MOJ
eISSN: 2374-6939


Case Report Volume 16 Issue 2
Department of Orthopaedic Surgery and Sports Medicine, University of Kentucky College of Medicine, Lexington, USA
Correspondence: Srinath Kamineni MD, Department of Orthopaedic Surgery and Sports Medicine, Kentucky Clinic, Department of Orthopaedic Surgery, 740 S. Limestone, Suite K401, Lexington, KY 40536-0284, Tel +1 (859) 806 7703, Fax (859) 323-241
Received: March 05, 2024 | Published: March 25, 2024
Citation: Ulrich G, Kamineni S. Brachial plexus compression by a long head of the biceps tendon ganglion in the setting of anatomic total shoulder arthroplasty: a case report. MOJ Orthop Rheumatol. 2024;16(2):46-48. DOI: 10.15406/mojor.2024.16.00662
Case: A 59-year-old female with a history of chronic left shoulder pain presented with a chief complaint of a constant, “burning” sensation in the left chest and shoulder region. On MRI, a large cystic structure originating from the biceps tendon was noted. Surgical exploration confirmed a ganglion cyst to be encroaching upon and compressing the brachial plexus and axillary artery against the chest wall. 12 months after resection of the cyst, the patient remains pain-free.
Conclusion: Diffuse arm pain can stem from a variety of different pathologies. In this case, timely diagnosis of a unique pathology contributed to resolution of symptoms.
Level of Evidence: Level V.
Keywords: brachial plexus, ganglion cyst, osteoarthritis, total shoulder arthroplasty, case report
Ganglion cysts occurring around the shoulder are mostly in the spinoglenoid and suprascapular notches, and can cause compressive suprascapular nerve palsy.1 Those that are symptomatic and recalcitrant to conservative management can be treated with cyst decompression and resection with favorable long-term results.2 Additional locations include paralabral cysts, most of which are reported along the posterior, superior and anterior aspects of the glenohumeral joint with fewer reported inferiorl7.3 These are commonly associated with biceps tendinopathy, osteoarthritis of the glenohumeral joint and trauma and are usually treated with decompression and labral repair.4 We are unaware of a ganglion cyst arising from the long head of the biceps tendon large enough to compress the brachial plexus. The patient provided written informed consent for the publication of the case.
A 59-year-old female presented with a history of chronic left shoulder pain and stiffness. In addition to classic osteoarthritic symptoms, she reported an atypical pain described as a constant, deep-seated, “burning” sensation in the chest and shoulder region that ranged in severity from 6/10 at its best to 9/10 at its worst. This pain combined with debilitating weakness in the upper back and shoulder muscles had progressed to interfere with activities of daily living. This burning sensation in the chest and shoulder was not reproducible on physical exam, but there was palpatory tenderness inferior to the acromioclavicular joint, long head of biceps and anterior supraspinatus consistent with shoulder osteoarthritis and rotator cuff damage. During both passive and active range of motion exams, the patient was limited to 30 degrees of shoulder forward flexion, 30 degrees shoulder abduction and 0 degrees of both internal and external rotation, with palpable and audible crepitus. Pain was noted with all provocative maneuvers. She was neurologically intact in the axillary, radial, median, and ulnar nerve territories, with normal sensation to light touch, proprioception and two-point discrimination. Diffuse muscle atrophy was noted throughout her left shoulder on physical exam. She had equal radial and brachial pulses when compared to the contralateral asymptomatic arm. X-rays of the left shoulder revealed advanced, end-stage glenohumeral osteoarthritis with significant circumferential osteophytosis (Figure 1A &1B). As it was determined unlikely for these symptoms to be caused by isolated shoulder osteoarthritis and to help guide further management, MRI scans were ordered which demonstrated some thinning of the supraspinatus tendon, with Goutallier Grade 1 fat atrophy, and a degenerative long head biceps tendon. Additionally, a large cystic structure originating from the biceps tendon was noted (Figure 2).
