MOJ
eISSN: 2374-6939


Case Report Volume 4 Issue 1
Department of Orthopaedics, Mumbai Port Trust Hospital, India
Correspondence: Rohit Dharmadhikari, Department of Orthopaedics, Mumbai Port Trust Hospital, Wadala, Mumbai-400037, Tel 920000000000
Received: December 13, 2015 | Published: January 18, 2016
Citation: Dharmadhikari R, Gokhale A (2016) Symptomatic Bilateral Cervical Perineural Cyst. MOJ Orthop Rheumatol 4(1):00127. DOI: 10.15406/mojor.2016.04.00127
Perineural cysts are commonly found in the sacral region as asymptomatic lesions. Cervical perineural cysts are rare and there is no reported case of symptomatic bilateral cervical perineural cyst. There is controversy regarding the management of these cysts. Surgical and nonsurgical treatment is associated with complications. The objective of the present study is to present a rare case of symptomatic bilateral cervical perineural cyst treated by oral steroids and to discuss various aspects including management of perineural cyst. We conclude that cervical perineural cyst may be a cause of upper limb pain. Steroid therapy may be considered as an alternative treatment for smaller cysts (< 1.5 cm).
Keywords: Perineural Cyst, Tarlov Cyst, Steroid
Perineural or Tarlov cysts were first described by Tarlov.1 in 1938 during his autopsy studies of the filum terminale.1 Studies have shown the prevalence of these cysts to vary from 4.6% in some to upto 9% in others.2,3 Although most of these lesions are asymptomatic, on rare occasions, they may cause local or radicular pain, dysesthesia or paresthesia, paresis and bladder or bowel dysfunction. The ability to diagnose perineural cyst as a cause of neurological dysfunction has been enhanced by CT and MRI.
Although there is consensus that asymptomatic cysts should be followed, there is controversy regarding the methods of treatment of symptomatic cysts. Nonsurgical methods like CSF drainage and CT guided cyst aspiration are associated with recurrence.2,4,5 Surgical methods like decompressive laminectomy, cyst and nerve root excision and incision and drainage of the cyst with imbrications are associated with neurological deficit and surgical failures.4,6
The case of a 35-year-old male with symptomatic cervical perineural cysts treated with oral steroids is presented and the literature reviewed. To the best of our knowledge, this is the first case of symptomatic bilateral cervical perineural cyst in the literature.
History: This 35-year-old male carpenter presented with pain in neck radiating to left upper arm since 1 year and right upper arm since 8 months. The patient also complained of paresthesia along the top of shoulder to outer aspect of arm in both upper limbs. The pain was rated 8/10 on visual analog scale. It worsened on doing work and was only partially relieved with rest.
Examination
There was no tenderness to palpation of the cervical spine. The tone and motor power were normal in all muscle groups. The biceps jerk was 1+ on left side; rest of the deep tendon reflexes was 2+ and symmetrical. Sensations were intact.
Radiology and neurophysiology findings
Plain radiographs showed no abnormalities. MRI of the cervical spine was done. Sagittal T2W images showed hyperintense lesion at both C5-C6 neural foramen (Figure 1 & 2). Axial T2W images showed bilateral cervical perineural cyst at C5-C6 neural foraminae (Figure 3A & 3B). Post-contrast study showed no abnormal enhancement along the cysts. EMG-NC studies showed evidence of C5C6 chronic motor axon degeneration at root level. Left deltoid and biceps showed high amplitude large duration motor unit potentials during voluntary activity.
