MOJ
eISSN: 2374-6939


Research Article Volume 2 Issue 4
Orland Park Orthopedics, USA
Correspondence: Blair A Rhode, Orland Park Orthopedics, 16450 S 104th AV, Orland Park, Illinois 60467, USA, Tel 708-364-8441, Fax 708-364-8443
Received: February 11, 2015 | Published: April 29, 2015
Citation: Rhode BA. Biomechanical comparison of single- double- and novel triple- row rotator cuff repairs in a porcine model using generic anchors. MOJ Orthop Rheumatol. 2015;2(4):139-143. DOI: 10.15406/mojor.2015.02.00058
Comparison of a novel triple-row (NTR) rotator cuff repair (RCR) was made to single row (SR) and double row (DR) repairs as measured by gap formation, Ultimate Failure Load (UFL), and mode of failure. Porcine humeri were divided into three groups of forty and the infraspinatus tendons were completely released and then repaired using generic (PEEK) anchors. Biomechanical testing of RCRs consisted of 3500 cycles of a load varied from 10 to 180 Newtons (N). Gap size at all cycle counts was significantly larger for SR and DR than NTR RCRs. 84% of NTR repairs completed the 3500 cycle test versus 66% of DR and 61% of SR repairs. The tendon pulled from the sutures 60%, 49% and 33% of the time for SR, DR and NTR RCRs respectively. UFLs were 464 N for the NTR repairs, 394 N for DR and 414 N for SR repairs. In summary, NTR repairs resulted in smaller gap formation, higher UFLs, and fewer instances of tendons tearing at the sutures than SR or DR repairs. Results of NTR repairs demonstrate that the tendon footprint is securely restored with small gap formation for the range of forces that a shoulder will be subjected to in normal use.
Keywords: Rotator cuff, Rotator Cuff repair, Shoulder, Single row, Double row, Triple row, Porcine, Ultimate failure load, Biomechanical
RC,: Rotator Cuff; RCR,: Rotator Cuff Repair; SR, Single Row; DR, Double Row; NTR, Novel Triple Row; UFL, Ultimate Failure Load; N, Newtons; PEEK, Polyetheretherketone; df, Degrees of Freedom; RōG, Rhode Orthopedic Group
Rotator cuff disease is one of the most common shoulder disorders. When surgical intervention is indicated arthroscopic rotator cuff repair (RCR) has become the method of choice. The goal of the repair is to obtain tendon-to-bone fixation with a minimal gap that is maintained while healing proceeds. The optimal RCR method remains controversial.1 Biomechanical studies have been performed on both animal models and human cadaver shoulders to determine the relative merits of rotator cuff repair techniques.2–7 Comparison of double-row (DR) to single-row (SR) suture-anchor rotator cuff repair have not always resulted in clear advantages of one method over the other. Outcome differences remain in spite of several studies indicate that DR repairs result in better footplate restoration and smaller gap size than SR repairs.8 However, when tear size is stratified there is a significant difference between SR and DR repairs.9 Clinical studies of DR versus SR repairs often conclude that patient outcomes as measured by gap development do not differ between the two techniques.8 Studies often conclude that further research is required to determine whether better footplate restoration in DR repairs results in superior healing as observed by imaging the rotator cuff.
RCR biomechanical studies permit manipulations that cannot be duplicated in patients. Recent studies have employed an increasing number of anchors and sutures in a variety of configurations.10,11 The goal of each study was to increase the pressure over the entire footplate of the torn tendon. A triple row repair and a diamondback (DBK) repair employed knotless anchors at the edge of the tendon to allow sutures to compress the tendon edge to the bone.12–14 Pressure measurements in the tendon footplate indicated DBK repair was the best repair of four repair methods.
