MOJ
eISSN: 2374-6939


Case Report Volume 1 Issue 2
1Department of Orthopedic Surgery, AVE Orthopaedic Clinics, Netherlands
2Department of Neurology, Rivierenland Hospital, Netherlands
Correspondence: Ibo van der Haven, Department of Orthopedic Surgery, AVE Orthopaedic Clinics, Netherlands, Tel 310356223260, Fax 310355152557
Received: July 22, 2014 | Published: October 17, 2014
Citation: Wijers D, Piepers M, Hoogendoorn-Stroband TA, et al. Bilateral posterior fracture dislocation of the shoulder following an epileptic seizure. MOJ Orthop Rheumatol. 2014;1(2):32-33. DOI: 10.15406/mojor.2014.01.00010
We report a rare case of a 39-year-old man with bilateral posterior dislocated shoulder joints with comminuted fractures of the humeral heads after an epileptic seizure. Posterior shoulder dislocations prove to be a diagnostic challenge and in this case were missed at initial presentation. After a failed attempt of osteosynthesis and removal of material, he received a hemi-prosthesis in separate stages on both sides.
Keywords: Bilateral, Posterior, Fracture, Dislocation, Shoulder, Seizure
Numerous orthopaedic injuries can follow a seizure. Posterior fracture dislocation of the glenohumeral joint is a rare injury. It is one of the least common injuries to the shoulder.1 Diagnosis is difficult and often missed because of its rarity.2 In 50-80% of all cases the dislocation is only recognized after initial assessment.2,3 Bilateral posterior dislocation of the shoulders is almost pathognomonic for seizure, trauma or electric shock. By the force of the trauma the dislocated humerus can furthermore fracture. This can result in such an extensive destruction of the shoulder joints that it necessitates replacement with shoulder prostheses. Only few cases were described in literature.1 In this paper we present a 39 years old male who was brought into the emergency department after having a seizure. Posterior fracture dislocations of both shoulders were missed initially, resulting in a delay in diagnosis and treatment.
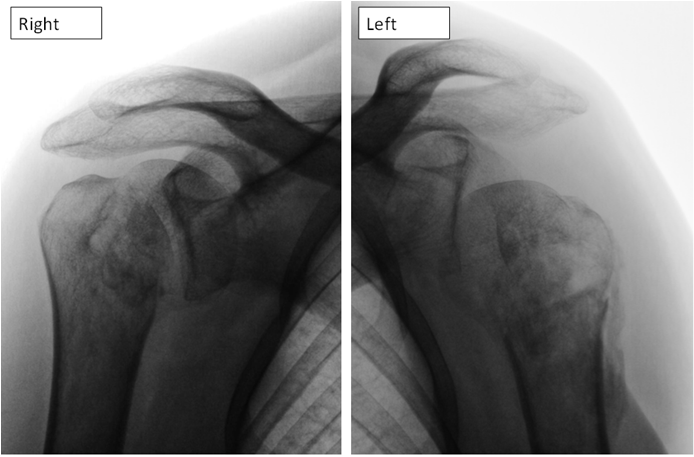
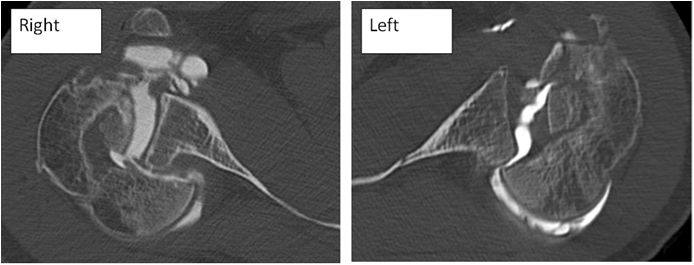
A 39 years old male was presented to the emergency room after experiencing a grand mal epileptic seizure. Initial examination revealed a bitten tongue, urinary incontinence, confused behavior and pain in both shoulders. The patient’s medical history was unremarkable for a seizure disorder. He was admitted at the neurology ward. The second day of admission it became clear during physiotherapy that the patient had a painful, limited range of motion in both shoulders. Antero-posterior radiographs were made and these showed bilateral posterior dislocated shoulder joints with comminuted fractures of the humeral heads (Figure 1). A general surgeon performed an open reduction and internal fixation of the left shoulder. Post-operative radiographs, 48 hrs. After surgery, showed dislocation of the osteosynthesis. Three weeks after initial presentation the hardware was removed and a conservative treatment was applied on both shoulders. After discharge, the patient consulted an orthopaedic surgeon on his own initiative in a specialized orthopaedic centre for a second opinion. A CT arthrography of the shoulders was performed showing extensive comminution and still present posterior dislocation of the fracture parts (Figure 2).
