MOJ
eISSN: 2374-6939


Research Article Volume 15 Issue 6
1Head of Arthroscopy and Sports Trauma Group of the Department of Orthopedics and Traumatology Hospital Puc Campinas, Brazil
2Postgraduate Program in Health Sciences/Rheumatology and Ultrasonography Service - Pontifical Catholic University of Campinas, Brazil
3Postgraduate Program in Health Sciences/Neurology Service - Pontifical Catholic University of Campinas, Brazil
4Head of Department of Orthopedics Hospital Puc Campinas, Campinas, Brazil
5Associate Orthopedist of the Arthroscopy and Sports Trauma Group, Department of Orthopedics Hospital Puc Campinas, Brazil
6Assistant Orthopedist of the Arthroscopy and Sports Trauma Group, Department of Orthopedics Hospital Puc Campinas, Braziil
Correspondence: José Alexandre Mendonça, Postgraduate Program in Health Sciences, PUC-Campinas, Rua da Fazenda, 125,Vila Flora, Sumaré – SP - Brazil, Zip code: 13175-665, Tel +55 019 25 8135-8322, +55 019 25 8135-8322
Received: October 18, 2023 | Published: November 3, 2023
Citation: Nunes LFB, Mendonça JA, Tedrus GMS, et al. Evaluation of the anterolateral ligament of the knee with high resolution ultrasound. MOJ Orthop Rheumatol. 2023;15(6):199-202. DOI: 10.15406/mojor.2023.15.00645
Objectives: To determine whether high-resolution ultrasound is an exam that contributes to the identification and assessment of the integrity of the anterolateral ligament of the knee in patients with anterior cruciate ligament injury.
Methods: 41 patients, 16 to 55 years old, with primary lesion of the anterior cruciate ligament were evaluated. Demographic data were collected, and a Pivot Shift test was performed. An ultrasound examination was performed, with a high- resolution probe, on both patients' knees, initially, seeking the visualization of the anterolateral ligament in all its extension and later assessing its integrity, ending with an assessment of the lateral meniscus.
Results: 100% of the evaluated cases, it was possible to visualize the anterolateral ligament through ultrasound with 46.3% of injuries, with the tibial portion being the most injured. 19 patients (46.3%) had anterolateral ligament injury on the same side as the anterior cruciate ligament injury, while in 19 cases (46.3%) no anterolateral ligament injury was observed on either side. 5 patients had a pivot shift test considered positive with 80% of associated anterolateral ligament injury. 31 patients had lateral meniscus injury by magnetic resonance imaging. Of the 31 patients, 25 were confirmed by ultrasound. Of the 11 patients without lesion of the lateral meniscus by MRI, none had an ultrasound lesion. Adding these two groups, 92.6% of results favorable to ultrasound, (p <0.001).
Conclusion: The data obtained suggest that ultrasound contributes to the identification and assessment of the integrity of the knee anterolateral ligament in patients with anterior cruciate ligament injury.
Level of Evidence IV.
Keywords: anterior cruciate ligament, knee, ligaments, articular, rupture, ultrasonography,
palavras-chave: joelho, ligamento articular, ligamento cruzado anterior, ruptura, ultrassonografia
Historically, anterior cruciate ligament (ACL) reconstruction began to gain importance and notoriety in the late 1960s, being the subject of many studies to the present day.1 In the 1960s, the diagnosis was difficult mainly due to the lack of clinical tests that identified the isolated ACL injury, and the treatment was based on an attempt to reduce the anterior knee drawer to 90o of flexion by tensioning the medial capsuloligament structures.1
The 70's were very important mainly due to the discovery of the Pivot Shift test, by Galway, and the lachman test, being today considered the most specific and most sensitive test, respectively, for the diagnosis of ACL injury.2,3
From the 1980s to the 2000s, the era of the free patellar tendon was considered. The tendon came to be considered the gold standard and the technique, finally offering good functional results and easy replication among surgeons.1
In the 2000s, although the ACL reconstruction technique was already extremely successful, with good results, it was noted that in 25% of the patients there was residual instability with the positive Pivot Shif test. This residual instability could be the cause of post-operative chondral and meniscal injuries, contributing to the degenerative evolution of this joint. The anterolateral knee complex consists of all layers of the iliotibial tract, including Kaplan fibers, the joint capsule and the recently studied anterolateral ligament (ALL). These structures act synergistically with the ACL, mainly in anterolateral rotational instability.4–6
ALL helps to control the rotational stability of the knee, especially in the first degrees of flexion.7,8 With a better understanding of this structure and a more accurate dissection technique, there seems to be a trend as to the origin of this structure in a region that goes from the center to the posterior and proximal region of the lateral epicondyle.9–13
The evaluation of ALL in imaging is the subject of many studies. In magnetic resonance imaging (MRI), a gold standard exam to assess internal knee injuries, the ALL, especially its tibial part, can be better visualized through the coronal T2 cut with fat suppression. The evaluation of the ALL has already been carried out by some teams and there is a consensus on the difficulty in analyzing the entire length of the ligament using MRI. Ultrasound (US) is a non-invasive, radiation-free, mobile and easily accessible imaging technology used for the evaluation of various systems, including musculoskeletal, vascular, gynecological and abdominal.14,15 There are few articles that demonstrate the ability of the US in the evaluation of ALL, especially in patients with ACL injuries. The use of high-definition US in the evaluation of the ALL would be a pioneer and could consolidate this imaging technique, together with MRI, as the gold standard in the evaluation of this ligament.
