MOJ
eISSN: 2374-6939


Research Article Volume 2 Issue 3
Orland Park Orthopedics, USA
Correspondence: Blair A Rhode, Orland Park Orthopedics, 16450 S 104th AV, Orland Park, Illinois 60467, USA, Tel 708-364-8441, Fax 708-364-8443
Received: February 14, 2015 | Published: April 2, 2015
Citation: Rhode BA. Evaluation and comparison of eyelet durability in generic and brand PEEK rotator cuff anchors in porcine cortical and cancellous bone. MOJ Orthop Rheumatol. 2015;2(3):95-100. DOI: 10.15406/mojor.2015.02.00049
Purpose: Test the durability of molded-generic poly ether ether ketone (PEEK) anchors designed for rotator cuff repair in comparison to brand-name anchors.
Methods: 5.5 mm PEEK rotator cuff (RC) anchors double loaded with #2 ultrahigh molecular weight polyethylene (UHMWPE) sutures were inserted into porcine humerus cortical or cancellous bone.
Tests
Test outcomes were eyelet breakage, suture breakage, knot slippage, or anchor pullout.
Result: Tests were run on 10 brand PEEK anchors and 10 generic PEEK anchors with only one of the brand name anchors surviving longer than 181 cycles of a 10 to 180 N load repeated 3600 times while all the generic anchors completed the test. No eyelets on 250 generic anchors failed regardless of the number of force cycles used. Mean UFL for generic eyelet breakage was 422 N with a 36.1 N standard deviation. Sutures failed at knots, never due to abrasion at the eyelet. Anchors never pulled out of cortical bone while 18% of 100 anchors pulled out of cancellous bone at 4300 cycles on average.
Conclusion: Generic RC anchors demonstrate equivalent durability to that of brand anchors while offering a significant cost advantage.
Clinical Significance: The durability of generic-molded PEEK anchors ensures rotator cuff repair in patients will not be compromised while resulting in a significantly reduced cost.
Keywords: Rotator cuff, Anchors, PEEK, Durability
RC, Rotator Cuff; RCR, Rotator Cuff Repair; UFL, Ultimate Failure Load; N, Newtons; PEEK, Poly Ether Ether Ketone; UHMWPE, Ultrahigh Molecular Weight Polyethylene; SD, Standard Deviation; CI, Confidence Interval
Rotator cuff (RC) disease is one of the most frequently treated clinical problems in the U.S. It increases with age resulting in repairs more than doubling from 1996 to 2006.1 While there is a long history of treatment with a variety of approaches, arthroscopy has become the preferred surgical technique as it is the least invasive and results in faster patient recovery time.2 Rotator cuff tears repaired arthroscopically use anchors loaded with sutures and as such the biomechanical properties of these elements are of great importance to clinical outcomes.
Anchors have improved in performance as designs and materials have evolved. Notable is the use of Polyetheretherketone (PEEK) for anchors because it is a chemically resistant crystalline thermoplastic material that is radiolucent, it is not biodegradable, and it is drillable when revision surgery is required. Performance and costs are clinically relevant parameters of RC anchors. Rotator cuff repair (RCR) costs can be addressed with the use of $69 generic anchors versus brand anchors costing as much as $450.
In a recent study of anchors inserted in fresh porcine humerus, the frequency of eyelet breakage was judged design dependent based on mechanical testing of various combinations of sutures and anchors.3,4 Eyelets were the weakest element of anchors and therefore their performance is a primary concern.
Biomechanical testing of 5.5 mm molded-generic RC anchors double loaded with ultrahigh molecular weight polyethylene (UHMWPE) #2 sutures was performed here after anchor insertion into porcine cortical and cancellous bone. Tests of anchors inserted in cortical bone focused exclusively on the durability of the anchor eyelets. Tests of anchors inserted in cancellous bone focused on pullout frequency. Tests employing a high number of cycles focused on possible anchor weaknesses that may occur infrequently. Generic anchor performance is also compared to that of brand anchors.
Hypothesis
H0: Molded-generic 5.5mm PEEK RC anchors are equivalent to brand RC anchors as measured by number of cycles to failure, ultimate failure load (UFL), eyelet failure or anchor pullout.