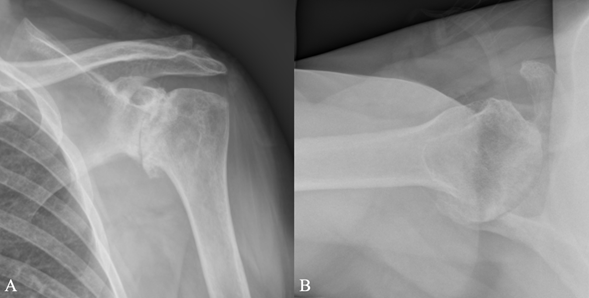
Figure 1 Preoperative plain radiographs of left shoulder in both A) anteroposterior and B) axillary views.
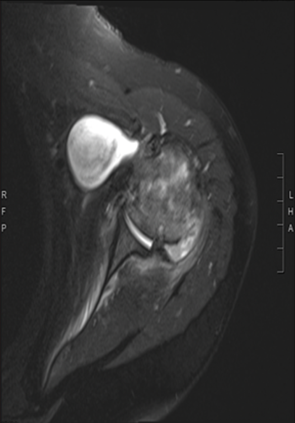
Figure 2 Preoperative MRI of left shoulder demonstrating a large cystic structure originating from the biceps tendon.
Preoperative discussion included the potential further investigations (arteriogram and nerve conduction studies) and various treatment options. A specific detailed discussion about nerve conduction studies, noting false negative results in early stages of compressive pathology reported in the literature was conducted. Since no objective clinically evident neurovascular signs could be elicited and given the costs associated and delays associated with nerve conduction studies, the patient opted for a left anatomical total shoulder arthroplasty with rotator cuff repair and augmentation along with exploration and possible evacuation of the cystic structure without any further investigations.
A standard deltopectoral approach was utilized, and the procedure commenced with partial tenotomies of the pectoralis major and conjoint tendon. Attention was then turned to the subscapularis, which was noted to be difficult to identify due to extensive scarring. While meticulously dissecting this scar tissue with a Cobb, an abnormal outpouching structure was noted in the subpectoral region (Figure 3A). Upon further dissection, this was noted to be the preoperatively diagnosed cystic structure that was circumferentially followed to the chest wall. At this point in this procedure, the cords to the brachial plexus were not palpable in their usual location and the axillary artery was not visible. It became apparent that these neurovascular structures were being inferiorly and medially compressed by the cystic structure. Given the close proximity of this location to the brachial plexus cords and axillary artery, it was decided to incise and carefully remove the contents of the cyst and the cyst wall itself before proceeding with further dissection (Figure 3B). After the cyst was incised and its contents evacuated, the axillary artery and cords of the brachial plexus became more visible. The cystic structure was then circumferentially dissected free of attachments along fascial planes and was excised and sent for cytology and pathology (Figure 3C). A stemless total shoulder arthroplasty procedure was carried out, the attenuated rotator cuff was repaired with collagen patch augmentation, and the biceps was tenodesed (Figure 4).
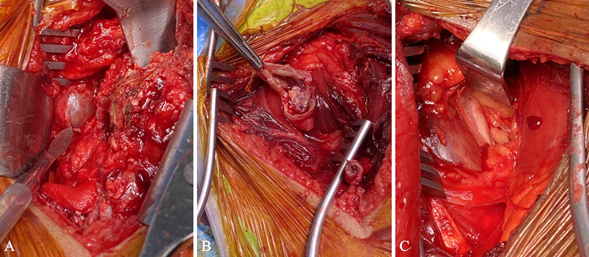
Figure 3 A) Intra-operative findings of ganglion cyst prior to resection, B) gelatinous material inside cyst, and C) the result after decompression was performed.