The hypothesis to be evaluated from this study is the effectiveness of the high- definition US examination as a reliable and useful imaging method in the evaluation and diagnosis of ALL lesions based on the US ability to visualize and evaluate its integrity.
Prospective observational study that evaluated 41 adult patients of both genders, aged 16 to 55 years, attended at the Arthroscopy and Sports Trauma Clinic center. All patients had a complete ACL injury of the knee, with a diagnosis made by physical examination, tests for ligament evaluation and image examination (MRI). All selected patients had a classic history of knee sprain in sports.
Procedures
The study had an experienced orthopedic medical evaluator, a member of the Sports Trauma group, who performed the following procedures on all patients: • Clinical history and demographic data collection: Age, sex and injured side. • MRI evaluation: confirmation of ACL injury through images and report, laterality and if there was an associated injury to the ML.
41 patients with ACL injuries participated in the study, 82.9% of the patients were male and 17.1% were female. The mean age of the patients was 28.6 years (standard deviation = 9.5 years). Regarding the injured side, 21 patients suffered an injury to the left knee and 20 patients had an ACL injury to the right knee. Table 1 shows the distribution of patients and injuries due to laterality. The visualization rate for the entire length of the ALL was 100.0%, with 46.3% of associated ALL injuries diagnosed by US, with the injured part being concentrated in the tibial region.
| Lesion | D | E |
| ACL lesion | 20 | 21 |
| ALL lesion | 10 | 9 |
| % ALL visualization | 100,0 | 100,0 |
| % ALL lesion | 50,0 | 42,0 |
| % femoral lesion | 30,0 | 22,2 |
| % tibial lesion | 70,0 | 77,7 |
Table 1 Distribution of patients and injuries due to laterality and location
Source: Elaborated by the author (2020).
Note: ALL, anterolateral ligament; ACL, anterior cruciate ligament.
Table 2 shows the side on which the US found the ALL injury. It was considered as a favorable result for the ultrasound evaluation when the ALL injury was found in the same laterality as the patient's ACL injury (ipsilateral); that is, of the 41 patients evaluated, 19 (46.3%) had an ALL injury, seen through ultrasound, on the same side as the ACL injury, and 19 patients (46.3%) did not have an ALL injury (Figure 1). Adding these two groups, there are 38/41 (92.6%) of results favorable to ultrasound, being statistically greater than 50% (p-value <0.001; Z test; unilateral hypothesis).
| ALL lesion | N | % |
| Ipsilateral | 19 | 31,7 |
| Contralateral | 3 | 7,3 |
| none | 19 | 46,3 |
Table 2 Proportion of anterolateral ligament injury found in the ultrasound exam - injured group
Source: Elaborated by the author (2020).
