MOJ
eISSN: 2374-6939


Case Report Volume 15 Issue 3
1Department of Clinical Education and Training, Kaohsiung Medical University, Chung-Ho Memorial Hospital, Kaohsiung, Taiwan
2Department of Physical Medicine and Rehabilitation, Taichung Veterans General Hospital, Taichung, Taiwan
3Department of Post-Baccalaureate Medicine, College of Medicine, National Chung Hsing University, Taichung, Taiwan
4School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
5Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
6Department of Physical Medicine and Rehabilitation, Tri-Service General Hospital, Department of Physical Medicine and Rehabilitation, School of Medicine, National Defense Medical Center, Taipei, Taiwan
Correspondence: Shin-Tsu Chang, MD, MS, PhD, Department of Physical Medicine and Rehabilitation, Kaohsiung/ Taichung Veterans General Hospital, Taichung, Taiwan; Department of Physical Medicine and Rehabilitation, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taipei, Taiwan , Tel 886-935-605-578
Received: May 15, 2023 | Published: May 31, 2023
Citation: Wang TT, Chu CW, Cheng YY, et al. Concurrence of longitudinal melanonychia and numbness in a patient with left hemiparesis suffering from thumb injury by clamp during performing occupational therapy. MOJ Orthop Rheumatol. 2023;15(3):104-106. DOI: 10.15406/mojor.2023.15.00627
Numbness within the thumb involving the palmar aspect with the three and a half digits as the division is a common presentation of peripheral nerve injury. However, it is rarely observed to be presented with numbness at half of the ulnar-palmar side of the thumb, where the longitudinal melanonychia on the nail plate acts as the division. We present a case that reveals concurrence of longitudinal melanonychia and numbness suffered from a thumb injury during the course of occupational therapy.
Keywords: longitudinal melanonychia, numbness, malpractice, thumb injury, rehabilitation, occupational therapy
In rehabilitation programs involving tool-use training, the clamp, which has been a piece of equipment for occupational therapy, is commonly used and often implemented for improving stability in the thumb and fingers, as well as strengthening of the flat pinch in order to enhance daily functions.1 Sufficient fine motor strength is essential, whether it be maintaining a grasp on a pencil or buttoning buttons; particularly in patients with hand spasticity, as it intensifies the effects of stretching exercises and the injection of muscle-relaxants, such as Botox.2
However, there was never a report to present any malpractice evidence surrounding use of the clamp during the performing of the patient’s occupational therapy. We herein present a case where the patient was suffering from longitudinal melanonychia together with numbness after such an event.
Our case centers around a 37‐year‐old Asian female experiencing underlying disease due to an old right intracranial hemorrhage at the right basal ganglia with left spastic hemiplegia,and subsequent hand deformity in the form of a clenched-like fist. She was admitted for inpatient rehabilitation involving tool-use training and spasticity reducing in her left-sided fingers. During rehabilitation, her left thumb was compressed by the rebound force of the clamp (Figure 1). Because she could only adopt a lateral pinch rather than flat pinch to operate the equipment due to her hand deformity (Figure 2). Over the period of two weeks, a brown to black, longitudinal1mm-wide streak appeared on the nail plate of her injured left thumb (Figure 3), which was confirmed as longitudinal melanonychia by our dermatologist. After detailed observation, it was determined that there was no periungual pigmentation, no nail dystrophy, nor any other associated nail lesions such as onycholysis, warty mass or hyperkeratosis. Simultaneously, the patient reported numbness at the palmar aspect of the ulnar (exact half) side of the left thumb, with the dark-colored line on the nail plate acting as the division. Numbness had developed under the dark line of the left palmar thumb, which was near the side of the index finger (Figure 4). Interestingly, numbness did not involve the other half of the thumb. This sensation continued for more than two months with no improvement, even after the application of a hot compress and rest. Six months later, the above condition gradually improved.

Figure 2 Injury site of this case. The female patient’s left thumb was compressed by the rebound force of the clamp (X). The patient adopts a lateral pinch rather than a flat pinch to operate the equipment due to her clenched-like fist.
The clamp is a popular type of equipment for use by patients with hand disorders,3–5 but its use had never been previously reported in a malpractice case such as ours. To the best of our knowledge, our case is the first to report on a patient who experienced numbness at the palmar aspect of the ulnar (exact half) side of the left thumb, as well as longitudinal melanonychia. Therefore, when operating the clamp during use of the occupational therapy equipment, it is necessary to be aware of the intensity, frequency, and duration of the therapy. Additionally, it has been recommended by therapists to moderately reduce the intensity of training in patients who are inattentive or display low compliance; otherwise, the results may see a similar consequence much like our case.
With regards to longitudinal melanonychia, information obtained both upon onset and during progression, as well as probable triggers for her melanonychia, were all intactly obtained from the patient. The exact diagnosis of longitudinal melanonychia commenced a detailed examination of all the fingernails in order to assess color and width of the band(s), color homogeneity, presence of signs of trauma or infection, presence of a Hutchinson's sign (refers to pigment extending to the periungual skin), as well as the presence of any other nail lesions.6 Based upon the dermatologist’s examination and the algorithm proposed by Rich,6 diagnosis of this case did not require a biopsy as a further invasive approach due to the single nail lesion width being < 3mm.
With the exception of a local injury accident, the patient did not have any other conditions associated with longitudinal melanonychia, such as pregnancy, nail biting, history of psoriasis, amyloidosis, phototherapy, or other conditions.7 In addition, while melanoma was one of our considerations, the clinical features which raise any suspicions of melanoma were absent. After a complete evaluation, the etiology of melanonychia in this case was strongly related to the thumb injury which occurred during operation of the clamp.
Along with the consequence of melanonychia, the thumb injury was also accompanied by numbness at the palmar aspect of the ulnar side of the left thumb. After comprehensively evaluating both the distribution of the numbness and the injury site reported by the patient, the numbness was recognized as contributing to the acute trauma of the ulnar proper palmar digital nerve of the thumb. According to the Gray's Anatomy Textbook, Figure 5 is schematized to illustrate the anatomic pathology of sensory innervation in the injured thumb. The acute compression results in nerve damage, reduced conductivity of nerve impulses, and eventually the presence of numbness in the distribution of the ulnar proper palmar digital nerve of the thumb.8 Peripheral nerves can easily get injured owing to acute compression, which in turn may bring about sensory deficits and even lifelong disability.9 Consequently, during operation of the clamp, it is highly recommended that the patient discontinue therapy prior to reaching the point of fatigue, which will therefore prevent further harm.
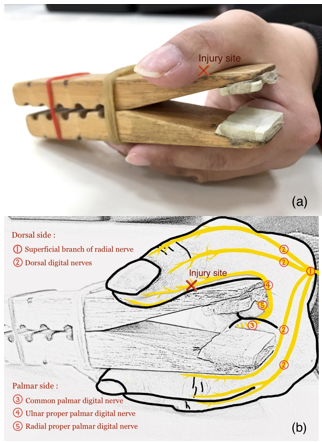
Figure 5 Injury site of compression force and schematic illustration of sensory innervation of fingers. (a) The patient’s left thumb was compressed by the rebound force of the clamp. (b) Patient’s numbness is recognized as contributing to acute trauma of the ulnar proper palmar digital nerve of the thumb.
Our case provides the first report presenting a malpractice case with regards to use of a clamp, where complications involving thumb numbness and longitudinal melanonychia occur. While operating a clamp during occupational therapy, it is necessary to be aware of the intensity, frequency, and duration of the therapy; otherwise, another patient may experience similar consequences as this case.
None.
The authors declare no conflicts of interest.

©2023 Wang, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.