Due to the ongoing controversy as to the best repair method and concerns over total cost, a novel triple-row (NTR) repair is compared to DR and SR repairs of porcine infraspinatus tendon tears. NTR repair employs two levels of mattress sutures and two knotless anchors beyond the tendon edge to compress the tendon to its footplate. This approach is reminiscent of the bridging self-reinforcing double-row RC repair.15 Repair performance is determined by Ultimate Failure Loads (UFLs), gap size development, and mode of tendon failure. Clinically RCR involves cost, time, and ease of repair, all of which are minimal in a simple-single row repair. A simple repair doesn’t strangulate the tendon and allows little separation from the bone in the absence of significant tension.
Hypothesis: H0: there is no difference between a triple row versus a single or double row RCR as measured by gap size, Ultimate Failure Load (UFL), or mode of tendon failure.
120 pig shoulders were obtained from a wholesale meat market and divided into three groups of 40. All tissue was removed from the humerus except the infraspinatus tendon. The preparation was frozen until used. Porcine infraspinatus tendons are approximately 15 mm in width and 7 mm thick in the footplate region. A double layer of sterile wrap (KimgardÒ) was sewed to the free end of the tendon using a continuous stitch (Ethicon 0 silk) to prevent the upper grip of the test instrument from compressing the tendon to the point that it results in an early failure at the site of the grip. After the preparation was warmed to room temperature the tendon was released from the humerus with a #20 scalpel blade. NTR repair employs two generic 5.5 mm polyetheretherketone (PEEK) anchors (RōG, Orland Park, IL) loaded with two ultrahigh molecular weight polyethylene (UHMWPE) #2 sutures inserted at a 75 -90° angle to the bone.16 The steps in an NTR repair technique are illustrated in (Figures 1–6).
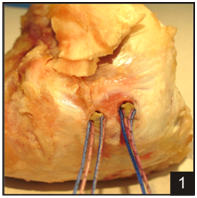
Figure 1 Step one of the triple row repair begins with inserting two double loaded anchors 1 cm apart in the tendon footplate.

Figure 3 Horizontal mattress passes are made through the anterior and posterior margins of the rotator cuff tear.
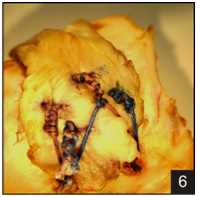
Figure 6 Finally, the sutures from the medial rows are passed through the knotless anchors positioned lateral to the footplate and tensioned to hold down the lateral edge of the tendon.
DR repairs consist of two mattress sutures medially placed and two knotless anchors placed laterally (Figure 7). Testing was identical to that of the NTR repair. SR repairs were constructed by placing two 5.5 mm double-loaded anchors in the tendon footprint separated by 1 cm (Figure 8). Testing was identical to that of the NTR repair.
The humerus was held at a 45° angle in a special-bilt vise with the tendon at its normal position and angle when the load is applied. Iron shafts are inserted through two holes drilled into the humerus and the vise to secure the humerus (Figure 9). This prevented the bone from slipping from the vise due to the use of UFLs (> 500 N). The free end of the wrapped tendon was placed in the upper grip of the test instrument. Tests and measurements are performed with a Test Resources 225LB Actuator (Shakopee, MN). A 10 N load is initially applied. The test force is then cycled 3500 times from 10 to 180 N at a rate of 635 mm/min or until tendon failure. These parameters were chosen based on several biomechanical studies of human rotator cuff.3,17-19 Position and load were sampled at 100/s for every 20th cycle and later analysed using MATLAB (Ver 7.1)®. The initial 1 min of the test session was video recorded for measurement of gap formation using MaxTRAQ software (Ver2.2.2.5, Innovision-systems.com). Photographs were taken at 100, 500, 1000, and 2000 cycles for gap measurement. Video recording at 30 frames/s of the single pull to failure test (UFL) was used to determine the mode of repair failure (STCamSWare x 86 ver1.0.0.4, www.sentechamerica.com). 10 intact tendons were subjected to the test sequence to ensure that this preparation was appropriate for the study. All survived the displacement-load cyclic test.

Figure 7 The double row repair employed two 5.5 mm double-loaded PEEK anchors centered in the tendon footprint separated by 1 cm with sutures tied in a mattress configuration. Two 5.5 mm knotless anchors are positioned laterally. Sutures from the medial row are passed through the knotless anchors and tensioned to hold down the lateral edge of the tendon.