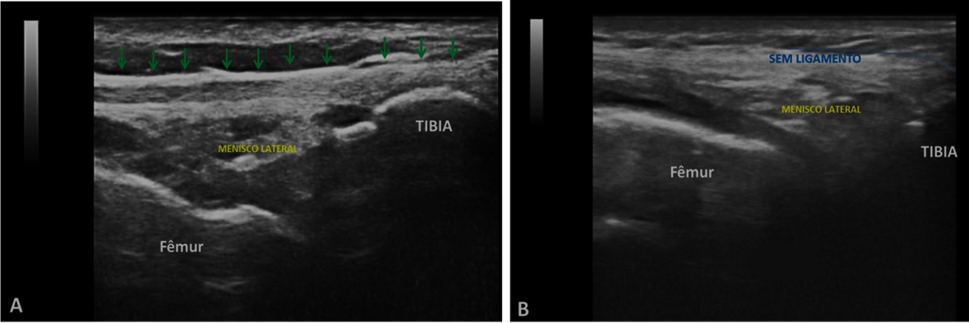
Figure 1 (A) Longitudinal ultrasound view of a normal anterolateral region, ALL in a right knee, with fibrillary hyperechogenic echotexture of the ALL (arrows); (B) View of longitudinal ultrasound of the anterolateral region in another right knee, without anterolateral ligament.
Table 3 shows the agreement between the pivot shift test and the ALL lesion findings at US. In the table it is noted that, of the 41 patients evaluated, 5 had a Grade 3 pivot shift test, considered positive, and of these 5, 4 had an ALL lesion seen through the US (80.0%). Twenty-one patients (51.2%) had negative results for ALL injury by US and pivot shift test and 4 patients (9.8%) had positive results in both evaluations; that is, an agreement of 61.0% (Kappa = 0.174) was observed between the evaluative exams. One patient (2.4%) had a negative result for ALL injury and positive for a pivot shift test and 15 patients (36.6%) had positive results for an ALL injury and negative for a pivot shift test. The p-value = 0.164 (Fisher's exact test) shows that there is no statistically significant association between the two exams.
| ALL US | Pivot | |||
| No | Yes | |||
| n | % | n | % | |
| No | 21 | 51,2 | 1 | 2,4 |
| Yes | 15 | 36,6 | 4 | 9,8 |
Table 3 Comparison of the Pivot Shift Test and lesion of the anterolateral ligament by ultrasound
Source: Elaborated by the author (2020).
Note: ALL, anterolateral ligament; US, ultrasound.
Table 4 shows the comparison between MRI and US for lateral meniscus (LM) findings. There is a high agreement between the exams (26.8% + 61.0% = 87.8%), with Kappa = 0.728. The p-value <0.001 (Fisher's exact test) indicates a statistically significant association between the two exams. Of the 41 patients evaluated, 30 had an ML lesion on MRI. Of these 30 patients, 25 presented the same lesion in the US evaluation. Of the 11 patients who did not have an ML lesion on MRI, none showed an injury after visualization by US.
| LM US | MRI LM | |||
| No | Yes | |||
| n | % | n | % | |
| No | 11 | 26,8 | 5 | 12,2 |
| Yes | 0 | 0,0 | 25 | 61,0 |
Table 4 Comparison of magnetic resonance imaging with ultrasound for finding the lateral meniscus
Source: Elaborated by the author (2020).
There is a consensus among several teams that have studied the visualization of the ALL by MRI that it is difficult to analyze the ligament along its entire length.15 Through MRI exams, Claes et al.16 identified ALL in all its extension in 76.0% of the cases; Helito et al.7 in 71.7% of cases and Taneja et al.17 found in only 11% of cases. Catherine et al.18 used MRI, cadaver dissection and immunohistochemistry to confirm the existence of ALL. In the image analysis, a high definition 3 Tesla machine was used and, although they visualized the ALL in 100.0% of the exams, they concluded that the anatomy cannot be clearly defined.
The US was used to visualize the ALL in some previous studies. Cianca et al.8 were the first to describe a view of ALL in a case report with a male patient. They reported that the ligament was easier to identify when the knee was flexed at 90° with slight internal rotation. Cavaignac et al.19 reported 100% sensitivity in visualizing the ALL in 18 cadaver knees when placing US-guided metal needles at the proximal and distal ends of the LAL and using a 12 MHz linear transducer, with evaluations performed by a single radiologist. They concluded that the US is an adequate tool for identifying the ligament. Likewise, Zappia et al.20 in an anatomical study with cadavers concluded that ultrasound is useful for assessing ALL but emphasized the importance of studies evaluating its visualization in the knees of patients with ACL injuries.
In other studies, Oshima et al.21 reported that the US could be used to confirm the integrity of the ALL, as they located the ligament using real-time virtual US on 18 knees of 9 healthy male volunteers (28-37 years old). The thickness, length and distance between the tibial insertion and the lateral tibial plateau were compared at MRI and at US (with knee flexed at 30°).