Over four months after the seizure, a cemented shoulder hemi-prosthesis was implanted on the left side. The right shoulder was treated in a similar fashion 16 months after the initial presentation. Post-operative treatment consisted of a sling during 6 weeks and physiotherapy. No postoperative complications were seen. The patient experienced multiple seizures after his first episode but no cause could ever be found. At the moment he is treated with anti-epileptic medication. Follow-up after two years showed a limited range of motion in both shoulders: 70 degrees abduction, 10 degrees exorotation in the right and 0 degrees in the left, 30 degrees of endorotation and finally 70 degrees of posterior flexion. The patient is able to perform daily activities, but due to his limitations he is no longer capable of working as an owner of an appliances store and performing his hobbies like sailing and playing darts.
Posterior dislocation of the shoulder may occur during a seizure when sustained contraction of internal rotators overcomes the weak external rotators.2 The anterior musculature spasm pulls the humerus back against the glenoid, creating a compression fracture.1 Patients with a posterior dislocated shoulder complain of pain and inability to exorotate the shoulder. Typical clinical presentation includes the patient holding his arm in internal rotation in the adducted position. There is an increased prominence of the coracoid process anteriorly and of the humeral head posteriorly.4,5 On plain anteroposterior radiographs posterior dislocation of the shoulder can be seen as an inability to look between the humeral head and the glenoid, and the ratio of head to glenoid is abnormal caused by the dislocated head being closer to the radiography plate.6 It can be difficult to detect a posterior dislocation of the glenohumeral joint on plain anteroposterior radiographs; therefore the diagnosis is usually delayed.7
Numerous orthopaedic injuries caused by a direct trauma or as consequences of the seizure itself can follow a seizure. These injuries are often diagnosed late.8 Posterior dislocation fracture of the shoulders is a very rare condition and in 50-80% of all cases only recognized after initial assessment.2,3 Although muscle pain in the shoulder region is often seen after a seizure with tonic-clonic, the necessity for an accurate examination and imaging in patient complaining of discomfort and weakness in the shoulders following a seizure is evident.8 A review by Kontakis et al.9 states that whereas there is no strong clinical evidence to support the theory of early treatment, this is nonetheless preferable for there is evidence that early treatment results in less pain and possibly less complications. Immediate treatment is advocated by most to prevent avascular necrosis of the humeral head.10 In literature there is no consensus considering the best course and type of treatment for complicated fractures like our patient’s.
In our case both shoulders were posteriorly dislocated and the fractures were comminuted in such a way that large parts of the humeral heads hooked behind the glenoid. It was not found until the second day after presentation. Preoperative imaging proved to be inadequate and contributed to the failure of initial surgery. This emphasizes the importance for computer tomography for adequate classification of the fracture and thus treatment.9 A hemi-arthroplasty of the shoulder is regarded as the best option in fracture dislocations.9,11 With his last surgery performed 16 months after initial presentation, it is discussable whether this patient should have received bilateral hemi-prostheses simultaneously.12,13
Although bilateral posterior fracture dislocation is a very rare injury, functional limitation of both shoulders can be devastating.14 Avoiding doctor’s delay, appropriated imaging and adequate surgical treatment can improve final functional results.
None.
The author declares that there is no conflict of interest.

©2014 Wijers, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.