Porcine shoulders were obtained from a wholesale meat market. Humeri were frozen until use and then warmed to room temperature. Test parameters used in studies of rotator cuff repair were based on estimates of the maximum force on human supraspinatus tendons to be approximately 300 Newtons (N).5 180 N has been estimated to be 2/3 of the maximum load of a maximum contraction of the rotator cuff.6–9 Test parameters for the present study were chosen based on this estimate and parameters used in a biomechanical study of anchor performance that cycled the load from 10 to 180 N 3500 times or until failure.10 Pull rate was 635 mm/min (10.5 mm/s) similar to the pull rate used in a recent cyclic test of anchors.4
Bone was tapped using each manufacturer’s tap to the depth of the laser line. Anchors double loaded with UHMWPE sutures were inserted at an approximately 75° angle11 until the laser line on the inserter aligned at the surface of cortical or cancellous bone (Figure 1). Anchor suture openings were oriented perpendicular to the line of suture pull.12,13 Sutures were passed over a metal rod in the upper grip of the test instrument and tied with eight alternating half-hitches. Tests were conducted using a measurement test instrument (Test Resources 225LB Actuator, Shakopee, MN, USA). Test sequences were: Test1- force cycled 100 times while recording load and displacement for each cycle; Test2- force cycled 3500 times while recording results at a rate of 100 samples/s for every 20th cycle due to DOS program storage limitations. Test2 was repeated three times for anchors in cancellous bone to determine whether anchors would pullout at some point; Test3- Ultimate Failure Load (UFL). Test outcomes were categorized as UFL in Newtons (N), eyelet break, knot slippage, suture break, or anchor pullout. A preliminary study was conducted to ensure that generic anchors had UFLs comparable to brand anchors. The study determined UFL mean and its SD for 15 generic anchors tested in cortical bone using a 10 to 100 N load repeated 200 times, the same parameters used previously.4 A Student’s t-test for unequal counts and SDs was used to determine group differences requiring a P-level < 0.05 for statistical significance (t-test computed using Graphpad).14
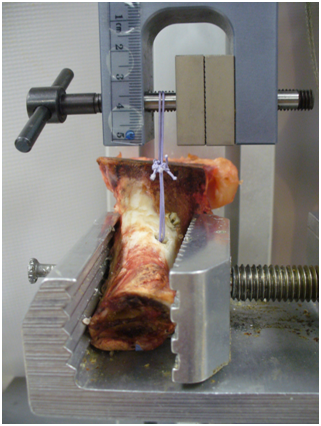
Figure 1 Test setup illustrating a pig humerus in the vise with sutures threaded through the eyelet and around the shaft of the upper grip of the test instrument. A shaft placed through the edge of the vise and through the bone prevented the bone from pulling out the vise when the UFL force was greater than 300 N. The head of the humerus was removed so that the upper grip of the test instrument could approach the anchor in cortical bone within 40 mm, the length of the sutures used in the tests.
Study 1
10 RC PEEK Corkscrew® FT-Optima 5.5 mm x 14.7 mm anchors purchased for $274 (Arthrex, Naples, FL. USA), PEEK material supplied by Invibio. 10 $69 RōG (Rhode’s Orthopedic group, Orland Park, IL) molded-generic PEEK 5.5 mm x 14.8mm RC anchors. PEEK supplied by Zeniva in compliance with ISO 13485. Anchors were inserted into cortical bone and subjected to Tests 1-3. Corkscrew FT anchors were chosen for comparison because they were not previously tested.3,4
Study 2
To minimize small sample size outcome limitations in establishing the likelihood of eyelet breakage or any other rare failure, sample size was increased to 100. Generic anchors were inserted into cortical bone and subjected to Tests 1-3.
Study 3
To establish the likelihood of generic anchor pullout, 100 anchors were inserted into cancellous bone and subjected to Test1, three repetitions of Test2 (10,500 cycles), and then Test3. Up to 8 anchors were inserted into each head of porcine humerus spaced at least 1 cm apart.
Study 4
Due to the lack of generic anchor eyelet breakage in the first three studies except in the UFL test, 25 additional anchors inserted into cortical bone were subjected to 10,600 cycles and 10 additional anchors were subjected to between 18,000 and 100,000 cycles to determine if there was a point at which anchors failed for any reason.