In our study evaluating 82 knees of 41 patients, the ALL was viewed in its entirety, corroborating the studies by Cavaignac et al.15 Of the 41 injured knees, 46.3% had an associated ALL injury diagnosed by US, with the majority of the injuries located in the tibial region. The prevalence of ALL injuries in patients with ACL injuries varies, in the literature, from 10 to 78%.9,12,22 In a previous study on cadavers, MRI analysis revealed a 2-4 mm thickening of the central third of the lateral capsule in 3/10 specimens (30%). On the other hand, only two studies have classified ALL lesions on MRI. Helito et al.22,23 defined four categories: proximal, distal, meniscal and Segond fractures.24 Of these, 38% had an abnormal sign of ALL. Cavaignac et al.19 comparing the ALL evaluation by US and MRI in 30 patients with acute ACL injury, showed 63% of ALL injury by US and 53% by MRI. Van Dyck et al.25 evaluated 90 patients with acute ACL injuries and found 46% of ACL injuries, while Helito, after analyzing 228 knees with acute ACL injuries, found 40% of ACL injuries, corroborating with the data from this injury study of ALL in patients with ACL injuries.23
In the analysis of the correlation of the pivot shift test with ALL injury, Cavaignac et al.19 demonstrated a 75% correlation of the positive physical examination with a lesion seen on the US. Song et al.2 after MRI review and ALL evaluation, they observed 76% of ALL injuries in the group with grade 2/3 pivot shift test against 29% of ALL injuries in group 2. In this study, there was a great correlation between the positive pivot shift test and the presence of the ALL lesion, going in the same direction as what the literature says.
In this study, in addition to the ALL assessment, the integrity of the lateral meniscus was assessed. Of the 41 patients evaluated, 30 had an LM lesion on MRI, and 25 had the same lesion on US. Of the 11 patients who did not have an LM lesion on MRI, none showed an injury after visualization by the US. Thus, it is concluded that in the LM evaluation, high agreement and statistically significant association between MRI and US were observed in the patients evaluated with ACL injury.
Shetty et al.26 in a study with 35 patients with meniscal injuries, reported that the US exams had sensitivity of 86.4%, specificity of 69.2%, PPV of 82.6% and NPV of 75%, and concluded that the US could be used to confirm the results of clinical tests before knee arthroscopy. Shanbhogue et al.27 in a study with 35 patients, compared the applicability of US and MRI (where MRI findings were used as the gold standard) as methods to identify meniscal injuries and found that sensitivity, specificity, accuracy and the NPV of US knee exams was 86.2%, 84.9%, 85.4% and 91.8%, respectively.
In another study, Sladjan et al.28 observed that the US is more sensitive and specific for chronic injuries of the LM (85 and 90%, respectively) than for acute injuries of the LM (71 and 87%). MRI also yielded higher values of sensitivity and specificity for chronic injuries of the LM (75 and 95%, respectively) than for acute injuries of the LM (68 and 87%) and concluded that the accuracy of the US examination is demonstrated by the high reliability of this method in the diagnosis of injuries of the LM of the knee. This study presents as strengths the use of a high-resolution 18Mhz US probe, superior to all the evaluated studies, and all the results were compatible with the hypothesis initially raised that the US is an imaging method that can help and add to the daily clinical practice of the orthopedic surgeon of the knee both to evaluate the ALL and to evaluate LM.
There is no gold standard method for assessing anterolateral rotational instability of the knee, and the pivot shift test is currently used for this. In this study, the test was positive in only 5 patients, showing a high correlation with ALL lesions. If the test was performed under anesthesia, the number of positive tests could have been greater, since in the US analysis, an ALL lesion was found in 19 patients.
It is concluded that ALL injury is common in patients with acute ACL rupture and are statistically associated with ML injuries. The ability to visualize the ALL through the US was increased. There was a favorable result in the agreement between the side of the ACL injury and the visualization of the ALL by examination. There was agreement between the positive results in the pivot shift test and the findings of ALL lesion in the US. The presence of an LM lesion on MRI is associated with the presence of changes in these structures in the US. The data obtained suggest that the US contributes to the identification and assessment of the ALL integrity of the knee of patients with ACL injuries.
None.
The authors declare no conflict of interests.
This project was not sponsored.
None.

©2023 Nunes, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.