MOJ
eISSN: 2374-6939


Case Report Volume 2 Issue 3
Past President European Wrist, Arthroscopy Society, UK
Correspondence: Tommy R Lindau, Consultant Hand Surgeon, Past President European Wrist, Arthroscopy Society (EWAS), The Pulvertaft Hand Centre, Kings Treatment Centre, Royal Derby Hospital, Uttoxeter Road, DE22 3NE, Derby, UK, Tel 00441332783389
Received: April 06, 2015 | Published: April 15, 2015
Citation: Lindau T, Oestreich K. Brodie’s Abscess 7 years after external fixation of a displaced distal radius fracture: a case report and review of the literature. MOJ Orthop Rheumatol. 2015;2(3):115-121. DOI: 10.15406/mojor.2015.02.00053
This case report and review of the literature present a rare long-term complication after a closed displaced distal radius fracture operated on with closed reduction and external fixation (EF). There were no early problems except a malunion without impairment. Seven years later the patient presented with a Brodie’s abscess; i.e. deep osteomyelitis at one of the previous EF pin sites. Brodie’s osteomyelitis often has a subtle and atypical presentation. X-rays may demonstrate an intraosseous bone lesion. Diagnosis is often made through MRI and/or nuclear bone scans. Standard treatment is operative excision of the lesion with curettage, insertion of antibiotic beads and appropriate antibiotics based upon curettage of the cyst and microbiological findings. We followed these principals and had an excellent outcome.
Keywords: Radius fractures, Complications, Osteomyelitis,; Brodie's abscess, Operative treatment
We are presenting a rare long-term complication of a Brodie’s abscess 7 years after external fixation of an initially uncomplicated treatment of a closed distal radius fracture. To our knowledge, and after a review of the literature, this is the first case published.
The patient, a 29-year-old laboratory technician, sustained a closed, dorsally displaced distal radius fracture in January 2005 (Figure 1), when he had jumped out of a window. In his past medical history he presented with depression. The right-sided radius fracture was manipulated in the local A&E (Figure 2). He was admitted for a closed reduction and stabilisation, which was done with an external fixation (EF) (Figure 3). The fracture was left with a slight dorsal tilt, which was accepted. At the same time carpal tunnel decompression was done. At the 2 week follow-up the x-ray showed no problems with the external fixation. Further weekly checks with the practice nurse were without any signs of pin track infections. The external fixator was removed after 6 weeks. Physiotherapy followed as per routine postop protocol. He was left with a malunion of the right radius, but no functional limitations (Figure 4). 2008, 3 years after the EF, he was back climbing and suffered a fall and landed on both hands. He presented with some bruising on the right, malunited hand and a minimal fracture of his left wrist, which was treated in a plaster (Figure 5). In March 2012, 7 years from his fractured right radius, he was referred to the Orthopaedic department due to some months of intermittent pain in his right mid forearm. The distal radius pain remained unclear and therefore an urgent x-ray was taken to exclude any bony pathology. A 10 x 6 mm lucency in the distal radius, at the site of the previous external fixator pin, was found (Figure 6). There was an abnormal sclerotic change around this area with some thick periosteal reaction and the appearances were highly suspicious for underlying chronic osteomyelitis. Blood tests were normal at the time. The intermittent pain was not increased by activity or loading and appeared in an unpredictable pattern. Clinical examination showed little, except the established deformity after malunion. Two months later the patient was reviewed after an MRI scan that showed low-grade osteomyelitis (Figure 7).
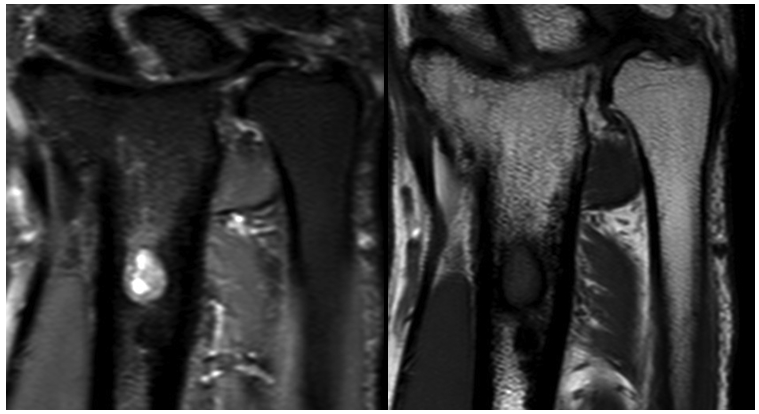
Figure 7 MRI scan showed a focal area measuring 6 x 8.6 x 11.7 mm area of iso-signal intensity lesion on T1 within the distal radius which was correspondent with high T2 signal intensity with areas of marrow oedema surrounding this lesion. There was abnormal periosteal reaction and sclerosis in the surrounding bone on both medial and lateral cortex of the distal radius in this region. The conclusion of MRI and x-ray were that the appearances were likely of a low-grade chronic osteomyelitis.
