MOJ
eISSN: 2374-6939


Clinical Report Volume 13 Issue 3
1Chief Consultant, Bari-Ilizarov Orthopaedic Centre,Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Bangladesh
2MD; FCPS, Prof., Bari-Ilizarov Orthopaedic Centre, Bangladesh
3MD (Ortho), MS (Ortho), Consultant, Orthopaedics, NITOR, Bangladesh
4Medical officer, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Mofakhkharul Bari, Bari-Ilizarov Orthopaedic Centre, 1/1, Suvastu Shirazi Square, Lalmatia Block E, Dhaka-1207, Bangladesh, Tel +8801819211595
Received: March 06, 2021 | Published: June 17, 2021
Citation: Bari MM, Shahidul I, Tanvir AM, et al. Correction of post septic equinus deformity of left ankle subluxation in combination with 1st metatarsophalangeal joint deformity of 90° downwards with 7 cm L.L.D of left leg, with bad scar and hard skin discoloration in dorsum of great toe. MOJ Orthop Rheumatol. 2021;13(3):54-58. DOI: 10.15406/mojor.2021.13.00548
Severe equinus deformity of left ankle and 90° deformity to the plantar surface in the left metatarsophalangeal joint can cause a compression and stretch in the whole great toe. As a result, the skin became hard and discolored in the dorsum of the great toe; the patient’s gait was awkward and with painful limping.1–6
Keywords: post-septic, equinus, 1st metatarsophalangeal joint, tibia, deformity, Ilizarov apparatus
A 20 years old male underwent childhood injection following a septic ankle swelling and pain, which his parents could not explain exactly, as because they are not literate. Severe equinus deformity developed and 7 cm L.L.D was measured in the leg. His parents came to my Bari-Ilizarov Orthopaedic Centre with their boy for correction of ankle equinus, 90° plantar flexion deformity of 1st metatarsophalangeal joint and 7 cm L.L.D of tibia.8
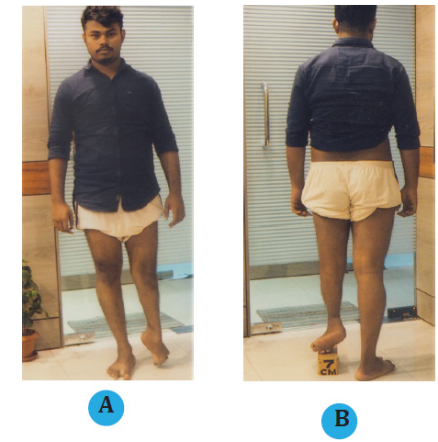