Preliminary study
The UFL test for 15 generic anchors resulted in a mean UFL of 451 N, standard deviation (SD) of 57.5 N, and confidence interval (CI) for mean is 336 to 566 N. These results are comparable to UFL values for 5.5mm PEEK anchors reported in Table 1 of a prior study.4
|
Arthrex |
Arthrex |
RōG Generic cycles completed |
RōG Generic |
|
|
|
182 |
|
3600 |
489 |
|
|
9 |
|
3600 |
526 |
|
|
43 |
|
3600 |
446 |
|
|
12 |
|
3600 |
381 |
|
|
35 |
|
3600 |
408 |
|
|
35 |
|
3600 |
417 |
|
|
5 |
|
3600 |
435 |
|
|
1 |
|
3600 |
420 |
|
|
27 |
|
3600 |
398 |
|
|
|
400 |
3600 |
466 |
|
Mean |
38.8 |
|
3600 |
431 |
|
STDEV |
55.8 |
|
0 |
46 |
|
Min |
1 |
|
3600 |
381 |
|
Max |
182 |
400 |
3600 |
523 |
Table 1 Eyelet durability test results for Arthrex and RōG PEEK anchors
Test results for Arthrex and RōG anchors inserted into porcine cortical bone: Arthrex PEEK Corkscrew FT 5.5mm, Naples, FL; RōG 5.5mm PEEK anchors, Orland Park, IL. Standard tests: (1) 100 cycles, 10 – 180 N, 635 mm/min; (2) 3500 cycles, 10 – 180 N, 635 mm/min; (3) UFL at 635 mm/min. 8 Corkscrew anchors failed during the initial 100 cycle test due to suture pullout, one anchor completed 82 cycles of test 2 for 182 total cycles, 1 anchor completed all 3 tests with UFL=400 N. All 10 RōG anchors completed all three tests with all eyelets breaking at an average UFL=431 N. t-test of anchor break UFLs not possible with an n=1 for Corkscrew anchors. t-test of the number of cycles to suture pullout results in P < 0.0001 given that no RōG generic anchors had a suture failure (3600 cycles, n=10) versus Corkscrew anchor sutures pulling out of the anchor intact at 38.8 cycles on average (n=9).
Study 1: Comparative performance of two manufacturer’s RC anchors
Ten 5.5mm PEEK Corkscrew FT anchors (Arthrex) and ten RōG 5.5 mm molded-generic RC anchors were inserted in cortical bone. Outcomes of the three tests varied considerably as seen in Table 2 where a single Corkscrew FT anchor completed all three tests with a UFL of 400 N, one Corkscrew anchor failed on the initial pull at 149 N and the other 8 failed by the intact suture pulling out of the anchor at an average of 38.8 cycles, 55.8 cycle SD, and a range of 1-182 cycles. All generic anchors passed Tests 1-3 with eyelet mean UFL=431 N, 46 N SD, and CI for mean is 339 to 523 N. A t-test of group UFLs could not be calculated because at least two samples in each group are required to calculate a P-value. An alternative t-test based on the number of cycles to failure in Table 2 resulted in P<0.0001.
|
Exp. No. |
Cycle count |
UFL (N) eyelet break |
UFL (N) suture break |
|
1 |
18000 |
|
|
|
2 |
20000 |
|
395 |
|
3 |
20000 |
|
565 |
|
4 |
20000 |
|
353 |
|
5 |
20000 |
382 |
|
|
6 |
20000 |
|
381 |
|
7 |
40000 |
480 |
|
|
8 |
50000 |
550 |
|
|
9 |
99750 |
410 |
|
|
10 |
100000 |
498 |
|
|
Count |
10 |
5 |
4 |
|
Average |
40775 |
464 |
424 |
|
Min |
18000 |
382 |
353 |
|
Max |
100000 |
550 |
565 |
|
SD |
32910 |
68 |
95 |
Table 2 High cycle count test of generic anchor durability
10 generic anchors were subjected to the cycle counts listed in column 2 to determine whether there was a point at which they would succumb to fatigue. While attempting to attain 20,000 cycles for anchor #1 without a break in the testing the Test instrument burnt out. After the instrument was repaired the testing paradigm was altered so that the 10-180 N force was repeated in blocks of 5000 cycles until the total count was attained. Sutures fatigued at 99,970 cycles for the #9 anchor, the anchor was removed then reloaded with sutures, then reinserted to obtain a UFL (this was the only instance of reloading sutures in this study). The mean UFL for eyelet breaking is 464 N with SD=68 N. The results are close to those obtained for the first three studies. Suture break mean UFL=424 N provides an underestimate of the eyelet break UFL. UFL results indicate neither anchors nor eyelets would fail for conditions that a human rotator cuff repair will ever encounter.