At the time it was agreed to treat this conservatively as the symptoms were only intermittent. In August 2012, 5 months from onset, the patient was re-referred due to increasing pain. At review, the pain had settled, but with two episodes of pain he was referred on to the local Hand department. He was reviewed a month later with full grip strength, no clinical signs of infection, but tenderness. A nuclear bone scan was done confirming osteomyelitis, so-called Brodie’s abscess (Figure 8). Repeated blood tests were still negative for infection. The patient was then operated on the Nov 2012 with curettage of the osteomyelitis in the radius and insertion of Gentamycin beads (Figure 9A–9C). Follow-ups 2 and 3 weeks postoperatively were uneventful. He was treated with oral Flucloxacillin for 8 weeks, after which there were no signs of inflammation or infection. Hence, the Gentamycin beads were removed and the previous defect was not bone grafted (Figure 10). The patient is still doing well 2 years after the Brodie’s abscess.
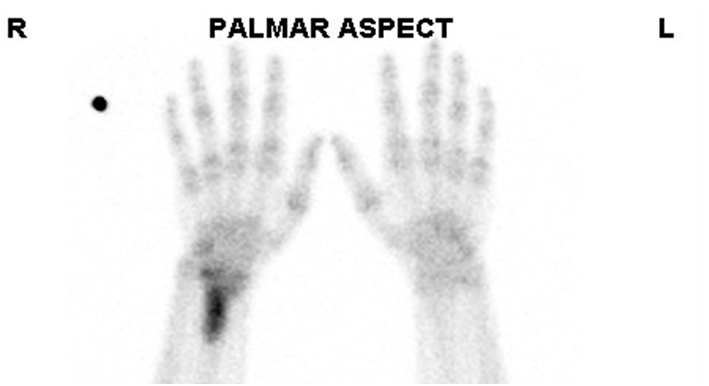
Figure 8 The NM Triple Phase Bone Scan noted (on perfusion and blood pool phase of imaging) hyperaemia in the region of the distal right radius.
Repeated blood tests were still negative for infection. The patient was then operated on the Nov 2012 with curettage of the osteomyelitis in the radius and insertion of Gentamycin beads (Figure 9A-9C). Follow-ups 2 and 3 weeks postoperatively were uneventful. He was treated with oral Flucloxacillin for 8 weeks, after which there were no signs of inflammation or infection. Hence, the Gentamycin beads were removed and the previous defect was not bone grafted (Figure 10). The patient is still doing well 2 years after the Brodie’s abscess.
We have performed a 10-year literature review regarding infection in general and particularly osteomyelitis, so-called Brodie’s abscess, after closed distal radius fracture (Table 1). The reported complication rate after distal radius fractures varies quite considerably. Some give a variation of 6-80% in the literature.1 Complications frequently encountered after operative treatment of distal radius fractures include tendon and nerve injuries, inadequate reduction with subsidence and collapse, inadequate placement of hardware, complex regional pain syndrome (CRPS), nerve compression syndromes and compartment syndrome.2 Infection is obviously more common in open distal radius fractures and quite frequently percutaneous K-wires cause superficial pin-track infections of less importance.3 These considerations affect choice of external or internal fixation.3
|
Author |
Title |
Journal |
Comment |
|
David J Petron, 2013 |
Distal radius fractures in adults |
Up To date |
Staphylococcus aureus osteomyelitis following hematoma block |
|
Shields DW, Elson DW, Marsh M, Gray AC |
Catastrophic osteomyelitis following percutaneous wire fixation of a distal radial fracture |
BMJ Case Rep. 2013 Jan 25;2013 |
osteomyelitis 4 weeks following surgery |
|
Tarallo L, Mugnai R, Zambianchi F, Adani R, Catani F. (level IV) |
Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. |
J Orthop Trauma. 2013 Mar 19. [Epub ahead of print] |
One patient had a deep post-operative infection treated with operative debridement. |
|
Subramanian P, Kantharuban S, Shilston S, Pearce OJ |
Complications of Kirschner-wire fixation in distal radius fractures. |
Techniques in Hand & Upper Extremity Surgery, September 2012, vol./is. 16/3(120-3), 1089-3393;1531-6572 (2012 Sep) |
The infection rate was 2%. These results illustrate a safe and clinically effective protocol for K-wire fixation in treating distal radius fractures. On the basis of this study, we do not advocate the use of prophylactic antibiotics, postulating that they do not affect infection rate |
|
Steinrucken J, Osterheld M C, Trampuz A, Borens O |
Malignancy transformation of chronic osteomyelitis: Description of 6 cases of Marjolin's ulcers |
European Journal of Orthopaedic Surgery and Traumatology, August 2012, vol./is. 22/6(501-505), 1633-8065;1432-1068 (August 2012) |
Case description: We present six patients with chronic osteomyelitis that developed well-differentiated squamous cell carcinoma… Five Marjolin's ulcers were located on the lower limb and one on the arm. |
|
Kurylo JC3 |
Open fractures of the distal radius: the effects of delayed debridement and immediate internal fixation on infection rates and the need for secondary procedures. |
Journal of Hand Surgery - American Volume, July 2011, vol./is. 36/7(1131-4), 0363-5023;1531-6564 (2011 Jul) |
We did not encounter infections for grade I and grade II open distal radius fractures, and infections do not appear to be related to either the time to debridement or the initial type of fracture fixation. Plating might be safe at the initial debridement, but temporary external fixation with a staged conversion to plating increases the risk of complications, which necessitates corrective secondary procedures.. |