Cyclic test
The majority of repaired tendons survived the 3500 cycle test regardless repair type, this consisted of 84% of NTR and 61% of DR, and 64 % of SR repairs. Gap size, a measure of repair integrity, is significantly larger for SR and DR compared to NTR (Figure 10). Gap size beyond 2000 cycles was nearly constant. NTR gap size is smaller than DR and SR gaps initially and over all later cycles of the test. With a commonly used criterion of a 5 mm gap constituting RCR failure, 29 of 39 DR and 30 of 40 SR repairs failed compared to 7 of 37 NTR repairs. With a criterion of a 9 mm gap constituting repair failure then 14 DR and 16 SR repairs failed compared to zero NTR repairs. NTR repair gap size remained less than 3.1mm in 14 instances throughout the 3500 test cycles. Because SR and DR results are very similar, NTR repair is only compared to the DR result. There is little overlap in gap size between techniques. An unpaired t-test for two groups with both unequal variances and counts was used to determine the significance of the gap differences.20 At all three cycle counts the two-tailed p- value was less than 0.0001. The t-value and degrees of freedom (t, df) for the three cycle counts were: at 100 cycles (6.9,74), at 1000 cycles (8.2, 2) and at 2000 cycles (8.3,53). All (t-values, dfs) indicate highly significant differences resulting in rejection of the H0 hypothesis based on gap size indicating an alternative hypothesis that NTR repair is a more robust technique. The mode of tendon failure was either intratendinous or intrasuture. 60% of SR and 64 % of DR repairs failed at the sutures versus 33% of the NTR repairs. When an NTR RCR failed, the tendon tore above the sutures at twice the rate of the sutures pulling through the tendon.
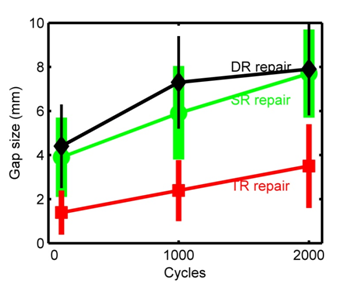
Figure 10 Comparison of mean gap formation for the three repair techniques at 100, 1000 and 2000 cycles. The vertical bars correspond to mean gap size in mm ± standard deviation (SD).
Ultimate failure load
There was a significant difference between the mean UFLs for NTR versus SR repairs, 465 N versus 410 N (Table 1). The H0 hypothesis was checked with a t-test that yielded t=2.76 with 44 degrees of freedom. The p-value for a one-sided test is 0.0042 and a 2 sided test of 0.0084, both highly significant, resulting in the rejection of the H0 hypothesis. Based on UFL, NTR RCR is significantly better than either SR or DR repairs.
|
UFL |
NTR |
SR |
DR |
|
Mean(N) |
465 |
414 |
394.5 |
|
SD(N) |
88.8 |
77.1 |
65.4 |
|
Count |
32 |
27 |
27 |
|
Min(N) |
295 |
280 |
268 |
|
Max(N) |
660 |
550 |
515 |
Table 1 UFLs statistics for the three repair techniques. Tendon failure during cyclic testing prevented UFL determination resulting in counts less than 40, the group count for each technique
UFL, Ultimate Failure Load; results for each repair technique; Mean UFL, SD, Standard Deviation, Minimum, and Maximum are given in Newtons (N).
The principal result of this study is that NTR RCR results in a smaller gap formation and higher UFLs than either SR or DR RCRs. This result was obtained while using higher loads (180 N) and significantly larger number of cycles (3500) than most previous studies.21,22 Based on this rigorous test environment it appears that after NTR repair the tendon will remain appropriately positioned at the footplate which is essential for healing after RCR.