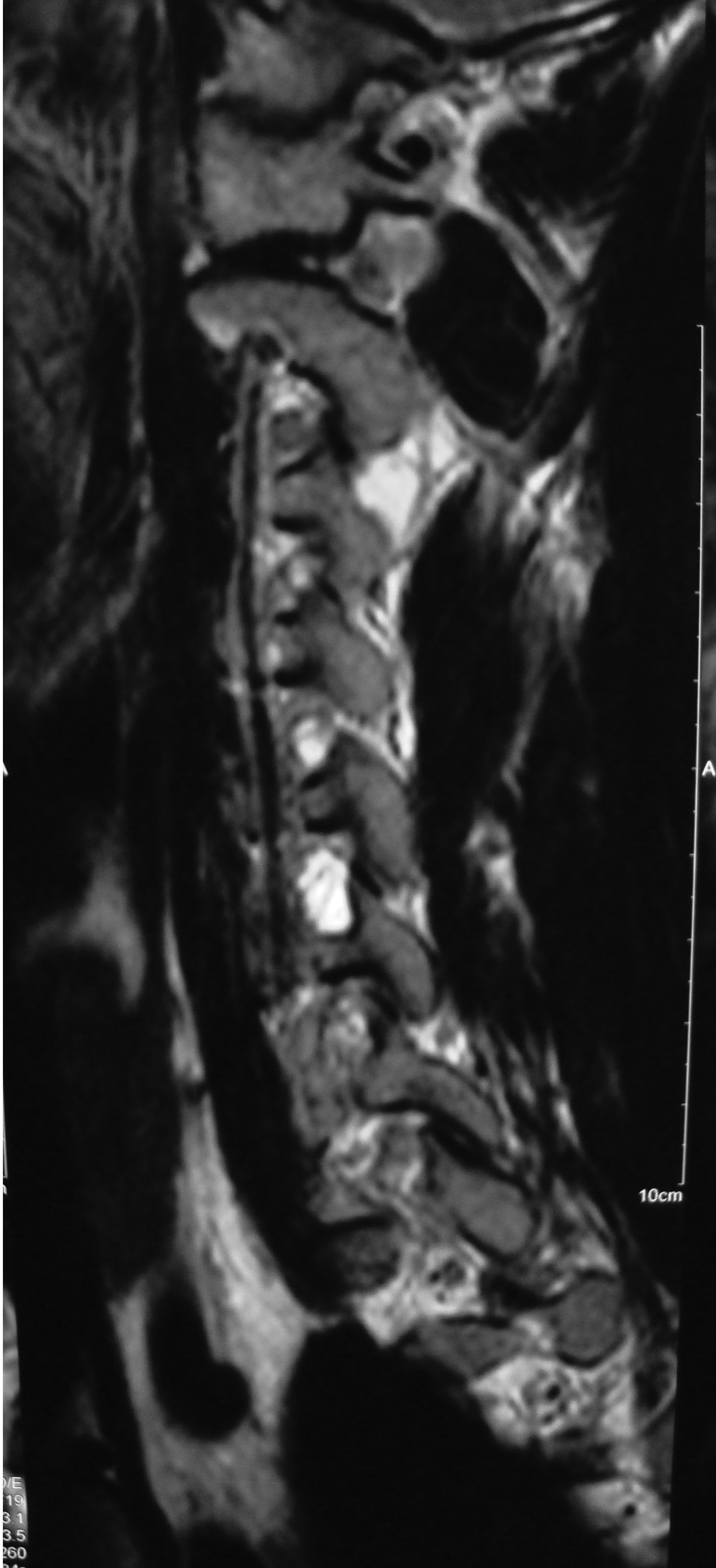
Figure 1 Sagittal T2W image of the cervical spine showing hyperintense lesion at C5-C6 neural foramen corresponding to the right perineural cyst.
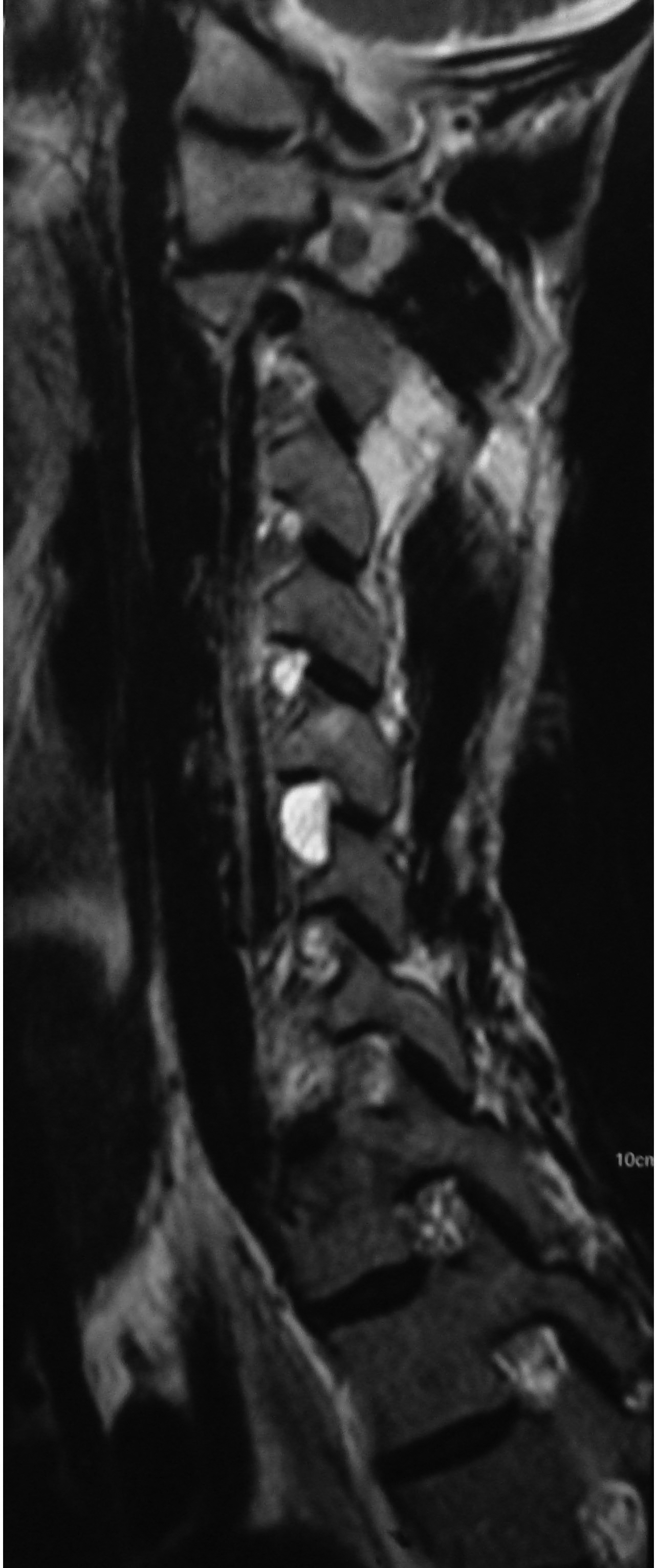
Figure 2 Another sagittal T2W image of the cervical spine showing similar hyperintense lesion at C5-C6 neural foramen corresponding to the left perineural cyst.

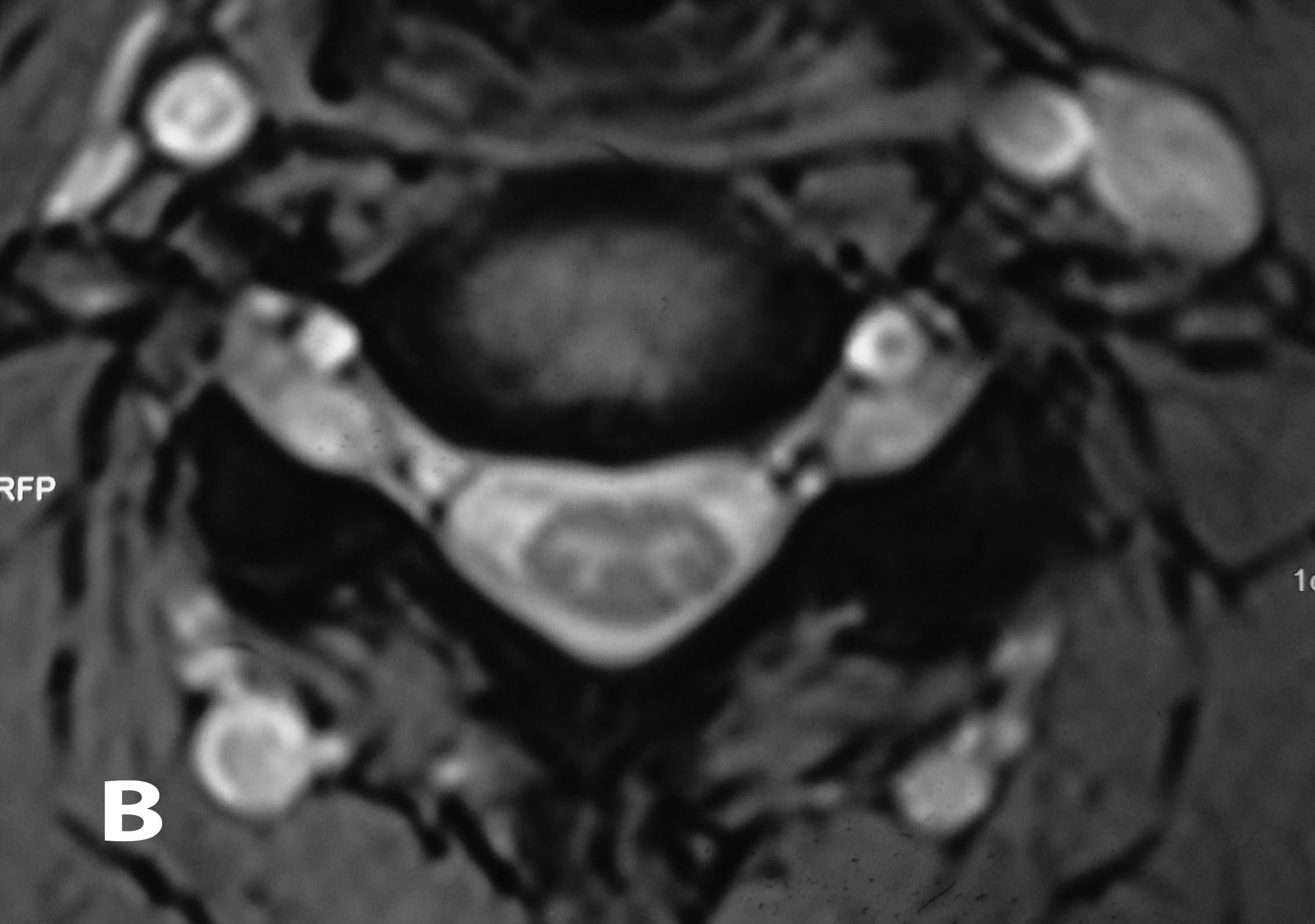
Figure 3A & B Axial T2W images of the cervical spine demonstrating bilateral cervical perineural cyst at the C5-C6 level.
Treatment
The patient was treated with a 6-day course of oral steroids, tapered from 24mg to 0mg. The patient had relief of symptoms with reduction of pain to 1/10 and return to work. At 6-month follow-up, the pain gradually increased to 6/10, but there was no neurological deterioration.
Perineural cysts form between the endoneurium and perineurium at the junction of the dorsal ganglion and the posterior nerve root. The lining of these lesions contains nerve fibres and they are not in contact with the CSF of the subarachnoid space. They have been classified by Nabors,et al as Type 2 or “extradural meningeal cysts with spinal nerve root fibres”7 and by Goyal,et al as category 1 of intraspinal cysts.7
