) |
|
1 |
Male |
66 |
Right |
54 |
Pain, swelling |
16 |
|
2 |
Male |
69 |
Right |
72 |
Pain, skin redness |
14 |
|
3 |
Male |
73 |
Right |
47 |
Pain, instability |
23 |
|
4 |
Female |
55 |
Right |
46 |
Pain, Swelling |
19 |
|
5 |
Female |
59 |
Left |
53 |
Pain |
15 |
|
6 |
Female |
61 |
Right |
63 |
Pain, instability |
9 |
|
7 |
Female |
62 |
Right |
66 |
Pain |
11 |
|
8 |
Female |
72 |
Left |
72 |
Pain, swelling, instability |
11 |
Table 1 Patients demographics, clinical presentations and follow up
During the revision surgery all cases showed direct tibiofemoral articulation with advanced polyethylene wear in addition to severe metallosis with black staining of the synovial tissues, cystic cavities, and metal-debris tumor-like formation (Figures 3, 4). A profound synovectomy was carried out in all cases and tissue samples were sent for histopathology which showed chronic inflammatory reaction and metal debris. Extended culture and sensitivity showed no bacterial growth. The implants were found to be loose in all cases. The retrieved implants showed visible scratches and advanced plastic wear. After removal of the prothesis, advanced osteolysis with holes filled with black debris was seen. Local debridement was carried out and cysts were curetted.
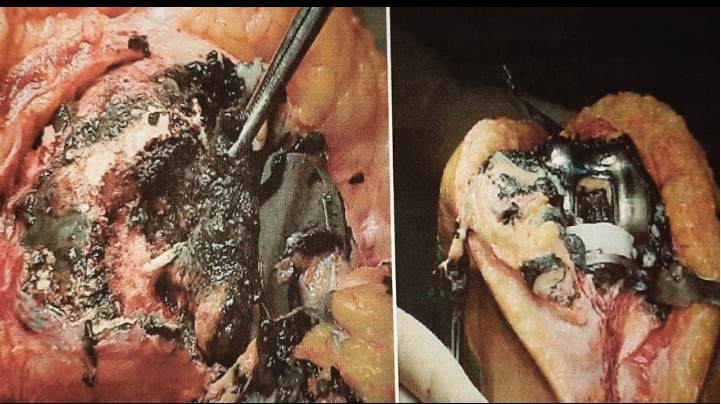
Figure 3 Intraoperative photos showing extensive black staining of the synovial tissues and advanced osteolysis with holes filled with metal debris beneath the prosthetic components.
All cases were revised using a cemented Legacy constrained condylar knee (LCCK, Zimmer, Warsaw, IN) (Figure 5). Metal augments has been used in 6 cases to reconstruct bony defects. After a mean of 14.7 months follow up, all the cases had stable revisions and none of the cases needed re revision. The Oxford knee score has improved from a mean of 22 to 38 (out of 48) on the last follow up.
We report a mechanism of failure of a cruciate retaining TKR where rupture of PCL lead to accelerated polyethylene wear and abnormal direct metal articulation leading to metallosis. Eight cases of PCL retaining knees were revised to constrained knee systems due to metallosis, Metallosis is the accumulation of metal debris within tissues. It was first reported by von Ludinghausen et al.9 with fracture fixation with metal hardware. Basically every metal implant (e.g. screws, plates, arthroplasty) has a potential local or systemic effect due to metal ions.
Metallosis is a well-known complication of metal-on-metal (MoM) bearing total hip arthroplasty and it is also reported after shoulder, elbow and wrist arthroplasty.10–13 After total knee arthroplasty, it is considered a rare complication because there is no normally metal on metal articulation and it can occur when this unintended take place after advanced polyethylene wear leading to direct metal articulation at the tibiofemoral or the patello-femoral interface (with metal backed patellar components). The released metal debris can induce a chronic inflammatory response leading pseudotumor formation, osteolysis and loosing.3 The pathogenesis involves direct cytotoxic effects, a delayed hypersensitivity (type IV) response to metal debris and particle-induced synovitis.13,14
Metallosis can cause significant bone loss therefore early diagnosis and revision surgery are crucial. There are few reports on metallosis after total knee arthroplasty. Elmogazy et al.3 reported 4 cases of revision TKA because of metallosis with advanced osteolysis and pseudotumor formation. They noted direct metal-on-metal tibial and femoral articulation in all cases during surgery. All patients had a one-stage revision surgery with implant removal, profound synovectomy and implantation of a constrained modular revision knee system. Weissman et al.7 reviewed the radiographs of 18 patients with Metallosis after TKA and reported that the metal-line sign (dense line outlining the capsule or articular surface of the knee joint) would be helpful to make the diagnosis preoperatively in many patients. Such sign was noticed in all of patients’ radiographs in this study. Schiavone Panni et al.1 reported four patients who underwent revision surgery because of metallosis after full thickness PE wear causing friction between the femoral and tibial component in three cases and between metal-back patellar component and the femoral component in one case after a mean time of 12.5 years after knee arthroplasty.
Sharareh et al.2 presented a case of metallosis after 26 years of TKA in a an 81 years old lady and was managed by revision TKA. They found abnormal direct MoM friction between the femoral component and both the tibial base plate and the metal backed patellar component.
Metallosis can appear radiographically as a thin rim of linear increased density outlining the capsule and the suprapatellar pouch, this is called the metal line sign. Other radiographic findings include circular radiodensities called (bubble sign), amorphous, cloudy, periprosthetic soft tissue densities called (cloud sign), osteolysis, loosing and metallic fragmentation.5
This short report aimed to retrospectively review eight cases of metallosis found during revision knee replacements for cruciate retaining knee systems. Several shortcomings have been found in this study, being retrospective, with small number of cases and short follow up after revision. Longer follow up would be needed to study the efficacy and longevity of revision in such cases.
We report a mechanism of early failure of a cruciate retaining TKR where rupture of PCL lead to accelerated polyethylene wear and abnormal direct metal articulation leading to metallosis. Metallosis is a rare situation that should be suspected in TKR cases with radiologically evident advanced polyethylene wear. It could lead to significant osteolysis making revision surgery technically challenging.
None.
The authors declare no conflicts of interest.

©2021 Maziad, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.