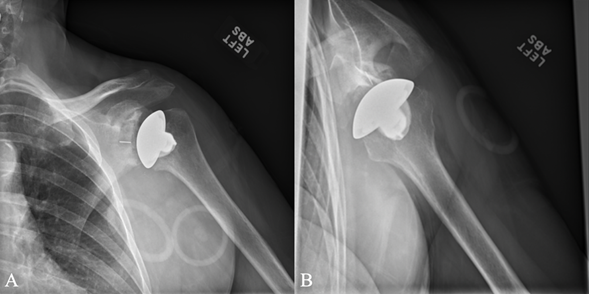
Figure 4 Postoperative plain radiographs of left shoulder demonstrating appropriately positioned stemless implant in both A) anteroposterior and B) axillary views.
At the 2 week postoperative appointment, the patient had complete resolution of the burning sensation in the chest and shoulder pain that she initially reported in addition to resolution of her osteoarthritic symptoms. As of 12 months post-surgery, the patient remains pain-free, with no dysesthesias related to the brachial plexus, and good shoulder function.
Unexplained arm and chest pain in a middle-aged female can be particularly challenging to diagnose given the wide range of potential causes. In the case of this patient, her past medical history was unrevealing and her physical exam findings were non-contributory. Furthermore, her vague, non-specific symptoms could be explained by a variety of conditions. For example, one known cause of such pain includes primary tumors of the brachial plexus, the most common of which are peripheral nerve sheath tumors.5 Other less common, but nonetheless well-described, causes of brachial plexus neuropathy include Neuralgic amyotrophy (Parsonage Turner Syndrome), extra neural brachial plexus hemangiomas, arterial thoracic outlet syndrome, and even Varicella-Zoster virus dissemination to the brachial plexus.6
To differentiate among these and various other possibilities, further diagnostic testing such as advanced imaging and electrophysiological studies may be performed. Beyond plain radiography, ultrasound scanning is often performed due to its low cost, but has a relatively low sensitivity for brachial plexopathies and false negative rates up to 35%.7 Hence, in this case, it was decided to proceed with an MRI scan.
MRI scans provide good visualization of soft tissue structures in the shoulder girdle, and are particularly useful for identifying rotator cuff pathology and ganglion cysts. They are less effective at diagnosing adhesive capsulitis, glenohumeral or acromioclavicular arthritis, brachial plexopathy and cervical degenerative disease.8 The MRI demonstrated a large cystic structure, with a clear communication to the long head biceps tendon sheath, a source of brachial plexus irritation. After a potential source of the pain was identified, possible vascular causes, such as thoracic outlet syndrome, were considered, but was precluded by the patient due to the invasive nature and complications associated with angiograms.9 Since no vascular malformations were visible on MRI, cyst resection, at the time of anatomic total shoulder arthroplasty with rotator cuff repair and augmentation, was performed. This procedure proceeded as planned with an uneventful post-operative course, reaffirming that this was the appropriate management for this presentation.
While ganglion cysts are most commonly found in the wrist, foot or knee, in theory they can arise at any articular surface as a consequence of continuous micro-trauma to mesenchymal cells at the synovial capsular junction.10 Often, both physical examination and X-ray findings in these patients are non-specific. It is therefore important to always consider ganglion cysts as a source of pain or functional loss in patients with conditions that affect the joint space, such as biceps tendinopathy. As is evidenced by this patient, timely diagnosis, exclusion of other differential diagnoses, followed by cystic resection can help lead to resolution of symptoms.
Diffuse arm pain can stem from a variety of different pathologies making diagnosing such presentations challenging. While a thorough clinical history and physical exam, including specific provocative maneuvers, is a responsible starting point, diagnosis often requires further investigation including X-ray, ultrasound, and MRI. In this case, the constant, diffuse burning chest and shoulder pain was thought to be caused by brachial plexus compression by a ganglion cyst, originating from the long head of the biceps tendon. Diagnosis was supported with an MRI scan and symptoms subsided following resection of the cyst combined with an anatomic total shoulder arthroplasty, with complete resolution of symptoms.
None.
No potential conflict of interest relevant to this article was reported for all authors. Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.

©2024 Ulrich, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.