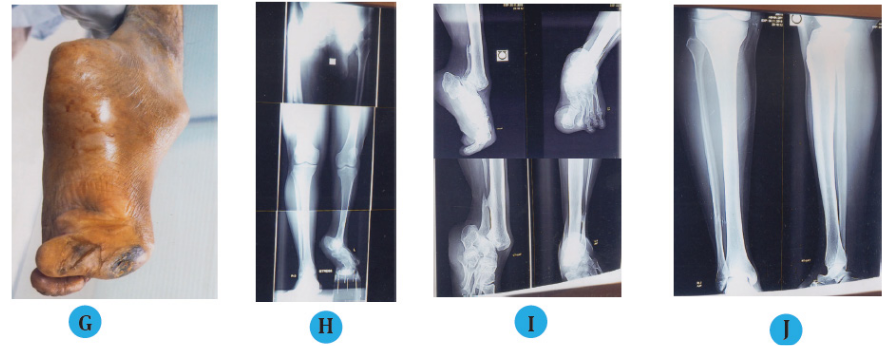
Figure 1 20 years old male, post septic equinus deformity of le ankle subluxation in combination with 1st metatarsophalangeal joint deformity of 90° downwards with 7 cm L.L.D of le leg, with bad scar and hard skin discoloration in dorsum of great toe.
(A, B) Preoperative photograph of left leg of the patient with post septic equinus deformity of left ankle, 1st metatarsophalangeal Joint deformity of 90° downwards with 7 cm LLD of a 20 years old male (front and back view).
(C) Ankle subluxation in combination with 1st metatarsophalangeal joint deformity of 90° downwards.
(D) Right and left foot with downwards displacement of great toe with discoloration of the skin.
(E, F) Plantar surface of the foot and great toe (AP and lateral view).
(G) Hard and discolored skin over the dorsum of the great toe.
(H) Stress radiographic view of lower limb with post septic equinus deformity of left ankle with 7 cm LLD, with 90° downwards displacement of great toe.
(I) Radiographic view of equinus ankle and 90° downwards displacement great toe.
(J) Radiographic view of normal right tibia and ankle for comparative study.
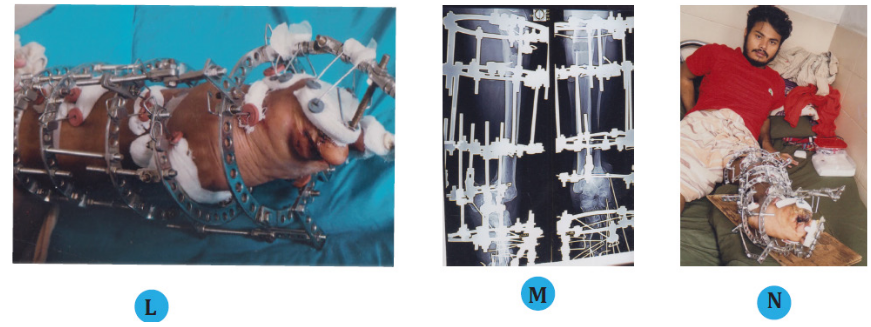
(L) Clinical photo of the left foot after 21 days of application of mini Ilizarov.
(M) Radiograph of left foot after application of the mini Ilizarov.
(N) Clinical photos of the patient with mini Ilizarov.
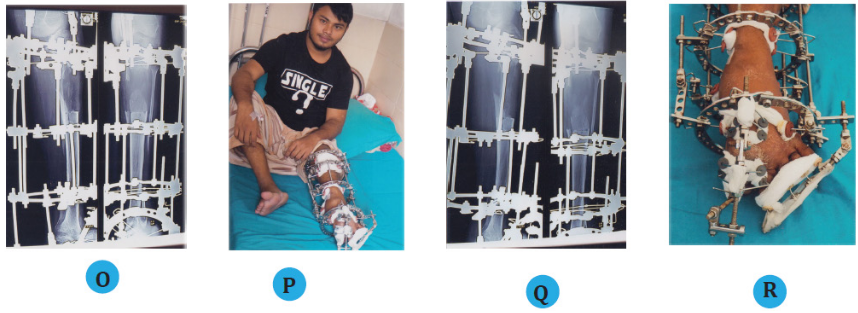
(O) Radiograph after 2 months with mini Ilizarov in the left leg with lengthening regenerate.
(P) Clinical photo of the patient with mini Ilizarov after 3 months.
(Q) Radiograph of left leg after 3 months with good regenerate.
(R) Clinical photo of the left ankle with almost corrected 1st metatarsophalangeal joint.


(S) Stress radiographic view of lower limb after correction of the ankle equinus, left 1st metatarsophalangeal joint 90o deformity correction with equalization of 7 cm L.L.D.
(T, U) Clinical appearance of the patient with brace (Front and back view).
(V, W) Final standing clinical appearance of the patient with ankle equinus and 1st metatarsophalangeal joint correction.
Doing lengthening of tibia equinus may happen and to prevent that we are correcting simultaneously the equinus deformity also by distracting the posterior two hinges in the calcaneal region.
None.
All authors declare no conflicts of interest.
There is no funding source.

©2021 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.