There remains disagreement as what is the best RCR method. In an earlier study, SR repairs with a modified suture configuration were compared to four different DR repairs in pig shoulders with a sample size of 8.21 Repairs were first tested with a 10 to 20 N force range for 50 cycles with the tendon at a 90° angle to the humeral shaft. Maximum force was then increased in 20 N steps until a 100 N force was obtained. While DR repairs resulted in greater footprint coverage than SR, the principal finding was that SR repairs with modified suture configurations yielded comparable results to DR configurations. Similar results were obtained in this study with comparable gap sizes for SR and DR repairs (Figure 10) with the caveat is that SR repairs were more likely to fail based on excessive gap size formation.
A single row repair in cadavers utilized three triple loaded anchors to create a row of 6 mattress sutures and an additional two large mattress sutures close to the tendon edge.22 Cyclic loading results showed that this repair exhibited smaller displacements than a DR repair with significant differences between the anterior/posterior locations. In contrast, DR repairs were reported to be significantly better than SR repairs.23 The diamondback double row repair technique (DBK) resulted in a large “pressurized containment grid” in cadaver shoulders and used two double loaded anchors medially and three anchors laterally.14 DBK repair is similar to NTR repair in that both utilize lateral mattress sutures to maintain the lateral edge of the tendon in contact with the footplate. NTR repair has a double row of mattress stitches (total of four) and used one less anchor than DBK repair.
Anchor pullout and suture breakage have been studied extensively because of their importance in RCRs.24 Certain anchor design features may result in more eyelet and suture failures. For example, Barber demonstrated that lateral anchors that were designed to accommodate three sutures had significant eyelet failures and were more prone to suture slippage.25 A suture-tape, rip-stop DR configuration covered more of the footprint than a SR triple loaded anchor.26 No SR or DR repair tested showed 5 mm of displacement after the first 100 cycles. The most common catastrophic failure was the suture tearing out of the tendon. In this study, if a 5 mm gap is the criteria for repair failure then both SR and DR repairs failed as the number of cycles increased. In contrast, gap formation in NTR repairs never reached the 5 mm failure criteria.
The most common NTR repair failure was the tendon fatiguing followed by tearing above the sutures. Anchors did not pullout nor did sutures break or wear out at the eyelets. This indicates that generic PEEK anchors and UHMWPE sutures will not be limiting elements of RCRs. This reinforces the general conclusion that the size of the tear and condition of the tendon and bone are the limiting aspects of achieving a repaired rotator cuff. Patient age is a major factor affecting bone density resulting in longer healing times and contributing to the higher rate of RC repair failure.27 Tendon cellularity and vascularity are markedly diminished at age 70, bone quality is also inferior, resulting from osteoporosis of the greater tuberosity, cystic degeneration, and irregularity of cortical margins, all of which may significantly complicate anchor fixation.28 Hardware required for RCR methods can vary considerably for medium to large tendon tares. One method used 3 anchors and 9 sutures in a SR repair with 8 mattress sutures while 6 anchors and 6 sutures were used for a DR repair with 4 mattress sutures.22 In comparison, NTR repair used 4 anchors and 4 sutures saving significant costs. When the humerus real estate in a RCR is limited a single anchor would be used laterally. Less hardware translates into shorter surgery time.
The principal result of this study is that NTR RCR results in a smaller gap formation and higher UFLs than either SR or DR RCRs. Neither generic anchors nor UHMWPE sutures failed in the 120 RCRs performed in this study, i.e. no anchors pulled out or eyelets broke. For NTR RCRs tendons tore medial to the sutures and only occasionally at the sutures.
This is a biomechanical study and as such its immediate application to the clinical experience is limited. This is a zero time measure and as such provides no information regarding tendon healing. Porcine humerus is likely harder than human humerus bone and that may explain why there were no anchor pullouts in these tests whereas in cadaver studies or patients the humerus may be compromised increasing the likelihood of anchor pullout.
NTR rotator cuff repairs exhibited smaller gap development and higher UFLs than SR or DR repairs while providing compression of the tendon to the footplate. No additional time, effort, or materials are required relative to DR repairs. Generic anchor use did not degrade repairs while reducing costs. Whether these properties will result in improved outcomes in humans will have to be demonstrated in a clinical trial.

©2015 Rhode. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.