|
Courvoisier A et al.12 |
Flare-up of previously quiescent chronic osteomyelitis 20 years after childhood skeletal traction: a report of two cases. |
Orthopaedics & traumatology, surgery & research, December 2011, vol./is. 97/8(886-9), 1877-0568 (2011 Dec) |
In this report, we describe two new cases of chronic osteomyelitis that manifested (many years) after childhood skeletal traction. After analysing these two cases, we proposed measures that can be implemented to avoid such complications, along with a simple, appropriate, reproducible treatment approach. |
|
Olasinde et al.11 |
Treatment of Brodie's abscess: excellent results from curettage, bone grafting and antibiotics |
Singapore Medical Journal, June 2011, vol./is. 52/6(436-9), 0037-5675;0037-5675 (2011 Jun) |
Brodie's abscess accounted for just 2 percent of all patients with osteomyelitis…. and the radius …(was affected) in 10 percent… Patients with Brodie's abscess respond well to surgical curettage of the abscess, cancellous bone grafting and antibiotic therapy. |
|
Das AK et al.4 |
Percutaneous pinning for non-comminuted extra-articular fractures of distal radius. |
Indian J Orthop. 2011 Sep;45(5):422-6. doi: 10.4103/0019-5413.83949. |
This study's aim was to examine the functional outcome of percutaneous K-wiring of these extra-articular distal radius fractures with immobilization in neutral position of the wrist.pin tract infection (n=2) (our of 32 patients). |
|
Lakshmanan P et al.5 |
Infection rate of percutaneous Kirschner wire fixation for distal radius fractures.
|
Journal of Orthopaedic Surgery, April 2010, vol./is. 18/1(85-6), 1022-5536;1022-5536 (2010 Apr) |
The infection rate after percutaneous Kirschner wire fixation is unacceptable. Kirschner wires should be buried under the skin to decrease the infection rate. |
|
Lin TY et al.13 |
Pathological fracture of the right distal radius caused by Enterobacter aerogenes osteomyelitis in an adult. |
American Journal of the Medical Sciences, May 2010, vol./is. 339/5(493-4), 0002-9629;1538-2990 (2010 May) |
osteomyelitis, Lin (2010) comments that “Acute bacterial osteomyelitis that results in pathological fractures in the extremities is rare in adults". The article reports “the first case of enterobacter aerogenes osteomyelitis of the right distal radius, complicated with a pathological fracture”. |
|
Ting JW et al.15 |
Free deep circumflex iliac artery vascularised bone flap for reconstruction of the distal radius |
Microsurgery, 2010, vol./is. 30/2(163-7), 0738-1085;1098-2752 (2010) |
Complicated cases such as these are often limited in their management options. We present a complex case of distal radius fracture and bone loss in which initial therapy with nonvascularized bone graft failed, and osteomyelitis was a further complicating factor. With the aid of preoperative planning with computed tomographic angiography (CTA), a deep circumflex iliac artery (DCIA) bone flap was able to be assessed as a reconstructive option. |
|
Taylor SM et al.17 |
Wound botulism complicating internal fixation of a complex radial fracture |
Journal of Clinical Microbiology, February 2010, vol./is. 48/2(650-653), 0095-1137 (February 2010) |
Botulism developed in a patient following surgical repair of an open radial fracture. Symptoms resolved after treatment with antitoxin and antibiotics, and hardware excision was deferred. Subsequent osteomyelitis necessitated hardware exchange, and wound cultures grew Clostridium argentinense. |
|
Desai A et al.6 |
Discharging pin sites following K-wire fixation of distal radial fractures |
Acta Orthopaedica Belgica, June 2009, vol./is. 75/3(310-5), 0001-6462;0001-6462 (2009 Jun) |
We conclude that pin site discharge, whether sterile or infected, is in general not an indication for early wire removal. |
|
Handoll HH et al.9 |
External fixation versus conservative treatment for distal radial fractures in adults. |
Handoll HHG, Huntley JS, Madhok R. External fixation versus conservative treatment for distal radial fractures in adults. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD006194. DOI: 10.1002/14651858.CD006194. pub2. |
Fifteen heterogeneous trials, involving 1022 adults with dorsally displaced and potentially or evidently unstable distal radial fractures, were included. While all trials compared external fixation versus plaster cast immobilisation, …We conclude that pin site discharge, whether sterile or infected, is in general not an indication for early wire removal. |
|
Saint-Cyr M16 |
Double-barrel free fibula flap for treatment of infected nonunion of both forearm bones.