The proposed etiologies for the perineural cysts include ischaemic degeneration, inflammation, hemorrhage, trauma, arachnoid proliferation, obstruction of perineural lymphatic flow or developmental origin.1,3,8-11 Several authors have proposed that increased CSF hydrostatic pressure may be a factor in the origin of perineural cysts or their growth and becoming symptomatic.4,12,13 The patient in this study had a history of heavy lifting at work-maneuver that raises CSF pressure.
Although usually diagnosed as incidental findings, 20% of perineural cysts are symptomatic1. Various studies indicate that women develop symptomatic perineural cysts more often than men.9,10,13 MRI is considered as the gold standard for diagnosis and is more sensitive than CT myelography.14,15
There is no consensus on the optimal management of symptomatic perineural cysts. Nonsurgical methods include lumbar CSF drainage to decrease the hydrostatic pressure.4 However symptoms recur after drainage is stopped.4 Although cyst aspiration relieves symptoms, it is often only temporarily effective.2 Reduction of the cyst wall or insertion of fat into the cyst have failed due to cyst reinflation.16 Percutaneous fibrin glue therapy is effective in resolution of symptoms, but is associated with postprocedural aseptic meningitis.5
Surgical treatment options include deompressive laminectomy, cyst wall resection, cyst fenestration and imbrication and cyst shrinkage using bipolar cautery.9,12,17-19 However complications like postoperative pseudomeningocele and neurological deficits occur. Usually patients with larger cysts (>1.5cm) and associated radiculopathy benefit from surgery.9
As perineural cysts may become symptomatic due to inflammation, steroids may be useful in the conservative management as suggested by this case and Mitra et al.6 Since effective treatment of perineural cysts is controversial and associated with complications, steroids may be a good initial option. Though the exact role of steroids is not clear, it is unlikely that they have a nonspecific analgesic effect.6 However further studies are required to examine the efficacy of steroids in the treatment of perineural cysts.20
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
None.
None.

©2016 Dharmadhikari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.