Study 2: 100 generic anchors tested in cortical bone
In small sample studies all possible outcomes may not be observed if they have a low probability of occurrence. To ensure that generic anchors do not exhibit any low probability flaws, 100 anchors were subjected to Tests 1-3. 83 eyelets broke at a mean UFL of 413 N, 35 N SD, and CI for mean of 343 to 483 N; 17 sutures broke at a mean UFL of 454 N, 65 N SD, and CI for mean of 324 to 584 N. Because suture break force is an underestimate for eyelet breakage, the UFL results were combined resulting in a mean UFL of 420 N.
Study 3: 100 generic anchors tested in cancellous bone
Because anchor pullout from human cancellous bone is an undesirable RCR outcome that could result from anchor design, generic anchor pullout was tested after insertion into cancellous bone of porcine humeri. After Test1, Test2 was repeated 3 times resulting in a total of 10,600 cycles to increase the likelihood of anchor pullout. Cancellous bone was variable in hardness, demonstrated by all anchors pulling out of one humerus while no anchors pulled out of another humerus. Humerus size appeared to be the principal factor contributing to pullout frequency. Averages for five possible test outcomes were: 59 eyelets broke at 430 N, 15 sutures broke at 383 N, 7 anchors pulled out during the UFL test at 393 N, 18 anchors pulled out at an average of 4300 cycles with a range of 141 to 10451 cycles. In one instance the sutures broke at 9000 cycles.
Study 4: 35 generic anchors in cortical bone tested with 10,600 to 100,000 load cycles
25 generic anchors in cortical bone passed the identical durability test used for anchors in cancellous bone, 10 -180 N for 10,600 cycles. Mean UFL for the 23 anchors that completed the full cycle count was 458 N, SD of 58.3 N with CI for mean of 341 to 575 N. There were nine instances of suture breakage at a mean UFL of 423 N, SD of 55.5 N with CI for mean of 312 to 534 N. All suture breaks occurred at the knots. Because no eyelets broke before 10,600 cycles, ten anchors were then tested using higher cycle counts to determine whether there is a point at which anchors or eyelets break down (Table 1). Six anchors were cycled 20,000 times before the UFL test with no early breakdown. Mean anchor-eyelet UFL was 464 N, SD of 67.9 N with CI for mean of 328 to 600 N. Cycle count was increased for four anchors to 40000, 50,000, 99,750, and 100,000 times respectively, again no breakdowns. Sutures fatigued at 99,750 cycles for the #9 anchor, the anchor was then reloaded with sutures to obtain a UFL=410 N.
Generic anchor test results summary
Combining results of the preliminary test and the four studies, 250 anchors were subjected to a cumulative total of nearly 2,000,000 cycles of a 10 to 180 N force without an eyelet break. No UHMWPE sutures wore out at the eyelets even after as many as 100,000 cycles. The entire distribution of eyelet break UFLs is significantly higher than the 180 to 250 N maximum force that a human supraspinatus tendon will likely experience (Figure 2). The 325 N minimum UFL of the distribution is nearly twice the frequently cited near maximum 180 N supraspinatus load providing a significant safety factor.
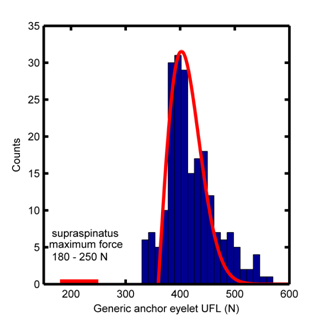
Figure 2 Distribution of generic anchor eyelet UFLs tested in four studies (n=217 eyelet breaks out of 250 anchors tested). The red bar indicates the range of the maximum force estimates that the human supraspinatus muscle will experience.9,17 The mean UFL is 424 N with SD of 42.4 N and the distribution appears to be best approximated by a Rayleigh distribution that is skewed to the right and represented by the red curve (http://en.wikipedia.org/wiki/Rayleigh).