|
Journal of Reconstructive Microsurgery, November 2008, vol./is. 24/8(583-7), 0743-684X (2008 Nov) |
chronically infected nonunion of the radius and ulna treated with a double-barrel free fibula flap |
|
Gehrmann SV et al.10 |
Distal radius fracture management in elderly patients: a literature review.
|
J Hand Surg Am. 2008 Mar;33(3):421-9. doi: 10.1016/j.jhsa.2007.12.016. |
Volar plating with fixed-angle screws may be particularly suitable for elderly patients who may take longer to heal a fracture, be more susceptible to pin-track infection, |
|
Raskin KB et al.7 |
Distal Radius Fractures: External Fixation and Supplemental K-Wires |
Atlas of Hand Clinics, September 2006, vol./is. 11/2(187-196), 1082-3131 (September 2006) |
The frequently reported pin-related complications can be reduced significantly by several key steps to surgical application. Open bicortical half pin placement avoids soft tissue, tendon, and nerve iatrogenic injuries, and minimizes the risk of unicortical pin insertion that can result in metacarpal or radial shaft fractures or subsequent loosening or infection. Pin inflammation and superficial infection often can be resolved by oral antibiotics, physician pin care, and gauze dressing |
|
Basu A, Bhalaik V, Stanislas M, Harvey IA.
|
Osteomyelitis following a haematoma block. |
Injury. 2003 Jan;34(1):79-82. |
Abstract: No abstract available |
Table 1 Literature review last 10 yrs on distal radius fractures and osteomyelitis
Furthermore, infection is more commonly found after K-wire treatment than compared to external fixation.4–8 Risk factors for pin track infection has been discussed. Type of pin insertion and patient age was highlighted: The Cochrane report from 20079 compares conservative versus external fixation of distal radius fractures in adults. Here external fixation was associated with a high number of complications, such as pin-track infection, but many of these were minor and the type of pin insertion was challenged as a cause of infection. In patients treated with external fixation, the main risk factor for pin track infection is patient age related.10
Closed, as opposed to open, distal radius fractures only rarely have infection as a complication post surgery. The literature is scares. Osteomyelitis, so-called Brodie’s abscess, is an even rarer complication after closed distal radial fracture and external fixation; in fact, we believe this is the first publication on that matter. Brodie’s osteomyelitis is generally a rather uncommon variant of subacute osteomyelitis. There is only limited literature available regarding long-term Brodie’s osteomyelitis after external fixation in general; with about 2 % Brodie’s abscess in all osteomyelitis.11 In a cohort of 20 patients with Brodie’s abscess, only 10 % affected the radius. The majority is found in the lower limb, which is supported in a series of chronic osteomyelitis 20 yrs after childhood skeletal traction therapy within management of lower limb fractures in children.12 Some rare complications without relation to trauma has been seen in the distal radius in elderly diabetic patients are osteomyelitis and pathological fractures13 and in the ulna with growth of Salmonella typhi.14
Osteomyelitis as a rare complication of complex distal radius fractures has been seen if the initial treatment included bone grafting.15,16 An extremely rare case of osteomyelitis after ORIF of an open radial fracture and wound botulism has been described,17 but not after external fixation. We present a rare case of Brodie’s osteomyelitis 8 years after treatment with external fixation for a closed displaced distal radius fracture. The complication is hard to understand as there was no sign of initial infection at time of treatment nor were there any contributing complicating factors, such as old age, diabetes etc.
Brodie’s osteomyelitis often has a subtle and atypical presentation. It should be kept in mind as a differential diagnosis even in late complications after trauma many years ago also in cases with an initially uncomplicated distal radius fracture treatment. In addition to normal x-rays, which may demonstrate intraosseous bone lesion; MRI scan and/or nuclear bone scan is often needed to establish correct diagnosis. Blood tests can be unspecific and misleading as in our case. Microbiology should be obtained routinely intra-operatively to provide adequate antibiotic cover. Once diagnosed, standard treatment for Brodie’s abscess is operative excision of the lesion with curettage and insertion of antibiotic beads4,15 demonstrated in our case.
None.
None.

©2015 Lindau, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.