MOJ
eISSN: 2374-6939


Editorial Volume 7 Issue 3
Zagazig University, Egypt
Correspondence: Khaled Mohamed Mohamed Diab, Zagazig University, Egypt, Tel +20 1015863282
Received: January 28, 2017 | Published: February 22, 2017
Citation: Diab KMM (2017) Augmentation in Primary Total Knee Arthroplasty, is it Essential? MOJ Orthop Rheumatol 7(3): 00275. DOI: 10.15406/mojor.2017.07.00275
Steady developments in the field of arthroplasty research in recent decades have led to total knee replacement becoming one of the most successful orthopedic operations. Long-term follow-up studies indicate a survival rate of at least 90% within 15 years.1,2 Primary total knee arthroplasty (TKA) using modern implants results in more than 95% good to excellent results.3
The numbers and indications of primary knee replacements are expanding, and the procedure is now being offered to younger and more active patients than in the past.4 The success of TKA depends on restoration of mechanical alignment, maintenance of the joint line, balance of ligaments and soft tissue, restoration of the function of quadriceps, achievement of a stable implant, and reconstruction of substantial amounts of bone lost using metal wedges or by stem augmentation.
To achieve good long-term biological stabilization, initial secure mechanical stability is vital. A lack of initial stability can lead to resorption of bone at the implant-tissue interface and can consequently result in loosening and failure of the prosthesis.5
Bone loss around the knee in the setting of TKA remains a difficult and challenging problem for orthopedic surgeons. Uncontained peripheral bone defect in the posteromedial tibial plateau is not an infrequent problem even in primary TKA, especially in large angular deformities.6
There have been improvements in the design of prostheses in recent years, the most important of which are the introduction of metal wedge augmentation and modular fluted stems with a variable offset, which improve the alignment and allow press-fit fixation.7-9
The benefits of modular augments lie in the simplicity of replacing the bone defect without the additional risks associated with bone grafts. In most situations involving proximal tibial reconstruction, a stemmed implant is commonly used. Modular metallic augments are being increasingly used when proximal tibial bone stock is deficient. Intramedullary stems used in conjunction with tibial metaphyseal metallic augments reduce the mechanical burden in the surrounding bone by reducing bone stresses and micromotion between the implant and the adjacent bone.10
Cameron & Jung.11 showed that the additional use of a tibial stem on its own markedly reduced the micromovements of a cementless tibial implant, especially as it affects mediolateral movement.
The use of modular tibial metal augmentations should be considered as an effective solution to severe proximal tibial bony deficiencies. The wedge allows a proper tibial cut to be made, and it helps in restoring the normal joint line. It allows fast recovery of the patient with immediate weight bearing.12
The author.13 carried out a study to present the applicability and the results of the use of augments in a group of patients with primary osteoarthritis who have a severe degree of varus deformity. Twenty-five patients (average age 69 years) who had a varus alignment of the knee of more than 20 degrees were included in this study. The mean follow-up period was 24 months. All procedures were performed using a standard technique, and a P.F.C. Sigma Knee Replacement was implanted in all cases. Rehabilitation and mobilization began on the first postoperative day assisted by a physical therapist with full weight bearing. Outcomes were evaluated using the American Knee Society Score. Results showed that the mean improvement in the postoperative arc of flexion was 33 degrees. The average Knee Society knee score.14 was 44 points preoperatively and 82 points at the final follow-up. One patient developed peroneal nerve palsy; this patient recovered after 2 months. The study concludes that the use of modular metal block augmentation devices for peripheral tibial defects could serve as a simple, rapid, and dependable technique that yields predictable results, and the inclusion of a medullary modular stem in the implant component confers greater stability for the prosthesis. There are no standards for the augmentation in primary total knee arthroplasty, and each case should be dealt with according to the degree of deformity and bony defect intraoperatively (Figure 1).
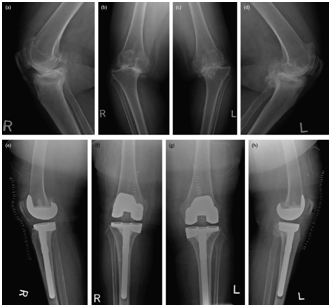
Figure 1 Case presentation for use of modular augments. (a-d) Preoperative and (e-h) postoperative anteroposterior standing view and lateral view radiographs of a 77-year-old female patient. Varus of 22° in the right knee and 20° in the left knee was observed preoperatively, which showed balanced alignment postoperatively on using a medial tibial metal wedge and a tibial stem in both knees.
None.
None.

©2017 Diab. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.