Comparing the results of biomedical mechanical testing of a generic-molded-PEEK RC anchor to those for the Corkscrew FT anchor demonstrated that the generic anchor could endure substantially greater loads that were repeated for many cycles. The Corkscrew FT anchor was shown to be prone to early suture pullout from the anchor while the suture remained intact in all but one instance in which a UFL of 400 N was obtained. Direct comparison with other RC anchors is limited due to cost considerations and the fact that most brand anchors had been tested.3,4 Generic anchor test results are therefore compared to publish UFLs for several brand anchors in Table 3 noting that the published and current results were both obtained using calibrated measurement test instruments.4
|
Anchors 5.5 mm |
UFL (N) n=10 |
SD (N) n=10 |
Range (N) n=10 |
t-test of H0 Pr(a) |
Eyelet break n=20 |
Suture break n=20 |
Anchor pullout n=20 |
|
Healicoil PK |
298.7 |
37.4 |
244-355 |
.0001 |
20 |
|
|
|
Quattro X |
370.6 |
26.8 |
323-409 |
.0004 |
19 |
|
1 |
|
Reel X |
384 |
66 |
339-501 |
.013 |
6 |
11 |
3 |
|
Healix PEEK |
404.3 |
24.4 |
356-451 |
.067 |
18 |
2 |
|
|
Foot Print Ultra |
453.7 |
71.2 |
331-548 |
.089 |
|
6 |
14 |
|
Twin Fix PK |
469.4 |
48.7 |
394-563 |
.813 |
20 |
|
|
|
Quattro Link |
482.3 |
35.6 |
442-550 |
.146 |
|
17 |
3 |
|
Generic (n=15) |
451.4 |
57.5 |
355-556 |
|
12 |
3 |
|
Table 3 Ultimate Load to Failure performance of PEEK 5.5mm rotator cuff anchors
The H0 hypothesis that there is no difference in mean force to failure between generic and brand anchors is true for four brands of anchors where the p-value is greater than the customary P<0.05 criteria for significance. Three brand anchors have significantly lower UFLs than the generic anchor based on highly significant t-test P-values between 0.0001 and 0.013. Generic anchors were tested with 10-180 N load repeated at least 3600 times in comparison to brand anchors tested with a 10-100 N load repeated 100 times.
Mechanical testing of 250 $69 generic-molded PEEK anchors using a 10 to 180 N force cycle repeated more times than a human RCR would endure during the healing period, demonstrated no anchor design weakness. No eyelets ever broke nor did any sutures abrade at the eyelets in anchors subjected to nearly 2 million total test cycles. No anchor body breakage or pullouts occurred when inserted in cortical bone. When anchors were inserted into cancellous bone, eyelets broke during the UFL test in 59% of 100 anchors. Anchors pulled out of cancellous bone 18% of the time at an average of 4300 cycles of the 10 – 180 N load which is significantly greater than a RCR would be subjected to during the healing phase. A previous study of RCRs concluded that condition of the tissue or bone was the limiting reason for repair failure.15–17 High UFLs and the high number of cycles before pullout of generic anchors from cancellous bone indicate the anchors will not be the limiting factor of RCRs.
Molding PEEK anchors eliminates a more expensive machining process. The overall cost reduction based on the use of generics opens up the possibility of significant savings which increase as the number of anchors increases for large RC tear repairs. The transition to Orthopedic generics parallels the occurrence in pharmaceuticals. Costs will be especially important when federal healthcare rules are enforced and the fact that RCRs are becoming more frequent as the population ages.
Limitations
In the interest of assessing anchor eyelet breakage with other modes of failure removed, anchors were placed in porcine cortical humerus bone which not analogous to human humerus bone. The use of porcine cancellous bone to focus on anchor pullout tendency is an approximation of RCR conditions encountered clinically especially in older patients.
Generic RC anchors demonstrate equivalent or better durability to that of brand anchors while offering a significant cost advantage. Generic anchor eyelets exhibit no fatigue or breakage issues when tested at conditions that exceed those that patients would experience under normal shoulder use. There was no wear of UHMWPE sutures at the eyelets.
Generic anchors will not limit RCRs and any failure will result from the quality of the tissue and bone. Significant cost savings result from their use.

©2015 Rhode. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.